Thyroid Cancer Overdiagnosis: Are We Treating What Doesn’t Need Treatment?

Abstract
Background and Purpose:
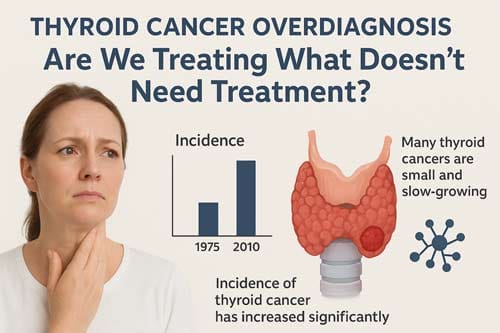
The global incidence of thyroid cancer has risen sharply over the past three decades. Data indicate that annual incidence increased from 5.0 cases per 100,000 individuals in 1975 to 14.6 cases per 100,000 in 2009 [1]. Despite this substantial increase, thyroid cancer–related mortality has remained largely unchanged. This striking discrepancy has raised concerns that the observed increase reflects overdiagnosis rather than a true surge in clinically notable disease. The purpose of this analytical review is to examine the evidence supporting thyroid cancer overdiagnosis, evaluate the drivers behind increased detection, assess the clinical consequences of aggressive treatment for low-risk tumors, and discuss evolving strategies in management that aim to address these challenges.
Methods:
A comprehensive review of the literature was performed, spanning publications from 1975 to 2024. The analysis included epidemiological studies, clinical trials on active surveillance, cost-effectiveness and economic analyses, as well as current guideline recommendations for thyroid cancer screening and management. Special attention was given to studies assessing the role of ultrasonography in detection, the outcomes of active surveillance for papillary thyroid microcarcinomas (PTMCs), and international variations in diagnostic and treatment practices.
Results:
The evidence consistently supports the existence of widespread thyroid cancer overdiagnosis, particularly of PTMCs, which are small, indolent tumors that often remain clinically silent throughout a patient’s lifetime. The sharp increase in incidence over recent decades correlates with the widespread use of neck ultrasonography and other high-resolution imaging modalities, which are capable of detecting subclinical and clinically insignificant lesions [2] [3].
Large-scale data further highlight the scope of the problem. For example, in Russia alone, it is estimated that more than 138,000 men and women were overdiagnosed with thyroid cancer within the last thirty years [4]. Similar trends have been reported globally, indicating that the majority of the rise in thyroid cancer incidence is attributable not to a true epidemic, but to improved detection of biologically indolent disease.
Clinical research has also reshaped the understanding of management options. Active surveillance has emerged as a safe and effective alternative to immediate surgical intervention for carefully selected patients with low-risk PTMCs. Multiple prospective studies have shown that these tumors exhibit minimal growth, a very low likelihood of lymph node metastasis, and no evidence of distant metastasis during surveillance periods [5]. These findings challenge the historical paradigm of routine surgery and instead support a more individualized approach that balances disease control with quality of life.
Conclusions:
Thyroid cancer overdiagnosis represents a critical issue in modern oncology, with significant implications for patients, clinicians, and healthcare systems. Advances in imaging technology have increased the detection of thyroid lesions, but this has also led to overtreatment of indolent tumors that pose little clinical risk. The current body of evidence supports more judicious use of screening, with targeted rather than population-wide approaches. Active surveillance should be considered a first-line strategy for low-risk PTMCs, provided that patients are appropriately counseled and closely monitored. Central to effective management is a patient-centered framework that emphasizes shared decision-making, ensuring that treatment decisions align with both clinical evidence and individual patient preferences.
Keywords: thyroid cancer, overdiagnosis, papillary thyroid microcarcinoma, active surveillance, screening, ultrasonography
Introduction
The landscape of thyroid cancer diagnosis and management has undergone a profound transformation over the past several decades. Global data indicate a steady and notable rise in the incidence of well-differentiated thyroid cancers, particularly papillary thyroid carcinoma. Much of this increase is attributed not to a true surge in disease prevalence but to enhanced detection of small, low-risk tumors through widespread use of high-resolution imaging technologies and more aggressive diagnostic practices. Many of these tumors are of questionable clinical significance, raising concerns about whether they represent meaningful disease or incidental findings unlikely to ever cause harm.[6] [7] This trend has sparked ongoing debate within the medical community about the appropriateness of current diagnostic thresholds, screening strategies, and treatment paradigms.
Epidemiological evidence further underscores the magnitude of the issue. Over the past decade, the incidence of thyroid cancer has risen at a rate of approximately 4.5% per year, outpacing all other malignancies. In the United States, the reported incidence reached 15.3 cases per 100,000 persons in 2013. Yet despite this striking rise in detection, thyroid cancer–specific mortality has remained largely unchanged. The discrepancy between rapidly increasing incidence and stable mortality rates is considered a defining feature of overdiagnosis, a phenomenon in which cancers are identified that would not have caused clinical symptoms, morbidity, or mortality within a patient’s natural lifespan.
The concept of overdiagnosis in thyroid cancer is not merely theoretical but carries profound consequences for patients, healthcare systems, and society. Patients diagnosed with indolent tumors are frequently subjected to overtreatment, including thyroidectomy, radioactive iodine ablation, and lifelong thyroid hormone replacement therapy. These interventions, while life-saving in appropriate cases, carry major risks such as surgical complications, metabolic imbalances, and long-term dependence on medication. Beyond physical morbidity, patients experience the psychological and social burden of carrying a cancer diagnosis, even when the biological behavior of their tumor may be indolent. From a broader perspective, overtreatment also places unnecessary strain on healthcare resources, contributing to rising costs without clear improvements in patient outcomes.
