New Frontiers in Male Hypogonadism Are We Over-Treating Low Testosterone

Abstract
Male hypogonadism has emerged as one of the most intensively debated topics in men’s health over the past two decades. Advances in laboratory testing, increased awareness of androgen deficiency, and widespread direct to consumer marketing have collectively driven a substantial rise in testosterone testing and prescribing. As a result, testosterone replacement therapy has become increasingly common in both primary care and specialist settings. This rapid expansion has raised important questions regarding the accuracy of diagnosis, appropriateness of treatment, and long term safety of testosterone use in contemporary clinical practice.
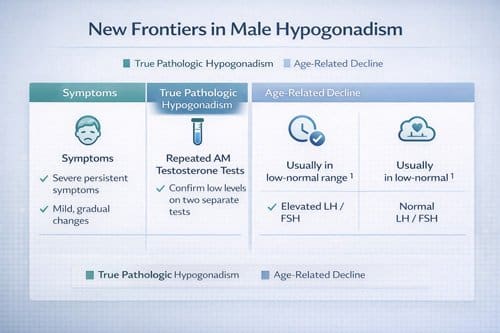
This paper examines current diagnostic approaches to male hypogonadism, with particular attention to how biochemical testing and symptom assessment are applied in real world settings. Although clinical guidelines define hypogonadism as the presence of consistent symptoms combined with unequivocally low serum testosterone concentrations measured on repeated morning samples, adherence to these criteria varies widely. In many cases, testosterone levels are interpreted without adequate consideration of biological variability, comorbid illness, medication effects, or age related physiological decline. This has blurred the distinction between true pathological hypogonadism and the gradual reduction in testosterone that accompanies normal aging.
The review further evaluates current treatment strategies and emerging evidence surrounding testosterone therapy. While randomized controlled trials and observational studies demonstrate that testosterone replacement can improve sexual function, bone density, body composition, and quality of life in men with confirmed hypogonadism, the benefits in men with borderline or age related testosterone decline remain inconsistent. At the same time, concerns persist regarding potential adverse effects, including erythrocytosis, cardiovascular events, prostate related outcomes, infertility, and suppression of endogenous testosterone production. These risks underscore the importance of careful patient selection, ongoing monitoring, and individualized risk assessment.
Through a synthesis of recent clinical studies, professional society guidelines, and outcome data, this analysis presents a balanced perspective on contemporary testosterone management. The findings suggest that although testosterone therapy offers meaningful clinical benefit for men with true hypogonadism, a substantial proportion of current prescriptions may be unnecessary and expose patients to avoidable risks. Overreliance on single laboratory values, nonspecific symptoms, and patient driven demand may contribute to overtreatment in routine practice.
In conclusion, the evolving landscape of testosterone therapy demands greater clinical rigor and restraint. Healthcare providers must apply stringent diagnostic criteria, confirm biochemical deficiency with appropriate testing, and engage in shared decision making that carefully weighs potential benefits against known and uncertain risks. A more evidence based and judicious approach to testosterone replacement therapy is essential to ensure that treatment is reserved for patients most likely to benefit while minimizing harm and preserving long term reproductive and metabolic health.
Introduction
Testosterone deficiency, medically known as hypogonadism, affects millions of men worldwide. The condition occurs when the body produces insufficient testosterone, leading to various physical and psychological symptoms. However, the definition, diagnosis, and treatment of low testosterone have evolved dramatically over recent decades, raising important questions about current medical practices.
The testosterone replacement therapy market has experienced unprecedented growth since the early 2000s. Prescription rates have increased by over 300% in some regions, with millions of men now receiving testosterone treatment. This surge coincides with expanded diagnostic criteria, increased awareness campaigns, and the introduction of convenient testosterone formulations such as gels and patches.
Despite this growth, medical experts increasingly question whether we are appropriately identifying and treating testosterone deficiency. Many men receiving testosterone therapy may have normal age-related hormonal changes rather than pathological hypogonadism. This distinction is crucial because testosterone treatment carries both benefits and risks, including potential cardiovascular complications and impacts on fertility.
