The Great Vitamin D Debate Optimal Levels, Supplementation, and Clinical Outcomes
Abstract
Vitamin D deficiency is among the most common nutritional disorders globally, affecting an estimated one billion individuals across a wide range of ages, ethnicities, and geographic regions. Contributing factors include limited sunlight exposure, skin pigmentation, dietary insufficiency, obesity, aging, and certain chronic medical conditions. Given the widespread prevalence of deficiency and the biological role of vitamin D in calcium homeostasis, skeletal integrity, immune function, and cellular regulation, its clinical significance has become a major focus of research and debate in contemporary medicine.
This paper critically examines current evidence regarding optimal serum vitamin D concentrations, appropriate supplementation strategies, and their associated clinical outcomes. Despite decades of investigation, there remains substantial disagreement among healthcare professionals regarding what constitutes vitamin D sufficiency, how aggressively deficiency should be corrected, and which patient populations are most likely to benefit from supplementation. Target serum 25 hydroxyvitamin D thresholds vary across guidelines, with differing definitions of deficiency, insufficiency, and optimal levels contributing to inconsistent clinical practice.
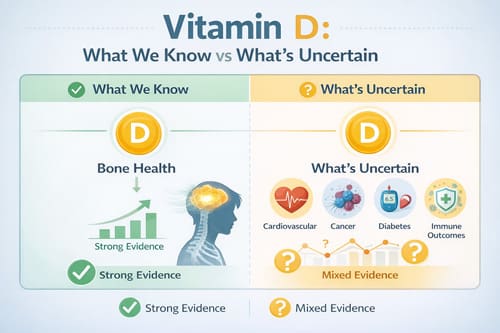
Recent large scale randomized controlled trials have further complicated the landscape by challenging long held assumptions about the broader health benefits of vitamin D supplementation. While observational studies have historically linked low vitamin D levels to increased risk of cardiovascular disease, malignancy, diabetes, and immune mediated conditions, interventional trials have often failed to demonstrate consistent reductions in these outcomes with routine supplementation in generally healthy populations. These findings have prompted a reassessment of vitamin D’s role beyond bone and mineral metabolism and raised important questions about causality, baseline deficiency status, and trial design.
In contrast, the benefits of vitamin D for bone health remain well established. Adequate vitamin D levels are essential for calcium absorption, prevention of osteomalacia, and reduction of fracture risk when combined with appropriate calcium intake in at risk populations. Emerging evidence also suggests that vitamin D may exert context dependent effects on immune function, muscle strength, and inflammatory pathways, although these relationships appear to be more nuanced than previously assumed and may vary based on individual patient characteristics.
This review synthesizes current clinical guidelines from major medical organizations, including differing recommendations on screening, supplementation thresholds, and dosing regimens. It also evaluates evidence from recent randomized trials and meta analyses to clarify where vitamin D supplementation provides clear benefit and where expectations should be tempered. Finally, the paper offers practical, evidence informed recommendations for clinicians managing patients with varying vitamin D status, emphasizing individualized risk assessment, appropriate dosing, and realistic counseling regarding anticipated health outcomes. By integrating evolving evidence with clinical pragmatism, this analysis aims to support more consistent and rational use of vitamin D in everyday practice.
Introduction
Vitamin D has transitioned from being viewed primarily as a nutrient essential for bone health to a hormone like compound with potential biological effects across multiple organ systems. The identification of vitamin D receptors in a wide range of tissues, including the immune system, cardiovascular system, endocrine organs, and central nervous system, has driven extensive research into its broader physiological and clinical roles. As a result, healthcare providers are increasingly confronted with complex decisions regarding vitamin D screening, interpretation of serum levels, supplementation strategies, and long term monitoring.