Given these realities, there is increasing recognition of the need to refine approaches to thyroid cancer detection and management. Contemporary research and expert consensus are now focused on developing evidence-based strategies to minimize overdiagnosis and overtreatment. These strategies include risk stratification tools that better distinguish indolent tumors from clinically notable disease, the use of active surveillance as a viable alternative to immediate intervention for select patients, and revisions to diagnostic criteria that aim to reduce unnecessary labeling of low-risk lesions as “cancer.” Advances in molecular diagnostics, imaging interpretation, and personalized treatment planning are also being explored as mechanisms to improve clinical decision-making.[9] [10]
This analytical review seeks to critically examine the evidence surrounding thyroid cancer overdiagnosis, highlighting the complex interplay of epidemiological trends, technological advances, clinical practice patterns, and patient expectations that contribute to this phenomenon. It further evaluates the clinical, psychological, and economic consequences of overdiagnosis and overtreatment, while analyzing emerging strategies designed to mitigate these challenges. By synthesizing the most current research and expert perspectives, this paper aims to provide healthcare professionals, policymakers, and researchers with a comprehensive understanding of thyroid cancer overdiagnosis and the evolving approaches to achieving more balanced, patient-centered care.
Research Questions and Objectives
This review addresses several key questions:
- What evidence supports the existence of thyroid cancer overdiagnosis?
- What factors have contributed to the increase in thyroid cancer incidence?
- What are the clinical, psychological, and economic consequences of thyroid cancer overdiagnosis?
- How effective are current strategies, such as active surveillance, in addressing overdiagnosis?
- What recommendations exist for optimizing thyroid cancer screening and management practices?
The Evidence for Thyroid Cancer Overdiagnosis
Epidemiological Patterns Supporting Overdiagnosis
The epidemiological evidence for thyroid cancer overdiagnosis is compelling and consistent across multiple countries and healthcare systems. The analysis shows that this plateau in incidence has been primarily driven by a period effect… there is evidence that previous efforts to decrease the overdiagnosis of thyroid cancer in the USA have created a plateau rather than reduction in incidence [11] [12]. This pattern suggests that increased detection, rather than a true increase in disease occurrence, has driven the observed trends.
International studies have documented similar patterns globally. Over the study period (1989–2015) the age standardized incidence of thyroid cancer has tripled in Russian women and doubled in men [13], yet mortality rates remained stable. This disconnect between incidence and mortality serves as a key indicator of overdiagnosis, as would be expected when detecting cancers that were destined to remain clinically insignificant.
The temporal relationship between technological advancement and cancer detection provides further evidence. Greater thyroid ultrasound use led to increased diagnosis of low-risk thyroid cancer, emphasizing the need to reduce harms through reduction in inappropriate ultrasound use and adoption of nodule risk stratification tools [14]. Studies have demonstrated that regions with higher rates of imaging utilization show correspondingly higher rates of thyroid cancer diagnosis, supporting the hypothesis that increased detection rather than increased disease occurrence drives incidence trends.
Autopsy and Screening Studies
Historical autopsy studies provide crucial context for understanding the reservoir of undetected thyroid cancers in the population. Many autopsy studies on subjects who died of non-thyroidal diseases reported latent small thyroid carcinoma in up to 5.2% of the subjects. A mass screening study for thyroid cancer in Japanese adult women detected small thyroid cancer in 3.5% of the examinees [15]. These findings suggest that a substantial proportion of the population harbors clinically silent thyroid cancers that would never manifest as clinical disease.
The discrepancy between the prevalence of latent cancers found at autopsy and the lifetime incidence of clinically diagnosed thyroid cancer provides compelling evidence for the existence of a large reservoir of indolent tumors. This reservoir becomes clinically relevant only when intensive screening programs are implemented, leading to detection of cancers that would otherwise remain undiagnosed throughout a person’s lifetime.
Tumor Characteristics and Natural History
Studies examining the natural history of papillary thyroid microcarcinomas have provided insights into their typically indolent behavior. The doubling rates (per year) during active surveillance (median: 0.0) were >0.5, 0.1 to 0.5, −0.1 to 0.1, and <−0.1 in 5, 38, 97, and 29 cases, respectively. The proportions of tumors with rather rapid growth, slow growth, stable, and a decrease in size were 3%, 22%, 57%, and 17%, respectively [16]. These findings demonstrate that the majority of small thyroid cancers exhibit minimal or no growth over extended periods, supporting the concept that many detected cancers represent overdiagnosis.
After a mean of 6.8 years of observation, 29 lesions (6.0%) had increased in size. Mean age for initial calcification pattern was 52.1 years for A (n = 135), 54.2 years for B (n = 235), 56.3 years for C (n = 96), and 60.1 years for D (n = 14), and the incidence rates of tumor enlargement were 9.6, 5.5, 3.2, and 0%, respectively [17]. This age-related decrease in tumor progression suggests that older patients are particularly likely to harbor indolent lesions that represent overdiagnosis.
Factors Contributing to Increased Detection
Technological Advances in Imaging
The widespread adoption of high-resolution ultrasonography represents the primary driver of increased thyroid cancer detection. This is interpreted as an increase in the incidental detection of small papillary thyroid carcinomas by the widespread use of high-resolution imaging techniques such as ultrasonography. However, the mortality rates of thyroid carcinoma have not changed, suggesting that small papillary thyroid carcinomas may be overdiagnosed and overtreated [18].