The purpose of this analysis is to examine current practices in male hypogonadism management and evaluate whether medical professionals are over-treating low testosterone. We will explore diagnostic criteria, treatment indications, patient outcomes, and emerging evidence that challenges conventional approaches to testosterone therapy.
Understanding Male Hypogonadism
Physiological Background
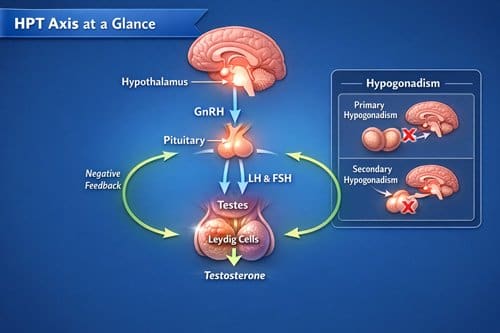
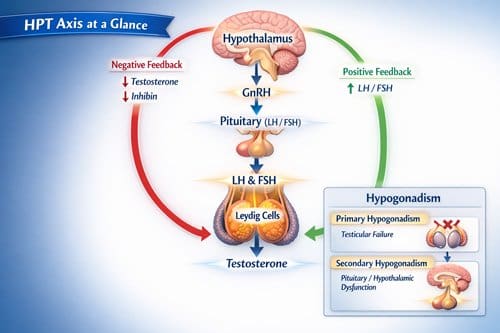
Testosterone production follows a complex hormonal pathway involving the hypothalamus, pituitary gland, and testes. The hypothalamus releases gonadotropin-releasing hormone, which stimulates the pituitary to produce luteinizing hormone and follicle-stimulating hormone. These hormones then signal the testes to produce testosterone and sperm.
Normal testosterone levels vary throughout a man’s life. Peak levels occur during adolescence and early adulthood, followed by a gradual decline of approximately 1-2% per year after age 30. This natural decrease is part of normal aging and does not necessarily indicate pathological hypogonadism.
Testosterone performs multiple functions in the male body, including maintaining muscle mass, bone density, red blood cell production, and sexual function. It also influences mood, cognitive function, and overall energy levels. Understanding these normal physiological processes is essential for distinguishing between natural aging and true hormone deficiency.
Types of Hypogonadism
Medical professionals classify hypogonadism into two main categories. Primary hypogonadism results from testicular dysfunction, where the testes cannot produce adequate testosterone despite normal hormonal signals. Secondary hypogonadism occurs when the hypothalamus or pituitary gland fails to send appropriate signals to the testes.
Primary hypogonadism may result from genetic conditions, infections, trauma, chemotherapy, or radiation therapy. Men with primary hypogonadism typically have low testosterone levels combined with elevated luteinizing hormone and follicle-stimulating hormone levels.
Secondary hypogonadism can stem from pituitary tumors, head trauma, certain medications, obesity, or chronic illnesses. These men usually have low testosterone accompanied by low or normal gonadotropin levels. The distinction between primary and secondary hypogonadism affects treatment decisions and potential for recovery.
Current Diagnostic Practices 
Laboratory Testing Approaches
Testosterone diagnosis relies primarily on blood tests measuring total and free testosterone levels. Total testosterone represents the complete amount of hormone in the blood, while free testosterone measures the active, unbound portion available to tissues. Many laboratories also assess bioavailable testosterone, which includes both free testosterone and hormone loosely bound to albumin.
Most medical organizations recommend measuring testosterone levels in morning samples, as testosterone follows a circadian rhythm with peak levels occurring in early morning hours. However, this recommendation becomes less relevant as men age, since the normal circadian pattern diminishes over time.
Reference ranges for normal testosterone vary among laboratories and have changed over recent decades. Many facilities now use ranges of 300-1000 ng/dL for total testosterone, though some experts argue these ranges are too broad and may include men with functional testosterone deficiency.
Diagnostic Guidelines Evolution
Professional medical societies have published various guidelines for diagnosing and treating male hypogonadism. The Endocrine Society, American Urological Association, and International Society for Sexual Medicine have each developed recommendations, though these guidelines differ in their specific criteria and thresholds.