Over the past two decades, recommendations surrounding vitamin D have undergone several significant shifts. Initial observational studies suggested strong associations between low vitamin D levels and a wide array of adverse health outcomes, including cardiovascular disease, malignancy, autoimmune disorders, and increased mortality. These findings fueled widespread enthusiasm for routine screening and high dose supplementation, often with the aim of achieving serum 25 hydroxyvitamin D concentrations well above traditional thresholds. However, subsequent large scale randomized controlled trials have failed to consistently demonstrate the anticipated benefits of vitamin D supplementation for many of these non skeletal outcomes. The absence of clear reductions in cardiovascular events, cancer incidence, or all cause mortality has prompted a critical reassessment of earlier assumptions and highlighted the limitations of extrapolating causality from observational data.
This evolving evidence base has contributed to substantial variability in clinical practice. Some clinicians continue to advocate for aggressive supplementation strategies, targeting serum levels above 40 ng/mL, based on perceived extraskeletal benefits or theoretical advantages. In contrast, others adhere to more conservative targets in the range of 20 to 30 ng/mL, aligning with thresholds recommended by several professional societies for maintaining bone health and preventing deficiency. This divergence reflects ongoing uncertainty regarding the definition of optimal vitamin D status, the clinical significance of marginal insufficiency, and the balance between potential benefits and risks associated with higher serum concentrations.
Accurate assessment and management of vitamin D status require an appreciation of the complex interplay between biological, environmental, and patient specific factors. Vitamin D synthesis and metabolism are influenced by geographic latitude, seasonal variation in ultraviolet exposure, skin pigmentation, age, body composition, dietary intake, supplement use, and comorbid conditions affecting absorption or metabolism. In addition, variability in laboratory assays and measurement techniques further complicates interpretation of serum 25 hydroxyvitamin D levels, contributing to inconsistent study findings and clinical uncertainty.
In this context, a nuanced and individualized approach to vitamin D management is increasingly recognized as essential. Rather than uniform screening and supplementation, clinicians must integrate current evidence, guideline recommendations, and patient specific risk factors when making decisions about testing and treatment. Ongoing research aimed at clarifying dose response relationships, identifying subpopulations most likely to benefit from supplementation, and refining clinical endpoints will be critical to resolving persistent controversies and optimizing vitamin D use in modern medical practice.

Vitamin D Metabolism and Physiology
Vitamin D exists in two primary forms: vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Vitamin D3 is synthesized in the skin through ultraviolet B radiation exposure or obtained through dietary sources and supplements. The conversion process begins when 7-dehydrocholesterol in the skin is converted to previtamin D3, which then undergoes thermal isomerization to form vitamin D3.
Following synthesis or ingestion, vitamin D undergoes hydroxylation in the liver to form 25-hydroxyvitamin D [25(OH)D], the major circulating form and standard biomarker for vitamin D status. This metabolite has a half-life of approximately 2-3 weeks, making it suitable for assessing vitamin D status over time. The final activation step occurs primarily in the kidneys, where 1α-hydroxylase converts 25(OH)D to the active hormone 1,25-dihydroxyvitamin D [1,25(OH)2D].
The active hormone binds to vitamin D receptors found in virtually all tissues, regulating gene expression through interaction with vitamin D response elements. This mechanism explains the wide-ranging potential effects of vitamin D beyond its classical role in calcium homeostasis. Additionally, many tissues express 1α-hydroxylase locally, allowing for tissue-specific production of active vitamin D.
Regulation of vitamin D metabolism involves complex feedback mechanisms. Parathyroid hormone (PTH) stimulates 1α-hydroxylase activity when calcium levels are low, increasing production of active vitamin D. Conversely, high levels of 1,25(OH)2D stimulate 24-hydroxylase, which initiates the degradation pathway. Fibroblast growth factor 23 (FGF23) also plays a crucial role in regulation, particularly in response to phosphate levels.
Measurement and Laboratory Considerations 
Accurate measurement of vitamin D status relies primarily on serum 25(OH)D concentrations. However, laboratory methods vary substantially, contributing to confusion about optimal levels and clinical interpretation. The most common assays include immunoassays and liquid chromatography-tandem mass spectrometry (LC-MS/MS).
