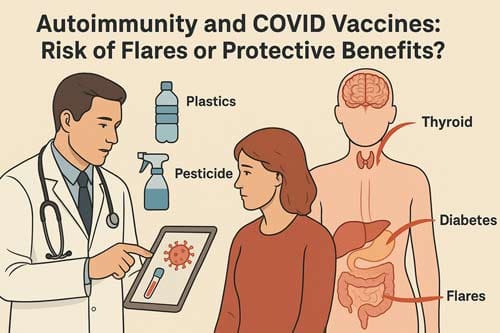
Autoimmunity and COVID Vaccines: Risk of Flares or Protective Benefits? A Comprehensive Analysis for Academic and Industry Experts
Abstract
The link between getting a COVID-19 vaccine and having an autoimmune disease is an intricate blend of immunology, public health, and clinical practice. This analytical review examines the benefits and risks of COVID-19 vaccines for individuals with autoimmune diseases. It looks at both the possible dangers of disease flares and the protective benefits of not getting SARS-CoV-2. Through a systematic analysis of recent literature spanning 2021-2025, we evaluate mechanisms of vaccine-induced autoimmune phenomena, including molecular mimicry, bystander activation, and adjuvant effects, while assessing the clinical evidence for both benefits and risks. The research reveals that COVID-19 vaccines are less effective in people with weakened immune systems than in healthy people, but they still offer significant protection against serious COVID-19 outcomes. About 10 to 18 percent of people with autoimmune inflammatory rheumatic diseases have disease flares after getting vaccinated. Most of these are mild to moderate in severity. The evidence shows that the benefits of vaccination far outweigh the risks of autoimmune flares. This supports the current recommendations for vaccination in this at-risk group. For the best clinical outcomes, though, individualised approaches that take into account disease activity, immunosuppressive medications, and patient-specific risk factors are still very important.
Keywords: COVID-19 vaccines, autoimmune diseases, molecular mimicry, bystander activation, immunocompromised patients, vaccine safety, disease flares
Introduction
The global COVID-19 pandemic has fundamentally transformed our understanding of vaccine immunology, particularly in vulnerable populations, including patients with autoimmune diseases. Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has resulted in more than 670 million infections and almost 7 million deaths globally [1] [2]. The quick development and distribution of COVID-19 vaccines was an unprecedented scientific achievement. However, there are still many complicated questions about how safe and effective they are for people with weak immune systems.
Patients with autoimmune diseases face a unique clinical dilemma. They are simultaneously at increased risk for severe COVID-19 outcomes due to their underlying immunosuppression and potentially vulnerable to vaccine-induced autoimmune phenomena. Multiple studies have demonstrated the effectiveness and safety of vaccines against COVID-19 in healthy populations, in people with risk factors, in people with or without SARS-CoV-2 infection, and immunocompromised people [3]. However, the exclusion of immunocompromised patients from initial clinical trials has created a knowledge gap that has been gradually filled through real-world evidence and post-marketing surveillance studies.
This analytical review addresses the critical question: Do COVID-19 vaccines pose greater risks of autoimmune flares, or do their protective benefits outweigh potential adverse effects in patients with autoimmune diseases? By examining the current evidence base, we aim to provide a balanced perspective that acknowledges both the complexity of immune interactions and the practical clinical considerations that inform vaccination decisions in this vulnerable population.
The research question guiding this analysis is whether COVID-19 vaccination in patients with autoimmune diseases represents a net clinical benefit when weighing protective effects against SARS-CoV-2 infection versus the risk of triggering autoimmune disease flares or new-onset autoimmune phenomena.
Mechanisms of Vaccine-Induced Autoimmune Phenomena
Molecular Mimicry
Molecular mimicry refers to a significant similarity between certain pathogenic elements contained in the vaccine and specific human proteins. This similarity may lead to immune crossreactivity, wherein the reaction of the immune system towards the pathogenic antigens may harm the similar human proteins, essentially causing autoimmune disease [4]. In the context of COVID-19 vaccines, several mechanisms have been proposed to explain potential autoimmune phenomena.
Molecular mimicry is one of the leading mechanisms by which infectious or chemical agents may induce autoimmunity. It occurs when similarities between foreign and self-peptides favor an activation of autoreactive T or B cells by a foreign-derived antigen in a susceptible individual [5]. The SARS-CoV-2 spike protein, which serves as the primary target antigen for most COVID-19 vaccines, shares structural similarities with various human proteins.