Modern ultrasound technology can detect thyroid nodules as small as 2-3 millimeters, far smaller than what could be detected by palpation alone. While this enhanced sensitivity represents a technological achievement, it has inadvertently led to the detection of numerous clinically insignificant lesions. The increased resolution has essentially shifted the threshold of detection downward, capturing lesions that would have remained undetected in previous eras.
Screening thyroid ultrasonography exhibited a good diagnostic performance, with a feasible social cost of use. This modality demonstrated major differences in sonographic features between screening-detected cancer and benign nodules [19] [20]. However, the challenge lies not in the technical capability to distinguish malignant from benign lesions, but in determining which malignant lesions require immediate intervention versus those that can be safely monitored.
Incidental Detection During Other Procedures
The increasing use of medical imaging for various purposes has led to a noreworthy increase in incidentally detected thyroid abnormalities. Cross-sectional imaging studies performed for other indications—such as carotid duplex studies, chest CT scans, and cervical spine MRIs—frequently reveal thyroid nodules that might otherwise go undetected. This phenomenon, sometimes termed “incidentalomas,” contributes substantially to the overall detection rate of thyroid abnormalities.
Thyroid Incidentalomas in Association With Low-Dose Computed Tomography in the National Lung Screening Trial [21] [22] demonstrates how screening programs for other conditions can inadvertently lead to thyroid cancer detection. The challenge for clinicians becomes determining appropriate follow-up for these incidentally detected lesions while avoiding unnecessary cascade testing and treatment.
Healthcare System and Practice Pattern Factors
Several healthcare system factors have contributed to increased thyroid cancer detection. The defensive medicine culture has encouraged more extensive workup of thyroid nodules to avoid potential malpractice liability. Additionally, subspecialization in endocrinology and endocrine surgery has led to more aggressive evaluation and treatment approaches.
A complex interplay of environmental, medical, and social pressures has resulted in increased awareness of the thyroid disease risk, increased screening of thyroid cancers, and increased diagnosis of thyroid cancers. Although there is evidence to suggest that the true disease incidence may be changing slightly, most of the increase is related to factors that promote early diagnosis of low-risk lesions, which is resulting in a major phenomenon of overdiagnosis [23].
Patient factors also contribute to increased detection. Greater health consciousness, increased access to healthcare, and patient-driven requests for screening all play roles in the detection of thyroid abnormalities. The availability of direct-to-consumer health screening services has further amplified this trend.
Clinical Consequences of Overdiagnosis and Overtreatment
Surgical Complications and Morbidity
Thyroid surgery, while generally safe when performed by experienced surgeons, carries inherent risks that become particularly relevant when applied to patients with overdiagnosed cancers who derive no benefit from the procedure. Based on 36 studies, permanent surgical harms, hypoparathyroidism, and recurrent laryngeal nerve palsy are not uncommon. Best estimates of permanent hypoparathyroidism are from 2 to 6 events per 100 thyroidectomies and are more variable with lymph node dissection. The rate of recurrent laryngeal nerve palsy is estimated at 1 or 2 events per 100 surgeries [24].
These complications take on particular importance when considered in the context of overdiagnosis. Patients who undergo surgery for overdiagnosed cancers experience real harm from complications while receiving no benefit from cancer treatment, as their tumors would never have progressed to cause clinical problems. The ethical implications of this scenario underscore the importance of accurate risk stratification and appropriate treatment selection.
Immediate surgery in patients with papillary thyroid microcarcinoma can be associated with a higher incidence of transient vocal cord paralysis and transient and permanent hypoparathyroidism compared with the nonoperative, active surveillance approach [25]. This comparison highlights the trade-offs involved in different management strategies and supports consideration of non-surgical approaches for appropriate patients.
Radioactive Iodine Treatment Complications
For patients who undergo thyroidectomy, radioactive iodine (RAI) treatment is often recommended, adding another layer of potential harm in overdiagnosed cases. Based on 16 studies, treatment of differentiated thyroid cancer with radioactive iodine (RAI) treatment is associated with a small increase in second primary malignancies; RAI treatment is also associated with increased permanent adverse effects on the salivary gland, such as dry mouth [26].
The long-term implications of RAI therapy include not only the immediate side effects but also potential increased risks of second malignancies. When applied to patients with overdiagnosed thyroid cancers, these risks represent pure harm without any compensating benefit, as the patients’ original cancers posed no threat to their health or longevity.
Psychological and Quality of Life Impact
The psychological burden of a cancer diagnosis represents an often underappreciated consequence of overdiagnosis. Even when patients are told they have a “good” cancer with excellent prognosis, the psychological impact of the cancer diagnosis can be substantial and long-lasting. Quality of life (QoL) is crucial when deciding between active surveillance and immediate surgery, and there has been a concern that cancer worry can affect the QoL in patients with thyroid cancer [27].
Studies examining patient experiences reveal that many individuals diagnosed with thyroid cancer experience anxiety, depression, and reduced quality of life that can persist long after successful treatment. For patients with overdiagnosed cancers, these psychological sequelae represent additional unnecessary harm. The labeling effect of cancer diagnosis can profoundly impact patients’ self-perception, relationships, and life decisions.
Various studies have shown approximately 10% of the patients switching to surgery primarily related to fear factor rather than increase in the tumor size or lymph node metastasis. The results of immediate surgery do raise issues related to complications of thyroid surgery and quality of life [28]. This finding illustrates how psychological factors can drive treatment decisions even in the absence of clinical progression, highlighting the importance of psychological support and counseling in cancer management.