Immunoassays, while widely available and cost-effective, may have issues with specificity and accuracy. Cross-reactivity with other metabolites and variable performance across different platforms can lead to inconsistent results. LC-MS/MS methods are considered the gold standard due to superior accuracy and precision, but they require specialized equipment and expertise.
Standardization efforts have improved laboratory consistency, but variation still exists. The Vitamin D Standardization Program, led by the National Institute of Standards and Technology, has worked to standardize reference materials and improve assay accuracy. Healthcare providers should be aware of their laboratory’s methodology and potential limitations when interpreting results.
Seasonal variation in vitamin D levels presents another consideration for measurement timing. In temperate climates, levels typically peak in late summer and reach their lowest point in late winter or early spring. This variation can be substantial, with differences of 10-20 ng/mL (25-50 nmol/L) between peak and trough levels.
Individual factors affecting vitamin D levels include age, body mass index, skin pigmentation, sunscreen use, geographic location, and dietary intake. Older adults have reduced capacity for cutaneous vitamin D synthesis, while individuals with darker skin pigmentation require more ultraviolet exposure to produce equivalent amounts of vitamin D.
Current Guidelines and Recommendations
Major medical organizations have developed varying recommendations for vitamin D intake and target serum levels. The Institute of Medicine (now National Academy of Medicine) established Recommended Dietary Allowances (RDA) of 600 IU daily for adults under 70 years and 800 IU daily for those over 70 years. These recommendations target maintenance of serum 25(OH)D levels above 20 ng/mL (50 nmol/L).
The Endocrine Society has advocated for higher targets, recommending maintenance of serum 25(OH)D levels above 30 ng/mL (75 nmol/L) and suggesting daily intakes of 1,500-2,000 IU for adults. This more aggressive approach reflects beliefs about vitamin D’s role in non-skeletal health outcomes.
International guidelines vary considerably. The European Food Safety Authority recommends 600 IU daily for adults, while some Nordic countries suggest higher intakes due to limited sun exposure. The variation in recommendations reflects different interpretations of available evidence and varying emphasis on potential non-skeletal benefits.
Clinical practice guidelines from specialty organizations add another layer of complexity. The American Association of Clinical Endocrinologists recommends targeting 25(OH)D levels between 30-50 ng/mL (75-125 nmol/L), while the American Geriatrics Society suggests 30 ng/mL (75 nmol/L) as a minimum target for older adults.
The lack of consensus among guidelines creates challenges for healthcare providers and contributes to practice variation. Some practitioners adopt conservative approaches based on established bone health benefits, while others pursue more aggressive supplementation based on theoretical benefits for other health outcomes.
Evidence from Recent Clinical Trials 
Large-scale randomized controlled trials have provided crucial evidence about vitamin D supplementation effects on various health outcomes. The VITAL trial, published in 2019, randomized over 25,000 participants to receive vitamin D3 2,000 IU daily or placebo for a median of 5.3 years. The primary endpoints were cardiovascular disease and cancer incidence.
Results from VITAL showed no reduction in the primary endpoints of major cardiovascular events or invasive cancer. However, secondary analyses suggested potential benefits in specific subgroups, including reduced cancer mortality and possible cardiovascular benefits in participants with lower baseline vitamin D levels.
The D2d trial examined vitamin D supplementation for diabetes prevention in adults with prediabetes. Participants received 4,000 IU daily of vitamin D3 or placebo for a mean of 2.5 years. Despite achieving substantial increases in serum 25(OH)D levels, vitamin D supplementation did not reduce diabetes incidence compared to placebo.
Meta-analyses of vitamin D supplementation trials have generally shown modest or no effects on most non-skeletal outcomes. However, some evidence suggests potential benefits for respiratory tract infections, particularly in individuals with severe vitamin D deficiency. The clinical importance of these findings remains debated.
The ViDA trial from New Zealand randomized over 5,000 participants to receive monthly vitamin D3 100,000 IU or placebo for a median of 3.3 years. This trial found no reduction in cardiovascular disease, fractures, or respiratory infections, despite achieving target 25(OH)D levels above 20 ng/mL in most participants.