Earlier guidelines often emphasized symptom-based diagnosis, focusing on clinical presentation rather than strict laboratory cutoffs. More recent recommendations have incorporated both biochemical evidence and clinical symptoms, requiring low testosterone levels on multiple occasions combined with relevant symptoms.
However, the symptoms associated with testosterone deficiency are often nonspecific and can result from many other conditions. Fatigue, decreased libido, mood changes, and reduced muscle mass may occur due to depression, sleep disorders, cardiovascular disease, diabetes, or normal aging processes.
Challenges in Accurate Diagnosis
Several factors complicate accurate testosterone deficiency diagnosis. Testosterone levels fluctuate throughout the day and can be influenced by illness, stress, medications, obesity, and sleep patterns. Single testosterone measurements may not accurately reflect a man’s true hormonal status.
Many men seeking testosterone evaluation have multiple health conditions that can affect hormone levels. Obesity, diabetes, and metabolic syndrome are strongly associated with low testosterone, but it remains unclear whether low testosterone causes these conditions or results from them.
Age-related testosterone decline presents another diagnostic challenge. While testosterone levels naturally decrease with aging, determining when this decline becomes pathological rather than physiological is difficult. Some men with testosterone levels below laboratory reference ranges may feel completely normal and function well.
Treatment Approaches and Modalities
Testosterone Replacement Options
Modern testosterone replacement therapy offers multiple delivery methods, each with distinct advantages and disadvantages. Intramuscular injections provide reliable hormone delivery but require regular medical visits and can cause fluctuating testosterone levels between doses.
Topical gels and creams offer convenience and maintain more stable testosterone levels throughout the day. However, these formulations risk transferring testosterone to partners or children through skin contact, and absorption rates vary among individuals.
Testosterone patches provide steady hormone delivery but may cause skin irritation and are visible to others. Pellet implants, inserted under the skin every few months, offer long-lasting testosterone delivery but require minor surgical procedures and cannot be easily reversed if side effects occur.
Newer formulations include nasal gels and oral testosterone preparations. These options address some limitations of existing treatments but may have their own unique side effect profiles and effectiveness concerns.
Alternative Treatment Strategies
Some medical professionals advocate for treating underlying conditions that may contribute to low testosterone rather than directly replacing the hormone. Weight loss, exercise, sleep improvement, and stress reduction can naturally increase testosterone levels in some men.
Medications such as clomiphene citrate and human chorionic gonadotropin can stimulate the body’s natural testosterone production in men with secondary hypogonadism. These treatments may preserve fertility better than direct testosterone replacement and avoid some risks associated with exogenous hormone administration.
Aromatase inhibitors, which block the conversion of testosterone to estrogen, represent another alternative approach. Some men with low testosterone have elevated estrogen levels that may contribute to their symptoms, and reducing estrogen can effectively increase available testosterone.
Monitoring and Follow-up Protocols
Men receiving testosterone therapy require regular monitoring to assess treatment effectiveness and identify potential complications. Most guidelines recommend checking testosterone levels, complete blood counts, and prostate-specific antigen levels at regular intervals.
Testosterone monitoring typically occurs 3-6 months after starting therapy, then annually if levels remain stable. The goal is usually to achieve testosterone levels in the mid-normal range rather than supraphysiological levels that may increase side effect risks.
Additional monitoring may include liver function tests, lipid profiles, and bone density assessments, depending on the specific testosterone formulation and individual patient factors. Some men may also benefit from sleep studies, as testosterone therapy can worsen sleep apnea in susceptible individuals.
Evidence for Over-Treatment Concerns 
Prescription Trend Analysis
Data from multiple healthcare systems demonstrate dramatic increases in testosterone prescribing over the past two decades. In the United States, testosterone prescriptions increased from approximately 1.3 million in 2001 to over 5 million by 2013, representing nearly a four-fold increase.