Economic Burden and Healthcare System Impact
Direct Healthcare Costs
The economic implications of thyroid cancer overdiagnosis are substantial and multifaceted. Annual cancer-related healthcare expenditure in the United States is estimated to exceed $150 billion by 2020… Thyroid cancer is the fastest growing cancer worldwide and is expected to surpass colon cancer as the third most common cancer in women by 2019. Although thyroid cancer is associated with a high disease-specific survival (∼98%), it is known to be associated with potentially high costs of care owing to treatment with surgery and radioactive iodine, lifelong surveillance with ultrasonography, and long-term medical therapy, similar to other cancers [29] [30].
The cumulative economic burden includes not only the immediate costs of diagnosis and treatment but also the ongoing expenses associated with long-term surveillance and management. By 2019, papillary thyroid cancer will double in incidence and become the third most common cancer in women of all ages at a cost of $18 [31] billion, representing a substantial allocation of healthcare resources to a condition with questionable clinical importance in many cases.
Cost-effectiveness analyses have questioned the value of widespread thyroid screening. Ultrasound screening for thyroid cancer has no obvious advantage in terms of cost-effectiveness compared with non-screening. The cumulative cost of screening for thyroid cancer was $18,819.24, with 18.74 quality-adjusted life years (QALYs), whereas the cumulative cost of non-screening was $15,864.28, with 18.71 QALYs. The incremental cost-effectiveness ratio of $106,947.50/QALY greatly exceeded the threshold of $50,000 [32] [33].
Patient Financial Burden
Beyond healthcare system costs, thyroid cancer diagnosis and treatment impose tremendous financial burdens on patients and their families. Estimates of the out-of-pocket costs of initial thyroid cancer diagnosis and treatment range widely ($1425-$17 000) and are influenced by age, surgical treatment type, and health insurance coverage. Independent risk factors of financial burden have included younger age, lack of health insurance, and annual household income of less than $49 000. The bankruptcy incidence at 1 year after cancer diagnosis is highest for thyroid cancer (9.3 per 1000 person-years) than other studied cancer types and 4.39-fold higher than control individuals among those aged 35 to 49 years [34] [35] [36].
Thyroid cancer survivors report greater psychological financial hardship than non-thyroid cancer survivors. Because this financial burden may be underrecognized in the medical community, further studies should be conducted to aid physicians in better understanding the impact of a thyroid cancer diagnosis [37]. The financial toxicity associated with thyroid cancer treatment represents an additional dimension of harm that disproportionately affects patients with overdiagnosed cancers.
Healthcare Resource Allocation
The management of thyroid cancer represents not only a relevant clinical and public health problem in France but also a potentially important economic burden. Overdiagnosis and corresponding associated treatments play an important role on the total costs of thyroid cancer management [38]. This resource allocation issue extends beyond individual patient care to affect healthcare system capacity and resource availability for other conditions.
The opportunity costs associated with thyroid cancer overdiagnosis include diverted resources from other healthcare needs, increased wait times for surgical procedures, and the allocation of subspecialty expertise to cases that may not require intervention. Despite these substantial clinical and economic burdens, thyroid cancer research remains underfunded by comparison, and in 2009 received only $14.7 million (ranked 30th) from the NCI. The impact of thyroid cancer on society has been underappreciated, as is evidenced by its low priority in national research funding levels [39] [40].
Active Surveillance as an Alternative Management Strategy
Evidence Base for Active Surveillance
Active surveillance has emerged as a evidence-based alternative to immediate surgery for carefully selected patients with low-risk papillary thyroid microcarcinomas. These and other studies have shown a low rate of cancer growth and lymph node metastases, no evidence of distant metastases during active surveillance of low-risk papillary thyroid carcinoma, and no life-threatening recurrence or death in patients who required surgery owing to disease progression [41].
The concept of active surveillance for thyroid microcarcinomas originated in Japan, where extensive experience has been accumulated. Active surveillance management has been introduced from Japan since the 1990s, as one of the measures to prevent overtreatment of low-risk papillary thyroid microcarcinoma [42]. The Japanese experience demonstrates that carefully selected patients can be safely monitored without immediate intervention, with surgery reserved for cases showing evidence of progression.
Based on existing literature and clinical experience, it appears that active surveillance is an appropriate strategy for monitoring micropapillary carcinoma [43]. Multiple international studies have now validated the safety and effectiveness of this approach in different healthcare settings and patient populations.
Patient Selection Criteria
Appropriate patient selection represents a critical component of successful active surveillance programs. Patients with thyroid cancer adjacent to either the trachea or recurrent laryngeal nerve or those with evidence of extrathyroidal extension, a high-risk molecular profile, lymph node, or distant metastases are considered inappropriate candidates for active surveillance [44]. These exclusion criteria help identify patients who require immediate intervention due to higher risk features.
The most ideal candidate would be patients with a tumor below 1 cm, intrathyroidal [45] [46]. Additional patient-related factors must also be considered, including age, comorbidities, patient preference, and psychological suitability for surveillance. To determine the most appropriate candidates for active surveillance, factors such as tumor size, location, multiplicity, and ultrasound findings are considered, along with patient characteristics like medical condition, age, and family history. Moreover, shared decision-making, which includes patient-reported outcomes such as quality of life and cost-effectiveness, is essential [47].