Skeletal Health Outcomes
The relationship between vitamin D and bone health represents the most established clinical application. Vitamin D deficiency leads to impaired calcium absorption, secondary hyperparathyroidism, and eventual bone demineralization. Severe deficiency causes rickets in children and osteomalacia in adults.
Evidence for vitamin D’s role in fracture prevention is strongest when combined with adequate calcium intake. Meta-analyses of randomized trials have shown modest reductions in fracture risk, particularly hip fractures, among older adults receiving vitamin D supplementation. However, benefits appear most pronounced in populations with baseline deficiency.
The relationship between serum 25(OH)D levels and bone mineral density is complex and may not be linear. Some studies suggest threshold effects, with benefits plateauing once adequate levels are achieved. Very high levels do not appear to provide additional skeletal benefits and may potentially increase fracture risk.
PTH levels provide additional insights into vitamin D adequacy from a bone health perspective. PTH concentrations typically stabilize when 25(OH)D levels reach approximately 20-30 ng/mL (50-75 nmol/L), suggesting this range may be adequate for calcium homeostasis and bone health.
Fall prevention represents another important skeletal health outcome potentially influenced by vitamin D status. Some studies have suggested that vitamin D supplementation may reduce fall risk through effects on muscle strength and balance. However, results have been inconsistent, and benefits may be limited to specific populations or dosing regimens.

Cardiovascular Disease and Mortality
Early observational studies suggested inverse relationships between vitamin D status and cardiovascular disease risk. These findings generated considerable enthusiasm for vitamin D supplementation as a cardiovascular disease prevention strategy. However, results from randomized controlled trials have been largely disappointing.
The VITAL trial found no reduction in major adverse cardiovascular events among participants receiving 2,000 IU daily of vitamin D3. Similarly, other large trials have failed to demonstrate cardiovascular benefits of vitamin D supplementation in general populations.
Some studies have suggested potential benefits in specific subgroups, particularly individuals with very low baseline vitamin D levels or certain ethnic groups. However, these findings require confirmation in dedicated trials before influencing clinical practice recommendations.
All-cause mortality represents an important endpoint for evaluating vitamin D supplementation benefits. Meta-analyses have suggested modest reductions in mortality risk associated with vitamin D supplementation, but individual trials have generally not shown statistically significant effects.
The disconnect between observational studies and randomized trials may reflect confounding factors in observational research. Vitamin D status may serve as a marker for overall health status rather than a direct causal factor for cardiovascular outcomes.
Cancer Prevention and Outcomes 
Observational studies have suggested inverse relationships between vitamin D status and cancer incidence, particularly colorectal cancer. These findings led to hypotheses that vitamin D supplementation might reduce cancer risk through effects on cell differentiation, apoptosis, and immune function.
The VITAL trial assessed cancer incidence as a primary endpoint but found no reduction in invasive cancer among participants receiving vitamin D supplementation. However, secondary analyses suggested potential reductions in cancer mortality, particularly after excluding the first two years of follow-up.
Colorectal cancer has received particular attention due to consistent observational evidence and plausible biological mechanisms. Some randomized trials have suggested modest benefits, but results have not been uniform across studies.
Laboratory and preclinical studies have identified multiple mechanisms by which vitamin D might influence cancer development and progression. These include effects on cell cycle regulation, immune function, and angiogenesis. However, translating these mechanisms into clinical benefits has proven challenging.
The timing and duration of vitamin D supplementation may influence cancer outcomes. Some researchers have hypothesized that longer treatment periods or higher doses might be necessary to observe benefits in cancer prevention trials.
Immune Function and Respiratory Health
Vitamin D’s role in immune function has received increased attention, particularly following the COVID-19 pandemic. Vitamin D receptors are present on most immune cells, and active vitamin D modulates both innate and adaptive immune responses.
Observational studies have suggested associations between vitamin D deficiency and increased susceptibility to respiratory tract infections. Some randomized trials have shown modest reductions in acute respiratory infections among individuals receiving vitamin D supplementation, particularly those with baseline deficiency.