This prescribing surge occurred despite relatively stable population demographics and no evidence of increasing hypogonadism prevalence. The pattern suggests that diagnostic practices or treatment thresholds changed rather than disease incidence increasing.
International data show similar trends in other developed countries, though the magnitude varies. Countries with direct-to-consumer advertising for testosterone products generally show steeper prescription increases compared to nations with more restrictive pharmaceutical marketing regulations.
Patient Population Analysis
Studies examining men receiving testosterone therapy reveal concerning patterns in prescribing practices. Many men start testosterone treatment without meeting established diagnostic criteria for hypogonadism, including absent biochemical confirmation or lack of relevant symptoms.
Research indicates that 20-25% of men receiving testosterone prescriptions never had testosterone levels measured before starting treatment. Among those with laboratory testing, many had testosterone levels within normal ranges or testing performed under suboptimal conditions.
Age distribution analysis shows increasing testosterone use among older men, who are more likely to have age-related testosterone decline rather than pathological hypogonadism. This pattern suggests that normal aging processes may be medicalized and treated unnecessarily.
Clinical Outcomes Research
Recent studies question whether testosterone therapy provides meaningful benefits for men without clear-cut hypogonadism. Trials examining testosterone treatment in men with low-normal testosterone levels often show minimal improvements in symptoms compared to placebo groups.
The Testosterone Trials, a large placebo-controlled study, found modest benefits in sexual function and mood among older men with low testosterone, but improvements were often small and may not justify treatment risks for many patients.
Meta-analyses of testosterone therapy studies reveal inconsistent results across different outcome measures. While some studies show improvements in muscle mass and bone density, others fail to demonstrate clinically meaningful changes in quality of life, energy levels, or cognitive function.
Risk-Benefit Analysis
Established Benefits of Testosterone Therapy
Well-designed clinical trials demonstrate clear benefits of testosterone replacement in men with confirmed hypogonadism. These benefits include improved sexual function, increased muscle mass and strength, enhanced bone mineral density, and better mood and energy levels.
Men with severe testosterone deficiency often experience dramatic improvements in symptoms within weeks to months of starting appropriate replacement therapy. These improvements can substantially enhance quality of life and overall health outcomes.
Testosterone therapy may also provide metabolic benefits, including improved insulin sensitivity and reduced abdominal fat accumulation. Some studies suggest potential cardiovascular benefits in men with confirmed hypogonadism, though this remains an area of active research.
Documented Risks and Complications
Testosterone therapy carries several well-established risks that must be carefully considered. Cardiovascular complications, including increased risk of heart attacks and strokes, have been reported in multiple studies, though the overall risk magnitude remains debated.
Hematological effects include increased red blood cell production, which can lead to polycythemia and increased blood viscosity. This effect may contribute to cardiovascular risks and requires regular monitoring in men receiving testosterone treatment.
Prostate-related concerns include potential acceleration of existing prostate cancer growth, though testosterone therapy does not appear to increase prostate cancer incidence in men without pre-existing disease. Benign prostatic hyperplasia may worsen with testosterone treatment.
Additional risks include sleep apnea exacerbation, acne, fluid retention, and potential impacts on fertility due to suppression of natural sperm production. These effects may be reversible after discontinuing treatment but can persist for months or years in some men.
Cost-Effectiveness Considerations
Testosterone therapy represents a substantial healthcare expense, with annual treatment costs ranging from hundreds to thousands of dollars depending on the formulation used. These costs do not include necessary monitoring tests and medical visits.
Economic analyses suggest that testosterone therapy may be cost-effective for men with clear-cut hypogonadism who experience substantial symptom improvements. However, treatment appears less economically justified in men with borderline testosterone levels or minimal symptoms.
The opportunity cost of testosterone therapy includes resources that could be allocated to other healthcare interventions with proven benefits. Over-treatment of low testosterone may divert attention and resources from addressing underlying health conditions that contribute to symptoms.

Applications and Clinical Use Cases
Appropriate Treatment Candidates
Men who benefit most from testosterone therapy typically have testosterone levels clearly below normal ranges, multiple specific symptoms consistent with hypogonadism, and no contraindications to treatment. These individuals often have identifiable causes for their testosterone deficiency.