Monitoring Protocols and Progression Criteria
Standardized monitoring protocols have been developed to ensure safe implementation of active surveillance. For the patient who is a minimalist, the follow up strategy includes, ultrasound every 6 months for the first 1 or 2 years, and then every year after that [48] [49]. This surveillance schedule balances the need for adequate monitoring with practical considerations of cost and patient convenience.
An increase in maximal diameter by ≥3.0 mm, increases in the volume of thyroid nodules by 50%, or the development of lymph node metastases usually define disease progression and thus an indication for surgery [50]. These objective criteria help standardize decision-making regarding when to convert from surveillance to surgical intervention.
During active surveillance, patients undergo regular ultrasound examinations to monitor for signs of disease progression, including tumor growth, extrathyroidal extension, or lymph node metastasis. While active surveillance is a feasible and reliable approach for managing low-risk thyroid cancer, it requires careful patient selection, effective communication for shared decision-making, standardized follow-up protocols, and a clear definition of disease progression [51].
International Guidelines and Implementation
Professional organizations worldwide have increasingly endorsed active surveillance as an appropriate management option. In 2010, the Japanese Society of Thyroid Surgeons and Japan Association of Endocrine Surgeons guidelines for treating thyroid nodules adopted recommendations favoring active surveillance for low-risk PTMC as one treatment option. The American Thyroid Association has similarly endorsed the active surveillance management approach in patients with intrathyroidal papillary microcarcinoma, beginning in 2015 [52].
At present, active surveillance is a safe and reasonable approach in properly selected patients with low-risk papillary thyroid microcarcinoma, reducing the risks associated with thyroid surgery at a potentially reduced cost. The decision for active surveillance should be individualized, taking into account patient preference, patient characteristics, and tumor characteristics. Furthermore, the sophistication of the medical team, multidisciplinary approach, follow-up capabilities, and experience with high-quality ultrasound should be considered [53].

Current Screening Recommendations and Guidelines
U.S. Preventive Services Task Force Position
The U.S. Preventive Services Task Force has taken a clear position against routine thyroid cancer screening based on comprehensive evidence review. The USPSTF recommends against screening for thyroid cancer in asymptomatic adults. (D recommendation) [54]. This recommendation reflects careful consideration of the balance between potential benefits and harms of screening.
The USPSTF found inadequate direct evidence on the benefits of screening but determined that the magnitude of the overall benefits of screening and treatment can be bounded as no greater than small, given the relative rarity of thyroid cancer, the apparent lack of difference in outcomes between patients who are treated vs monitored (for the most common tumor types), and observational evidence showing no change in mortality over time after introduction of a mass screening program. The USPSTF found inadequate direct evidence on the harms of screening but determined that the overall magnitude of the harms of screening and treatment can be bounded as at least moderate, given adequate evidence of harms of treatment and indirect evidence that overdiagnosis and overtreatment are likely to be substantial with population-based screening. The USPSTF therefore determined that the net benefit of screening for thyroid cancer is negative [55].
Professional Society Guidelines
Professional medical societies have generally aligned with the evidence-based approach advocating against routine screening while supporting more judicious use of diagnostic procedures. The approach emphasizes clinical assessment and risk-stratified evaluation rather than population-based screening. Although ultrasonography of the neck using high-risk sonographic characteristics plus follow-up cytology from fine-needle aspiration can identify thyroid cancers, it is unclear if population-based or targeted screening can decrease mortality rates or improve important patient health outcomes. Screening that results in the identification of indolent thyroid cancers, and treatment of these overdiagnosed cancers, may increase the risk of patient harms [56] [57].
The emphasis has shifted toward improving the quality of diagnostic evaluation when thyroid abnormalities are detected incidentally or in symptomatic patients, rather than expanding screening efforts. This includes implementation of risk stratification systems, molecular testing when appropriate, and multidisciplinary care coordination.
International Variations in Approach
Different countries have adopted varying approaches to thyroid cancer screening and management, reflecting cultural, healthcare system, and resource differences. Some countries with established screening programs, such as South Korea, have experienced dramatic increases in thyroid cancer incidence with associated debates about the appropriateness of continued screening.
The Korean experience has been particularly instructive, demonstrating the potential consequences of widespread screening programs. Korea’s thyroid-cancer “epidemic”–screening and overdiagnosis [58] illustrates how screening initiatives can lead to substantial overdiagnosis with associated healthcare system and patient impacts.
Strategies to Address Overdiagnosis
Reducing Inappropriate Imaging
Efforts to address thyroid cancer overdiagnosis must begin with more judicious use of imaging studies. This includes developing clearer indications for thyroid ultrasonography, implementing decision support systems to guide appropriate testing, and educating healthcare providers about the risks of overdiagnosis. It is crucial that we continue to actively work on novel strategies to reduce the drivers of overdiagnosis [59].
Healthcare institutions can implement audit and feedback systems to monitor thyroid ultrasound utilization patterns and identify opportunities for optimization. Professional societies can develop and disseminate appropriate use criteria that help guide clinical decision-making regarding when thyroid imaging is indicated.
Improving Risk Stratification Systems
Enhanced risk stratification systems can help distinguish clinically vital thyroid cancers from those that represent overdiagnosis. The European Thyroid Imaging and Reporting Data System as a Remedy for the Overdiagnosis and Overtreatment of Thyroid Cancer: Results from the EUROCRINE Surgical Registry [60] represents one approach to standardizing risk assessment and improving diagnostic accuracy.
Molecular testing and genetic profiling may help identify tumors with indolent behavior that are appropriate for surveillance rather than immediate treatment. Integration of clinical, imaging, and molecular information can improve risk stratification and treatment decision-making.