Meta-analyses have suggested that daily or weekly vitamin D supplementation may reduce respiratory tract infection risk more effectively than large monthly doses. This finding has implications for optimal dosing strategies and may reflect the importance of maintaining stable vitamin D levels.
The COVID-19 pandemic prompted intense interest in vitamin D’s potential protective effects. Observational studies showed associations between vitamin D deficiency and increased COVID-19 severity, but randomized controlled trials have provided mixed results regarding supplementation benefits.
Autoimmune diseases represent another area of interest for vitamin D research. Some studies have suggested that vitamin D supplementation might reduce risk of autoimmune conditions or improve outcomes in established disease. However, evidence remains preliminary and requires further investigation.
Clinical Applications and Use Cases
Healthcare providers encounter vitamin D-related decisions across diverse clinical scenarios. Routine screening remains controversial, with some organizations recommending targeted screening of high-risk populations rather than universal assessment.
High-risk groups for vitamin D deficiency include older adults, individuals with limited sun exposure, those with darker skin pigmentation living at higher latitudes, patients with malabsorption disorders, and individuals taking medications that interfere with vitamin D metabolism.
Treatment of vitamin D deficiency typically involves higher initial doses followed by maintenance therapy. Common approaches include weekly doses of 50,000 IU for 6-8 weeks, followed by daily maintenance doses of 1,000-2,000 IU. However, optimal treatment regimens remain debated.
Monitoring during treatment depends on clinical circumstances and baseline deficiency severity. Patients with severe deficiency or malabsorption may require more frequent monitoring, while healthy individuals with mild deficiency may need less intensive follow-up.
Special populations require individualized approaches. Pregnant women need adequate vitamin D for fetal development, while older adults may require higher doses due to reduced synthesis capacity and increased needs for bone health.
Comparison with Related Nutrients
Vitamin D works synergistically with other nutrients, particularly calcium, magnesium, and vitamin K. Understanding these interactions is crucial for optimizing patient outcomes and avoiding potential complications.
Calcium intake affects vitamin D requirements and vice versa. Adequate vitamin D is necessary for optimal calcium absorption, while adequate calcium intake may influence vitamin D metabolism and bone health outcomes. Most clinical trials of vitamin D for bone health have included calcium supplementation.
Magnesium plays essential roles in vitamin D metabolism, serving as a cofactor for enzymes involved in vitamin D activation and degradation. Magnesium deficiency may impair vitamin D metabolism and contribute to vitamin D resistance.
Vitamin K, particularly vitamin K2, works with vitamin D to regulate calcium deposition in bones and soft tissues. Some researchers have suggested that vitamin D supplementation without adequate vitamin K might lead to inappropriate calcium deposition in arteries and soft tissues.
The concept of nutritional cofactors has led some practitioners to recommend combined supplements containing vitamin D along with related nutrients. However, evidence supporting specific combinations remains limited.
Challenges and Limitations
Several challenges complicate vitamin D research and clinical practice. Ethical considerations make it difficult to conduct long-term placebo-controlled trials in populations with severe vitamin D deficiency, potentially limiting our understanding of treatment benefits.
Baseline vitamin D status varies widely among study populations, making it difficult to compare results across trials. Studies conducted in populations with adequate baseline levels may not detect benefits that would be apparent in deficient populations.
Seasonal variation and geographic differences in vitamin D status create additional complexity for research interpretation. Trials conducted in different locations or seasons may yield different results due to varying baseline vitamin D status and sun exposure patterns.
Individual genetic variations affect vitamin D metabolism and may influence optimal levels and supplementation requirements. Polymorphisms in genes encoding vitamin D binding protein, vitamin D receptors, and metabolic enzymes contribute to inter-individual differences in vitamin D status and response to supplementation.
The optimal biomarker for vitamin D status remains debated. While 25(OH)D is widely used, some researchers have suggested that other measures, such as bioavailable vitamin D or vitamin D binding protein levels, might provide better assessments of vitamin D adequacy.