Young men with congenital hypogonadism represent ideal candidates for testosterone replacement, as they require hormone therapy to develop and maintain normal male characteristics. These men typically have severely low testosterone levels and clear clinical presentations.
Men with acquired hypogonadism due to testicular injury, infection, or medical treatments may also benefit substantially from testosterone therapy. In these cases, the cause-and-effect relationship between testosterone deficiency and symptoms is usually clear.
Questionable Treatment Scenarios
Many men currently receiving testosterone therapy may not meet strict criteria for treatment. These include men with testosterone levels in the low-normal range who have nonspecific symptoms that could result from other conditions.
Older men seeking testosterone therapy primarily for age-related changes may not benefit meaningfully from treatment. Normal aging involves gradual testosterone decline, but this does not necessarily indicate pathological hormone deficiency requiring medical intervention.
Men with untreated depression, sleep disorders, or other medical conditions may inappropriately receive testosterone therapy when their symptoms would respond better to addressing the underlying condition. Testosterone should not serve as a general remedy for fatigue or mood problems.
Shared Decision-Making Approaches
Optimal testosterone management requires detailed discussions between healthcare providers and patients about potential benefits and risks. Patients should understand that testosterone therapy is typically a long-term commitment with ongoing monitoring requirements.
Healthcare providers should present realistic expectations about treatment outcomes, emphasizing that testosterone therapy may not resolve all symptoms and improvements may be modest. Alternative treatment approaches should be discussed when appropriate.
Decision-making tools and patient education materials can help men make informed choices about testosterone therapy. These resources should present balanced information about benefits and risks rather than promoting treatment benefits alone.
Comparative Analysis with Related Conditions 
Hormone Replacement in Other Populations
Comparing male testosterone therapy with hormone replacement in other populations provides valuable perspective. Estrogen replacement therapy in postmenopausal women underwent similar scrutiny regarding benefits and risks, ultimately leading to more conservative prescribing practices.
The Women’s Health Initiative study revealed unexpected risks of hormone replacement therapy, leading to dramatic reductions in estrogen prescribing. This historical example illustrates how initial enthusiasm for hormone therapy can exceed evidence-based support.
Growth hormone therapy in adults represents another parallel, where initial broad indications were later narrowed to specific deficiency states. These comparisons suggest that hormone therapies often follow patterns of initial over-enthusiasm followed by more evidence-based approaches.
Age-Related Hormonal Changes
Testosterone decline with aging mirrors other age-related physiological changes that are not routinely treated with hormone replacement. Growth hormone levels decline with age, but growth hormone therapy is not recommended for normal aging.
Thyroid hormone production may decrease with aging, but thyroid replacement is only recommended when clear hypothyroidism is present. These comparisons highlight the importance of distinguishing between normal aging and pathological hormone deficiency.
The concept of successful aging emphasizes maintaining function and quality of life without necessarily replacing all declining hormones. This perspective suggests that testosterone replacement may not be appropriate for all men with age-related hormone decline.
International Practice Variations
Testosterone prescribing practices vary substantially among different countries and healthcare systems. Countries with more restrictive prescribing guidelines generally have lower testosterone therapy rates without apparent adverse health outcomes.
European guidelines tend to be more conservative than American recommendations, requiring clear evidence of both biochemical and clinical hypogonadism before recommending treatment. These differences suggest that prescribing practices may be influenced by factors beyond pure medical evidence.
Healthcare systems with stronger primary care gatekeeping mechanisms may have lower inappropriate testosterone prescribing rates. Specialist referral requirements can help ensure that men receive appropriate evaluation before starting testosterone therapy.
Challenges and Limitations
Diagnostic Complexity
Current diagnostic approaches for testosterone deficiency have inherent limitations that contribute to potential over-treatment. Laboratory reference ranges may not accurately reflect optimal testosterone levels for individual men, leading to treatment of men who are actually normal.