Education and Shared Decision-Making
Healthcare provider education represents a crucial component of addressing overdiagnosis. Clinicians need training in communicating uncertainty, discussing risks and benefits of different management options, and supporting patient decision-making. Although thyroid surgery is the most common management option for patients with papillary thyroid microcarcinoma, new management options demand that treatment decisions must be individualized and based on patient’s preference, context, and biology. This article describes management options for papillary thyroid microcarcinoma patients and shared decision-making as a novel method for individualizing care [61].
Patient education materials should accurately communicate the likelihood that detected thyroid abnormalities represent clinically noteworthy disease versus overdiagnosis. This includes helping patients understand the concept of overdiagnosis and the rationale for different management approaches including active surveillance.
Healthcare Policy Interventions
Policy-level interventions may be necessary to address systemic factors contributing to overdiagnosis. This could include insurance coverage policies that support active surveillance, quality measures that assess appropriate use of screening and diagnostic procedures, and research funding priorities that focus on identifying clinically noteworthy disease.
Increased awareness in the medical community and the general public of the societal burden of thyroid cancer, and substantial increases in research on thyroid cancer etiology, prevention, and treatment are needed to offset these growing concerns [62]. Policy makers need evidence-based information to make informed decisions about resource allocation and healthcare priorities.
Future Directions and Research Needs
Molecular and Genetic Advances
Future research should focus on developing more sophisticated methods for distinguishing clinically remarkable thyroid cancers from those representing overdiagnosis. This includes advancing our understanding of the molecular basis of thyroid cancer progression and identifying biomarkers that can predict clinical behavior. Diagnostic molecular markers, such as RET-PTC, RAS, and BRAFV600E mutations; galectin 3; and a new gene expression classifier, are outstanding examples that have improved diagnosis of thyroid nodules. BRAF mutation is a prognostic genetic marker that has improved risk stratification and hence tailored management of patients with thyroid cancer, including those with conventionally low risks. Novel molecular-targeted treatments hold great promise for radioiodine-refractory and surgically inoperable thyroid cancers as shown in clinical trials; such treatments are likely to become a component of the standard treatment regimen for patients with thyroid cancer in the near future. These novel molecular-based management strategies for thyroid nodules and thyroid cancer are the most exciting developments in this unprecedented era of molecular thyroid-cancer medicine [63].
Long-term Outcomes Research
Extended follow-up studies are needed to better understand the long-term outcomes of different management approaches, including active surveillance versus immediate surgery. This research should examine not only cancer-specific outcomes but also quality of life, functional status, and patient satisfaction measures.
The current study, encompassing over 15,000 patient-years of follow-up, is the largest study of its type to date. The primary message of these data is that patients with papillary thyroid microcarcinoma have an excellent prognosis [64]. Building on this foundation, future studies should continue to expand our understanding of natural history and optimal management approaches.
Healthcare System and Implementation Research
Research is needed to understand how to effectively implement evidence-based approaches to reducing overdiagnosis within different healthcare systems. This includes studying barriers and facilitators to adopting active surveillance, developing effective educational interventions for healthcare providers, and designing systems-level interventions to support appropriate care.
Patient-Centered Outcomes Research
Future research should prioritize patient-centered outcomes and incorporate patient preferences and values into study design and interpretation. This includes developing and validating patient-reported outcome measures specific to thyroid cancer, studying the effectiveness of shared decision-making interventions, and examining the impact of different management approaches on patient well-being.
Limitations and Challenges
Diagnostic Uncertainty
One of the fundamental challenges in addressing thyroid cancer overdiagnosis is the inherent uncertainty in determining which cancers will progress to cause clinical problems. Current risk stratification systems, while helpful, cannot perfectly predict tumor behavior. This uncertainty complicates clinical decision-making and can lead to conservative management approaches that may contribute to overtreatment.
The challenge is compounded by the excellent overall prognosis of thyroid cancer, which makes it difficult to design studies with sufficient power to detect meaningful differences in outcomes between different management strategies. Long-term follow-up periods are required to adequately assess the safety of less aggressive approaches.
Medicolegal Considerations
Healthcare providers face medicolegal pressures that may encourage more aggressive evaluation and treatment of thyroid abnormalities. The fear of missing a cancer diagnosis can drive clinical decision-making toward more extensive testing and treatment, even when clinical evidence suggests a more conservative approach would be appropriate.
Professional liability considerations may discourage adoption of active surveillance approaches, particularly in healthcare systems with high litigation rates. Addressing these concerns requires clear evidence-based guidelines, professional society support, and potentially legal system reforms that recognize appropriate care variations.
Healthcare System Barriers
Implementation of evidence-based approaches to reducing overdiagnosis faces various healthcare system barriers. These include reimbursement policies that favor procedural interventions over surveillance, fragmented care delivery that hinders coordination of surveillance programs, and provider time constraints that limit ability to engage in complex shared decision-making discussions.
Restrictive diagnostic workup strategies of patients with small thyroid nodules lead to limited patients eligible for active surveillance and a higher incidence of lymph node metastases. We believe that there is limited additive value for active surveillance in countries with restrictive diagnostic approaches [65]. This finding highlights how healthcare system characteristics can influence the feasibility and effectiveness of different management approaches.
Patient and Cultural Factors
Patient acceptance of active surveillance can be challenging, particularly in cultures where cancer diagnosis is associated with immediate treatment expectations. Various studies have shown approximately 10% of the patients switching to surgery primarily related to fear factor rather than increase in the tumor size or lymph node metastasis [66].