Safety Considerations and Toxicity
Vitamin D toxicity, while rare, can occur with excessive supplementation. Toxicity typically results from prolonged intake of very high doses rather than acute overdose. The tolerable upper intake level for vitamin D is set at 4,000 IU daily for adults.
Hypercalcemia represents the primary manifestation of vitamin D toxicity, resulting from excessive calcium absorption. Symptoms may include nausea, vomiting, weakness, and kidney problems. Severe cases can lead to cardiac arrhythmias and other serious complications.
Hypercalciuria (excessive calcium excretion in urine) may occur before overt hypercalcemia develops. Some individuals appear more susceptible to hypercalciuria with vitamin D supplementation, particularly those with certain genetic variants or underlying conditions.
The relationship between vitamin D levels and toxicity risk is not precisely defined. Most cases of toxicity have occurred with serum 25(OH)D levels above 150 ng/mL (375 nmol/L), but individual susceptibility varies.
Drug interactions may increase toxicity risk. Thiazide diuretics, calcium channel blockers, and other medications can affect calcium metabolism and potentially increase the risk of hypercalcemia in patients taking vitamin D supplements.
Future Research Directions
Several areas require additional research to resolve ongoing controversies and optimize clinical practice. Long-term studies of vitamin D supplementation effects on various health outcomes are needed, particularly in populations with baseline deficiency.
Personalized approaches to vitamin D supplementation based on genetic factors, baseline status, and individual characteristics represent an important research frontier. Understanding which patients are most likely to benefit from supplementation could improve clinical outcomes and resource utilization.
Optimal dosing strategies require further investigation. Questions remain about the relative benefits of daily versus intermittent dosing, appropriate doses for different populations, and target serum levels for various health outcomes.
The role of vitamin D in emerging health areas, including mental health, cognitive function, and metabolic disorders, warrants continued investigation. These areas show promise but require more definitive evidence from well-designed clinical trials.
Novel biomarkers for assessing vitamin D status and predicting response to supplementation may improve clinical decision-making. Research into vitamin D binding protein, bioavailable vitamin D, and other markers could provide better tools for patient management.
Practical Clinical Recommendations
Based on current evidence, healthcare providers should focus on populations most likely to benefit from vitamin D assessment and supplementation. Routine screening of asymptomatic individuals with low risk factors is generally not recommended, while targeted screening of high-risk populations is more appropriate.
For patients with documented vitamin D deficiency, treatment should focus on achieving and maintaining adequate levels for bone health. Target levels of 20-30 ng/mL (50-75 nmol/L) appear adequate for most individuals, though some patients may benefit from higher levels.
Supplementation strategies should consider patient preferences, adherence factors, and clinical circumstances. Daily dosing may provide more stable levels than intermittent high-dose regimens, but both approaches can be effective when used appropriately.
Monitoring requirements depend on clinical circumstances and treatment response. Patients with severe deficiency, malabsorption, or other complicating factors may require more frequent monitoring than healthy individuals with mild deficiency.
Patient education about realistic expectations from vitamin D supplementation is crucial. While benefits for bone health are well-established, patients should understand that evidence for other health benefits remains limited and that supplementation is not a panacea for multiple health conditions.

Conclusion 

Key Takeaways
The vitamin D debate continues to evolve as new evidence emerges from clinical trials and observational studies. While enthusiasm for high-dose supplementation has been tempered by recent trial results, vitamin D remains important for bone health and may have benefits for specific populations.
Healthcare providers should focus on evidence-based approaches to vitamin D management, emphasizing established benefits for skeletal health while maintaining realistic expectations about other potential effects. Individualized assessment and treatment strategies are preferable to universal supplementation approaches.
The field would benefit from continued research into optimal dosing strategies, target populations most likely to benefit, and biomarkers for assessing vitamin D adequacy. Until more definitive evidence emerges, conservative approaches targeting established benefits represent the most prudent clinical strategy.