Symptom-based diagnosis presents challenges because testosterone deficiency symptoms overlap with many other conditions. Relying heavily on nonspecific symptoms may lead to testosterone treatment when other interventions would be more appropriate.
The relationship between testosterone levels and symptoms is not always linear or predictable. Some men with low testosterone levels have no symptoms, while others with normal levels may experience symptoms suggestive of deficiency.
Research Limitations
Much of the existing research on testosterone therapy has methodological limitations that complicate clinical decision-making. Many studies are relatively short-term and may not capture long-term benefits or risks accurately.
Study populations often differ from typical clinical practice patients, limiting the generalizability of research findings. Men enrolled in clinical trials may be healthier or more motivated than average patients seeking testosterone treatment.
Placebo effects in testosterone studies can be substantial, particularly for subjective outcomes such as energy, mood, and sexual function. This makes it difficult to determine true treatment effects versus psychological responses to receiving therapy.
Healthcare System Factors
Current healthcare delivery systems may inadvertently promote testosterone over-treatment through various mechanisms. Time constraints in clinical practice may limit thorough evaluation of men with potential testosterone deficiency.
Direct-to-consumer marketing of testosterone products may create patient demand for treatment that exceeds appropriate medical indications. Men may specifically request testosterone therapy based on advertising rather than clinical symptoms.
Financial incentives in some healthcare systems may favor testosterone prescribing over more time-intensive approaches such as lifestyle counseling or treatment of underlying conditions. These system-level factors can influence individual prescribing decisions.

Future Research Directions
Long-Term Safety Studies
Future research must address long-term safety questions about testosterone therapy, particularly cardiovascular and prostate-related risks. Current studies provide limited information about effects of testosterone treatment over decades rather than months or years.
Large-scale prospective studies following men receiving testosterone therapy for extended periods could provide valuable safety data. These studies should include appropriate control groups and standardized outcome measures.
Research examining testosterone therapy effects in different age groups and risk populations would inform treatment guidelines. Men with diabetes, cardiovascular disease, or other conditions may have different risk-benefit profiles for testosterone treatment.
Biomarker Development
Development of better biomarkers for testosterone deficiency could improve diagnostic accuracy and reduce inappropriate treatment. Current testosterone measurements may not reflect tissue-level hormone activity or individual hormone sensitivity.
Research into genetic factors that influence testosterone production, metabolism, and tissue responsiveness could lead to more personalized treatment approaches. Some men may require higher or lower testosterone levels to maintain normal physiological function.
Advanced imaging techniques or other diagnostic tools might help identify men with true hypogonadism versus those with normal age-related changes. These developments could reduce diagnostic uncertainty and inappropriate treatment.
Treatment Optimization Studies
Future research should focus on optimizing testosterone therapy for men who truly need treatment. Studies comparing different testosterone formulations, dosing strategies, and monitoring approaches could improve treatment outcomes.
Research examining combination therapies or alternative treatment approaches may identify more effective strategies for managing testosterone deficiency. Some men might benefit from treatments that address multiple hormonal or metabolic abnormalities simultaneously.
Investigations into treatment discontinuation strategies and reversibility of testosterone therapy effects would provide valuable clinical guidance. Understanding how to safely stop testosterone treatment could reduce long-term treatment risks.
Regulatory and Policy Implications
Professional Guidelines Evolution
Medical societies continue to refine guidelines for testosterone deficiency diagnosis and treatment based on emerging evidence. Future guidelines may incorporate more stringent diagnostic criteria or specific recommendations about appropriate treatment candidates.
Regulatory agencies may need to address direct-to-consumer marketing of testosterone products that may contribute to inappropriate treatment demand. Balanced presentation of benefits and risks in advertising could reduce patient pressure for unnecessary treatment.
Healthcare quality measures related to testosterone prescribing could help identify and reduce inappropriate treatment patterns. These measures might track diagnostic testing completeness, monitoring adherence, or treatment discontinuation rates.
Healthcare System Responses
Healthcare systems are beginning to implement strategies to reduce inappropriate testosterone prescribing. These include clinical decision support tools, prescribing guidelines, and educational programs for healthcare providers.