Cultural attitudes toward cancer, tolerance for uncertainty, and trust in healthcare providers all influence patient willingness to consider surveillance approaches. Educational interventions and psychological support may be necessary to help patients understand and accept surveillance approaches when clinically appropriate.
Implications for Clinical Practice
Clinical Decision-Making Framework
Healthcare providers need structured approaches to clinical decision-making that incorporate evidence about overdiagnosis and overtreatment. This framework should include systematic risk assessment, consideration of patient preferences and values, and clear communication about the uncertainty inherent in cancer diagnosis and prognosis.
Owing to its excellent prognosis with low morbidity and mortality, balancing treatment risks with risks of disease progression can be challenging, leading to several areas of controversy. In particular, overdiagnosis, active surveillance vs surgery, extent of surgery, radioactive iodine (RAI) treatment, thyrotropin suppression, and postoperative surveillance are discussed. Recommendations regarding the diagnosis of differentiated thyroid cancer, the extent of treatment for low-risk differentiated thyroid cancer patients, and the intensity of posttreatment follow-up have all changed substantially in the past decade [67] [68].
Provider Education and Training
Medical education curricula need to incorporate concepts of overdiagnosis, shared decision-making, and evidence-based approaches to managing diagnostic uncertainty. This includes training in risk communication, understanding of test performance characteristics, and skills in supporting patients through complex decision-making processes.
Continuing education programs should address the latest evidence regarding thyroid cancer management and provide practical guidance for implementing surveillance approaches when appropriate. Professional societies play a crucial role in developing and disseminating educational content that supports evidence-based practice.
Quality Measurement and Improvement
Healthcare organizations need quality measurement systems that assess appropriateness of thyroid cancer care rather than simply measuring process indicators. This includes developing metrics that evaluate decision-making quality, patient satisfaction with the decision-making process, and long-term patient outcomes across different management approaches.
Quality improvement initiatives should focus on reducing unnecessary testing and treatment while ensuring that clinically important cancers receive appropriate care. This requires careful balance to avoid both overdiagnosis and underdiagnosis.

Conclusion 
The evidence overwhelmingly supports the existence of widespread thyroid cancer overdiagnosis, driven primarily by increased use of high-resolution imaging technology and more intensive screening practices. This phenomenon has resulted in substantial harm to patients through unnecessary surgery, radioactive iodine treatment, psychological distress, and financial burden, while consuming major healthcare resources without corresponding improvements in mortality outcomes.
These findings suggest that a substantial and growing part of the detected thyroid cancers are overdiagnosed and overtreated. Targeted screening and diagnostic strategies are warranted to avoid overdetection and unnecessary treatment of thyroid cancers [69]. The challenge for the medical community is to develop and implement strategies that reduce overdiagnosis while ensuring these cancers receive appropriate treatment.
Active surveillance has emerged as a safe and effective alternative to immediate surgery for carefully selected patients with low-risk papillary thyroid microcarcinomas. The evidence base supporting this approach continues to grow, with multiple international studies demonstrating low rates of disease progression and excellent patient outcomes. However, successful implementation requires appropriate patient selection, standardized monitoring protocols, multidisciplinary care coordination, and effective communication with patients.
The path forward requires multifaceted approaches addressing technological, clinical, educational, and policy dimensions of the overdiagnosis problem. This includes more judicious use of imaging studies, improved risk stratification systems, enhanced provider education, and healthcare policies that support evidence-based care. Patient education and shared decision-making represent crucial components of any comprehensive strategy to address overdiagnosis.
Future research priorities should focus on developing better methods for distinguishing tumors from those representing overdiagnosis, understanding long-term outcomes of different management approaches, and designing effective interventions to support implementation of evidence-based care. The molecular characterization of thyroid cancers holds particular promise for improving risk stratification and treatment decision-making.
The thyroid cancer overdiagnosis phenomenon serves as a broader lesson for modern medicine about the unintended consequences of technological advancement and the importance of evidence-based approaches to screening and treatment. As medical technology continues to advance, the principles learned from addressing thyroid cancer overdiagnosis may inform approaches to other conditions where similar challenges arise.
The ultimate goal is to optimize patient outcomes by providing the right treatment to the right patient at the right time, while minimizing harm from unnecessary interventions. This requires ongoing commitment from healthcare providers, professional organizations, healthcare systems, and policymakers to support evidence-based care that prioritizes patient well-being over other considerations. The stakes are high—both for individual patients who may be harmed by overdiagnosis and overtreatment, and for healthcare systems seeking to provide high-value care in an era of limited resources.
By continuing to advance our understanding of thyroid cancer biology, improving risk stratification methods, and supporting patient-centered decision-making, we can work toward a future where thyroid cancer care is optimally matched to individual patient needs and preferences, minimizing both overdiagnosis and underdiagnosis while maximizing patient well-being and healthcare value.
References:
American Thyroid Association. (2016). 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer. Thyroid, 26(1), 1-133.
Baek, H. S., Ha, J., Kim, K., Bae, J. S., Kim, J. S., Kim, S., Lim, D. J., & Kim, C. M. (2024). Cost-utility analysis of early detection with ultrasonography of differentiated thyroid cancer: A retrospective study on a Korean population. Endocrinology and Metabolism, 39(2), 310-323.
Bogdanovski, A. K., Sturgeon, C., & James, B. C. (2022). The cost and financial burden of thyroid cancer on patients in the US: A review and directions for future research. JAMA Otolaryngology-Head & Neck Surgery, 148(6), 568-575.