Patient education and shared decision-making should guide vitamin D management decisions. Providers should discuss the evidence for various health outcomes, potential benefits and risks of supplementation, and individual factors that might influence optimal approaches.
Conclusion
The vitamin D debate reflects the complexity of translating basic science discoveries into clinical practice recommendations. While initial enthusiasm for vitamin D supplementation was based on compelling observational evidence and biological plausibility, results from large randomized controlled trials have provided a more nuanced picture of vitamin D’s health effects.
Current evidence strongly supports vitamin D’s role in bone health and calcium homeostasis. Benefits for fracture prevention, particularly when combined with adequate calcium intake, justify supplementation in populations at risk for deficiency. However, evidence for cardiovascular disease prevention, cancer reduction, and other non-skeletal outcomes remains limited.
Healthcare providers should adopt evidence-based approaches that focus on established benefits while avoiding unsubstantiated claims about vitamin D’s effects. Targeted assessment and treatment of high-risk populations represents a more rational approach than universal supplementation or screening.
The field continues to evolve as researchers investigate optimal dosing strategies, identify populations most likely to benefit, and explore potential applications in emerging health areas. Future research should address remaining questions about personalized supplementation approaches and long-term effects of different vitamin D levels.
Clinical practice should emphasize patient education, shared decision-making, and realistic expectations about vitamin D supplementation benefits. While vitamin D represents an important nutrient with established health benefits, it should not be viewed as a cure-all for multiple health conditions.
Frequently Asked Questions: 
What is the optimal vitamin D level for most adults?
Most medical organizations recommend maintaining serum 25(OH)D levels above 20 ng/mL (50 nmol/L) for bone health. Some experts suggest targeting 30 ng/mL (75 nmol/L), though evidence for additional benefits at higher levels remains limited. Individual needs may vary based on age, health status, and other factors.
How much vitamin D should I take daily?
Daily vitamin D requirements vary by individual circumstances. General recommendations range from 600-800 IU daily for healthy adults, though many people require 1,000-2,000 IU daily to maintain adequate levels. People with deficiency may need higher initial doses followed by maintenance therapy.
Should everyone be screened for vitamin D deficiency?
Routine screening of healthy, low-risk individuals is generally not recommended. Targeted screening is more appropriate for high-risk groups including older adults, people with limited sun exposure, individuals with darker skin pigmentation in northern climates, and those with malabsorption disorders.
Can vitamin D supplementation prevent heart disease or cancer?
Current evidence from large randomized trials does not support vitamin D supplementation for preventing heart disease or cancer in general populations. While some studies suggest modest benefits in specific subgroups, these findings require confirmation before influencing clinical recommendations.
What are the signs of vitamin D toxicity?
Vitamin D toxicity is rare but can cause hypercalcemia leading to nausea, vomiting, weakness, and kidney problems. Toxicity typically occurs with very high supplement doses over extended periods. Most adults can safely take up to 4,000 IU daily without toxicity concerns.
Is it better to take vitamin D daily or weekly?
Daily dosing may provide more stable vitamin D levels than weekly or monthly high-dose regimens. However, both approaches can be effective when used appropriately. Daily dosing may be preferable for maintenance therapy, while weekly dosing might be used for initial treatment of deficiency.
Do I need to take vitamin D with other nutrients?
Vitamin D works with calcium, magnesium, and vitamin K for optimal bone health. While taking vitamin D alone can be beneficial, ensuring adequate intake of these related nutrients may optimize outcomes. Most people can meet these needs through diet and targeted supplementation if necessary.
How long does it take to correct vitamin D deficiency?
Correction of vitamin D deficiency typically takes 6-12 weeks with appropriate supplementation. Severe deficiency may require longer treatment periods. Follow-up testing after 2-3 months of treatment can help assess response and guide ongoing management.
References: 
- Autier, P., Boniol, M., Pizot, C., & Mullie, P. (2014). Vitamin D status and ill health: A systematic review. Lancet Diabetes & Endocrinology, 2(1), 76-89.