It has been recognized from the onset that specific immunological processes, such as molecular mimicry and immunological crossreactivity, may contribute to the induction of autoantibodies. Here, we attempt to gather the present information, especially that which suits the needs of verifying the stimulation of autoimmunity through molecular mimicry. Finding sequence or structure similarities provided an immense amount of proof-of-concept support. At the same time, the detection of significantly higher levels of autoantibodies in the patient samples was credited as experimental evidence [6].
Autoimmunity following SARS-CoV-2 infection and vaccination is common, and molecular mimicry could play a paramount role. Epidemiological data and animal studies on multiple ADs suggest that molecular mimicry is one of the likely mechanisms for the loss of peripheral tolerance and the development of clinical disease [7] [8].
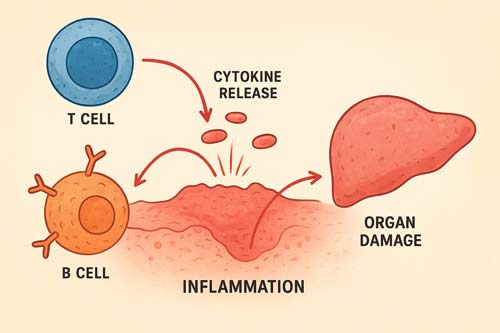
Bystander Activation
Bystander T cell activation refers to the activation of T cells without antigen recognition. During an immune response to a pathogen, bystander activation of self-reactive T cells via inflammatory mediators such as cytokines can trigger autoimmune diseases [9]. This mechanism represents a non-specific pathway through which vaccination can potentially trigger autoimmune phenomena.
Three main mechanisms have been offered to explain the development of autoimmunity: molecular mimicry, epitope spreading, and bystander activation. The latter is characterized by auto-reactive B and T cells that undergo activation in an antigen-independent manner, influencing the development and course of autoimmunity [10].
The inflammatory milieu created by vaccination can activate autoreactive immune cells that were previously in a quiescent state. During the innate immune response following vaccination, the immune system produces a large number of cytokines, which may induce autoimmunity through the bystander activation pathway. It includes the activation of bystander CD8+T cells primarily under the action of IL-15 and the activation of CD4+T cells primarily under the influence of IL-2 [11] [12].
We present probable pathways underpinning the genesis of COVID-19 autoimmunity, such as bystander activation caused by hyperinflammatory conditions, viral persistence, and the creation of neutrophil extracellular traps. Other hypothesized mechanisms include bystander activation induced by a hyper-inflammatory state (also known as “cytokine storm” or “cytokine release syndrome”), viral persistence (polyclonal activation caus [13] [14].
Adjuvant Effects
Molecular mimicry is involved in these phenomena, as is the necessity for the presence of two chemically complementary antigens and an immunologic adjuvant. The HLA pattern of the host is also an important factor [15]. While mRNA COVID-19 vaccines do not contain traditional adjuvants, the lipid nanoparticles and the mRNA itself can act as immunostimulatory agents.
Adjuvants in vaccines can act as ligands for pattern recognition receptors (PRRs), such as toll-like receptors (TLRs), bind to them to mobilize innate immune cells and secrete massive cytokines, and induce an innate immune response. Additionally, adjuvants also enhance the induction of adaptive immune responses to vaccine antigens [16].
The safety profile of vaccine adjuvants has been extensively studied. The tripartite group of experts concluded that there is no compelling evidence supporting the association of vaccine adjuvants with autoimmunity signals. No convincing evidence was found associating adjuvants and autoimmunity in humans [17] [18].
Clinical Evidence: Disease Flares Following COVID-19 Vaccination
Incidence and Characteristics of Flares
Multiple large-scale studies have documented the incidence of autoimmune disease flares following COVID-19 vaccination. 18% patients flared, of which 11.7% were within the 3 months of interest. Median (IQR) time-to-flare was 60 (30, 114) days. 25% of flares were self-limiting, 61% were mild to moderate, and 14% were severe [19] [20] [21] in the CONVIN-SING study, which represents one of the largest cohorts examining this phenomenon.
Flares occur in nearly 1 in 10 individuals with AIRDs after COVID vaccination; people with comorbidities (especially AIDm), MHDs, and those receiving the Moderna vaccine are particularly vulnerable [22]. This finding from the COVAD study provides additional perspective on the global incidence of post-vaccination flares.