Dal Maso, L., Panato, C., Franceschi, S., Serraino, D., Buzzoni, C., Busco, S., … & Vaccarella, S. (2018). The impact of overdiagnosis on thyroid cancer epidemic in Italy, 1998-2012. European Journal of Cancer, 94, 6-15.
Davies, L., & Morris, L. G. T. (2017). The USPSTF recommendation on thyroid cancer screening: Don’t “check your neck”. JAMA Otolaryngology-Head & Neck Surgery, 143(8), 755-756.
Dedhia, P. H., Saucke, M. C., Long, K. L., Doherty, G. M., & Pitt, S. C. (2022). Physician perspectives of overdiagnosis and overtreatment of low-risk papillary thyroid cancer in the US. JAMA Network Open, 5(4), e228722.
Fukuoka, O., Sugitani, I., Ebina, A., Toda, K., Kawabata, K., & Yamada, K. (2016). Natural history of asymptomatic papillary thyroid microcarcinoma: Time-dependent changes in calcification and vascularity during active surveillance. World Journal of Surgery, 40(3), 529-537.
Haymart, M. R., Esfandiari, N. H., Stang, M. T., & Sosa, J. A. (2022). Current controversies in low-risk differentiated thyroid cancer: Reducing overtreatment in an era of overdiagnosis. Endocrine Reviews, 43(6), 1007-1024.
Hoang, J. K., Nguyen, X. V., & Davies, L. (2015). Overdiagnosis of thyroid cancer: Answers to five key questions. Academic Radiology, 22(8), 1024-1029.
Jegerlehner, S., Chiolero, A., Aujesky, D., Rodondi, N., Germann, S., Konzelmann, I., … & NICER Working Group. (2017). Overdiagnosis and overtreatment of thyroid cancer: A population-based temporal trend study. PLoS One, 12(6), e0179387.
Kim, M. J., Moon, J. H., Lee, E. K., Song, Y. S., Jung, K. Y., Lee, J. Y., … & Park, Y. J. (2024). Active surveillance for low-risk thyroid cancers: A review of current practice guidelines. Endocrinology and Metabolism, 39(1), 47-60.
Lang, B. H., Wong, C. K., & Wan, K. Y. (2021). Differentiated thyroid cancer: A health economic review. Clinical Endocrinology, 95(1), 28-46.
Li, M., Dal Maso, L., & Vaccarella, S. (2020). Global trends in thyroid cancer incidence and the impact of overdiagnosis. The Lancet Diabetes & Endocrinology, 8(6), 468-470.
Lin, J. S., Bowles, E. J. A., Williams, S. B., & Morrison, C. C. (2017). Screening for thyroid cancer: Updated evidence report and systematic review for the US Preventive Services Task Force. JAMA, 317(18), 1888-1903.
Miyauchi, A., Ito, Y., & Oda, H. (2018). Insights into the management of papillary microcarcinoma of the thyroid. Thyroid, 28(1), 23-31.
Nickel, B., Brito, J. P., Barratt, A., Jordan, S., Moynihan, R., & McCaffery, K. (2017). From overdiagnosis to overtreatment of low-risk thyroid cancer: A thematic analysis of attitudes and beliefs of endocrinologists, surgeons, and patients. Thyroid, 30(5), 696-703.
Sanabria, A., Kowalski, L. P., Shah, J. P., Nixon, I. J., Angelos, P., Williams, M. D., … & Ferlito, A. (2018). Growing incidence of thyroid carcinoma in recent years: Factors underlying overdiagnosis. Head & Neck, 40(4), 855-866.
Solis-Pazmino, P., Salazar-Vega, J., Lincango-Naranjo, E., Garcia, C., Jaramillo Koupermann, G., Ortiz-Prado, E., … & Brito, J. P. (2021). Thyroid cancer overdiagnosis and overtreatment: A cross-sectional study at a thyroid cancer referral center in Ecuador. BMC Cancer, 21(1), 42.
Tuttle, R. M., Zhang, L., Shaha, A., & Shah, J. P. (2022). Active surveillance for low-risk differentiated thyroid cancer. Endocrinology and Metabolism Clinics of North America, 51(4), 679-698.
U.S. Preventive Services Task Force. (2017). Screening for thyroid cancer: US Preventive Services Task Force recommendation statement. JAMA, 317(18), 1882-1887.
Vaccarella, S., Franceschi, S., Bray, F., Wild, C. P., Plummer, M., & Dal Maso, L. (2016). Worldwide thyroid-cancer epidemic? The increasing impact of overdiagnosis. New England Journal of Medicine, 375(7), 614-617.
Walgama, E., Sacks, W. L., & Ho, A. S. (2020). Papillary thyroid microcarcinoma: Optimal management versus overtreatment. Current Opinion in Oncology, 32(1), 1-6.
Zaridze, D., & Maximovitch, D. (2021). Thyroid cancer overdiagnosis revisited. Cancer Epidemiology, 74, 101994.
Zhou, Q., Li, H. L., Li, Y., Gu, Y. T., Liang, Y. R., Liu, H. Z., … & Lin, G. Z. (2021). Cost-effectiveness analysis of ultrasound screening for thyroid cancer in asymptomatic adults. Frontiers in Public Health, 9, 643208.
Zhu, Q., Liu, J., Hu, J., & Zhang, Y. (2025). The epidemiological landscape of thyroid cancer and estimates of overdiagnosis in China: A population-based study. Thyroid, 35(3), 307-320.