- Bolland, M. J., Grey, A., Gamble, G. D., & Reid, I. R. (2014). Vitamin D supplementation and falls: A trial sequential meta-analysis. Lancet Diabetes & Endocrinology, 2(7), 573-580.
- Bouillon, R., Marcocci, C., Carmeliet, G., Bikle, D., White, J. H., Dawson-Hughes, B., … & Thacher, T. (2019). Skeletal and extraskeletal actions of vitamin D: Current evidence and outstanding questions. Endocrine Reviews, 40(4), 1109-1151.
- Burt, L. A., Billington, E. O., Rose, M. S., Raymond, D. A., Hanley, D. A., & Boyd, S. K. (2019). Effect of high-dose vitamin D supplementation on volumetric bone density and bone strength: A randomized clinical trial. JAMA, 322(8), 736-745.
- Dawson-Hughes, B., Staten, M. A., Knowler, W. C., Nelson, J., Vickery, E. M., LeBlanc, E. S., … & Pittas, A. G. (2020). Intratrial exposure to vitamin D and new-onset diabetes among adults with prediabetes: A secondary analysis from the vitamin D and type 2 diabetes (D2d) study. Diabetes Care, 43(12), 2916-2922.
- Holick, M. F. (2017). The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention. Reviews in Endocrine and Metabolic Disorders, 18(2), 153-165.
- Institute of Medicine. (2011). Dietary reference intakes for calcium and vitamin D. Washington, DC: The National Academies Press.
- Manson, J. E., Cook, N. R., Lee, I. M., Christen, W., Bassuk, S. S., Mora, S., … & Buring, J. E. (2019). Vitamin D supplements and prevention of cancer and cardiovascular disease. New England Journal of Medicine, 380(1), 33-44.
- Martineau, A. R., Jolliffe, D. A., Hooper, R. L., Greenberg, L., Aloia, J. F., Bergman, P., … & Camargo Jr, C. A. (2017). Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ, 356, i6583.
- Pittas, A. G., Dawson-Hughes, B., Sheehan, P., Ware, J. H., Knowler, W. C., Aroda, V. R., … & D2d Research Group. (2019). Vitamin D supplementation and prevention of type 2 diabetes. New England Journal of Medicine, 381(6), 520-530.
- Ross, A. C., Manson, J. E., Abrams, S. A., Aloia, J. F., Brannon, P. M., Clinton, S. K., … & Shapses, S. A. (2011). The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: What clinicians need to know. Journal of Clinical Endocrinology & Metabolism, 96(1), 53-58.
- Scragg, R., Stewart, A. W., Waayer, D., Lawes, C. M., Toop, L., Sluyter, J., … & Camargo Jr, C. A. (2017). Effect of monthly high-dose vitamin D supplementation on cardiovascular disease in the Vitamin D Assessment Study: A randomized clinical trial. JAMA Cardiology, 2(6), 608-616.
- Sempos, C. T., Heijboer, A. C., Bikle, D. D., Bollerslev, J., Bouillon, R., Brannon, P. M., … & Zittermann, A. (2018). Vitamin D assays and the definition of hypovitaminosis D: Results from the First International Conference on Controversies in Vitamin D. British Journal of Clinical Pharmacology, 84(10), 2194-2207.
- Theodoratou, E., Tzoulaki, I., Zgaga, L., & Ioannidis, J. P. (2014). Vitamin D and multiple health outcomes: Umbrella review of systematic reviews and meta-analyses of observational studies and randomised trials. BMJ, 348, g2035.
- Weaver, C. M., Alexander, D. D., Boushey, C. J., Dawson-Hughes, B., Lappe, J. M., LeBoff, M. S., … & Wang, D. D. (2016). Calcium plus vitamin D supplementation and risk of fractures: An updated meta-analysis from the National Osteoporosis Foundation. Osteoporosis International, 27(1), 367-376.
Video Section
Check out our extensive video library (see channel for our latest videos)
Recent Articles