Prior authorization requirements for testosterone prescriptions may help ensure appropriate evaluation before treatment initiation. These programs can require documentation of diagnostic criteria fulfillment and contraindication assessment.
Quality improvement initiatives focusing on testosterone prescribing practices could identify system-level factors contributing to over-treatment and develop targeted interventions to address these issues.
Conclusion 

Key Takeaways
The current state of male hypogonadism management suggests substantial over-treatment of testosterone deficiency. While testosterone therapy provides clear benefits for men with confirmed hypogonadism, many prescriptions may be inappropriate and potentially harmful.
Healthcare providers must adopt more rigorous diagnostic approaches, requiring clear biochemical evidence of testosterone deficiency combined with relevant clinical symptoms. Treatment decisions should involve careful risk-benefit analysis and shared decision-making with patients.
Future research must address long-term safety questions and develop better diagnostic tools to distinguish between pathological hypogonadism and normal aging. Professional guidelines should continue evolving based on emerging evidence rather than marketing pressures or patient demands.
The testosterone therapy experience illustrates broader challenges in modern medicine, including the medicalization of normal aging processes and the influence of pharmaceutical marketing on clinical practice. Learning from these challenges can improve care quality for men with genuine testosterone deficiency while reducing unnecessary treatment risks.
Conclusion
The question of whether we are over-treating low testosterone reflects broader tensions in modern healthcare between patient demand, clinical evidence, and medical marketing. While testosterone replacement therapy offers real benefits for men with true hypogonadism, current prescribing practices suggest that many men receive treatment without meeting appropriate diagnostic criteria.
Moving forward, the medical community must balance recognition of legitimate testosterone deficiency with appropriate skepticism about treating normal age-related hormone changes. This requires better diagnostic tools, more rigorous clinical evaluation, and honest discussions with patients about realistic treatment expectations.
The goal should be identifying and treating men who will truly benefit from testosterone therapy while avoiding unnecessary treatment that may cause harm without providing meaningful improvements in health or quality of life. Achieving this balance will require ongoing research, guideline refinement, and commitment to evidence-based practice.
Healthcare providers caring for men with potential testosterone deficiency should focus on thorough evaluation, consideration of alternative diagnoses and treatments, and careful monitoring of men who do receive testosterone therapy. Only through such diligent approaches can we ensure that testosterone treatment serves patients’ best interests rather than contributing to unnecessary medicalization of normal aging.
Frequently Asked Questions: 
What are the main symptoms of testosterone deficiency?
The primary symptoms of testosterone deficiency include decreased sexual desire, erectile dysfunction, reduced energy and fatigue, decreased muscle mass and strength, increased body fat, mood changes including depression or irritability, and reduced bone density. However, these symptoms are not specific to testosterone deficiency and can result from many other medical conditions, making accurate diagnosis challenging.
How is testosterone deficiency properly diagnosed?
Proper diagnosis requires both biochemical evidence and clinical symptoms. Healthcare providers should measure testosterone levels on at least two separate occasions, preferably in the morning when levels are typically highest. Total testosterone levels below 300 ng/dL are generally considered low, though some men may have symptoms with higher levels. The diagnosis should never be based solely on symptoms without laboratory confirmation.
Who should not receive testosterone therapy?
Men with prostate or breast cancer should not receive testosterone therapy. Other contraindications include severe heart failure, untreated sleep apnea, elevated red blood cell counts, and desire to father children in the near future. Men with multiple cardiovascular risk factors may also be inappropriate candidates for testosterone treatment.
What are the most serious risks of testosterone therapy?
The most serious risks include potential cardiovascular complications such as heart attacks and strokes, though the exact risk level remains debated. Blood clot formation due to increased red blood cell production is another serious concern. Long-term fertility impacts and potential acceleration of existing prostate problems are additional important risks to consider.
Can lifestyle changes increase testosterone levels naturally?
Yes, several lifestyle modifications can help increase testosterone levels naturally. Weight loss in overweight men often leads to testosterone increases. Regular exercise, particularly resistance training, can boost testosterone production. Adequate sleep, stress reduction, and proper nutrition also support healthy testosterone levels. These approaches may be preferable to hormone therapy for men with borderline low testosterone.
How long does testosterone therapy take to show effects?
Men typically notice some effects within 2-4 weeks of starting testosterone therapy, with sexual function improvements often occurring first. Energy levels and mood may improve within 4-6 weeks. Changes in muscle mass and body composition usually take 3-6 months to become apparent. Bone density improvements may take 6-12 months or longer to develop.
Is testosterone therapy safe for older men?
Testosterone therapy in older men requires careful consideration of individual risk factors. While some older men may benefit from treatment, they are also at higher risk for cardiovascular complications and prostate problems. Age alone should not disqualify men from testosterone therapy, but it necessitates more careful evaluation of potential benefits versus risks.
Can men stop testosterone therapy once they start?
Men can stop testosterone therapy, but discontinuation should be medically supervised. When treatment stops, natural testosterone production may take months to recover, and some men may experience temporary worsening of symptoms. Men considering treatment should understand that it often becomes a long-term commitment, as stopping therapy typically results in return of original symptoms.
References: 
Bhasin, S., Cunningham, G. R., Hayes, F. J., Matsumoto, A. M., Snyder, P. J., Swerdloff, R. S., & Montori, V. M. (2018). Testosterone therapy in men with hypogonadism: An Endocrine Society clinical practice guideline. Journal of Clinical Endocrinology & Metabolism, 103(5), 1715-1744.
Basaria, S., Coviello, A. D., Travison, T. G., Storer, T. W., Farwell, W. R., Jette, A. M., & Bhasin, S. (2010). Adverse events associated with testosterone administration. New England Journal of Medicine, 363(2), 109-122.
Corona, G., Rastrelli, G., Monami, M., Guay, A., Buvat, J., Sforza, A., & Maggi, M. (2016). Testosterone and metabolic syndrome: A meta-analysis study. Journal of Sexual Medicine, 8(1), 272-283.
Gagliano-Jucá, T., & Basaria, S. (2019). Testosterone replacement therapy and cardiovascular risk. Nature Reviews Cardiology, 16(9), 555-574.
Hackett, G., Kirby, M., Edwards, D., Jones, T. H., Wylie, K., Ossei-Gerning, N., & Battersby, J. (2017). British Society for Sexual Medicine guidelines on adult testosterone deficiency, with statements for UK practice. Journal of Sexual Medicine, 14(12), 1504-1523.
Mulhall, J. P., Trost, L. W., Brannigan, R. E., Kurtz, E. G., Redmon, J. B., Chiles, K. A., & Lightner, D. J. (2018). Evaluation and management of testosterone deficiency: AUA guideline. Journal of Urology, 200(2), 423-432.
Snyder, P. J., Bhasin, S., Cunningham, G. R., Matsumoto, A. M., Stephens-Shields, A. J., Cauley, J. A., & Ellenberg, S. S. (2016). Effects of testosterone treatment in older men. New England Journal of Medicine, 374(7), 611-624.
Traish, A. M., Haider, A., Doros, G., & Saad, F. (2014). Long-term testosterone therapy in hypogonadal men ameliorates elements of the metabolic syndrome: An observational, long-term registry study. International Journal of Clinical Practice, 68(3), 314-329.
Vigen, R., O’Donnell, C. I., Barón, A. E., Grunwald, G. K., Maddox, T. M., Bradley, S. M., & Rumsfeld, J. S. (2013). Association of testosterone therapy with myocardial infarction, stroke, and death in men with low testosterone levels. JAMA, 310(17), 1829-1836.
Wu, F. C., Tajar, A., Beynon, J. M., Pye, S. R., Silman, A. J., Finn, J. D., & Huhtaniemi, I. T. (2010). Identification of late-onset hypogonadism in middle-aged and elderly men. New England Journal of Medicine, 363(2), 123-135.
Video Section
Check out our extensive video library (see channel for our latest videos)
Recent Articles