The temporal relationship between vaccination and flare onset is essential for clinical management. The median period between immunization and the start of symptoms was eight days (IQR: 3 to 14) [23], suggesting that most vaccine-related autoimmune phenomena occur within the first two weeks following vaccination.
Risk Factors for Post-Vaccination Flares
Several clinical and demographic factors influence the risk of developing flares following COVID-19 vaccination. Older patients (53–65 years and >66 years) had a lower risk of flare [HR 0.6 (95% CI 0.5–0.8) and 0.7 (0.6–0.8), respectively]. Patients with inflammatory arthritis and with active disease had a higher risk of flare [HR 1.5 (1.2–2.0) and 1.4 (1.2–1.6), respectively]. Treatment with conventional synthetic disease-modifying anti-rheumatic drugs (csDMARDs), immunosuppression, and prednisolone was also associated with an increased risk of flare [24].
The first dosage was linked with new-onset events (69.8% vs. 59.3%, P = 0.0100), whereas the second dose was related to relapsing disease (29.5% vs. 59.3%, P = 0.0159). New-onset conditions and relapsing diseases were more common in women (51.5% and 62.9%, respectively; P = 0.0081) [25].
Specific Autoimmune Conditions
The spectrum of autoimmune phenomena reported following COVID-19 vaccination is broad. Immune thrombotic thrombocytopenia, autoimmune liver diseases, Guillain-Barré syndrome, IgA nephropathy, rheumatoid arthritis, and systemic lupus erythematosus. Immune thrombotic thrombocytopenia, autoimmune liver diseases, Guillain-Barré syndrome, IgA nephropathy, rheumatoid arthritis, and systemic lupus erythematosus [26] [27] represent the most commonly reported conditions.
The most common diseases associated with new-onset events following vaccination were immune thrombocytopenia, myocarditis, and Guillain-Barré syndrome. In contrast, immune thrombocytopenia, psoriasis, IgA nephropathy, and systemic lupus erythematosus were the most common illnesses associated with relapsing episodes [28].
Protective Benefits of COVID-19 Vaccination in Immunocompromised Patients
Vaccine Effectiveness
Despite reduced immunogenicity, COVID-19 vaccines demonstrate significant protective effects in immunocompromised populations. The pooled DOR for symptomatic COVID-19 infection in immunocompromised patients was 0.296 (95% CI: 0.108-0.811) with an estimated VE of 70.4% (95% CI: 18.9%- 89.2%). The pooled DOR for symptomatic COVID-19 infection in immunocompromised patients was 0.296 (95% CI: 0.108-0.811) with an estimated VE of 70.4% (95% CI: 18.9%- 89.2%) [29] [30].
VE of the widely available COVID-19 vaccines, including BNT162b2 (Pfizer/BioNTech), mRNA-1273 (Moderna), and Ad26.COV2.S (Janssen), and ChAdOx1 nCoV-19 (Oxford/AstraZeneca), ranged from 64% to 90% against SARS-CoV-2 infection, 73% to 84% against symptomatic illness, 70% to 100% against severe illness, COVID-19 VE for most outcomes in the IC populations included in these studies were lower than in the general populations [31].
VE of 2 doses of mRNA COVID-19 vaccine against COVID-19-associated hospitalization was lower among immunocompromised patients (77%; 95% confidence interval [CI] = 74%-80%) than among immunocompetent patients (90%; 95% CI = 89%-91%). VE of 2 doses of mRNA COVID-19 vaccine against COVID-19-associated hospitalization was lower among immunocompromised patients (77%; 95% confidence interval [CI] = 74%-80%) than among immunocompetent patients (90%; 95% CI = 89%-91%) [32] [33].
Immunogenicity in Different Patient Populations
The immune response to COVID-19 vaccines varies significantly among different immunocompromised populations. Seroconversion was increasingly likely in patients with haematological cancers (0.63, 0.57 to 0.69, I2=88%; 0.62, 0.54 to 0.70, I2=90%), immune mediated inflammatory disorders (0.75, 0.69 to 0.82, I2=92%; 0.77, 0.66 to 0.85, I2=93%), and solid cancers (0.90, 0.88 to 0.93, I2=51%; 0.89, 0.86 to 0.91, I2=49%). Seroconversion was similar between people with HIV and immunocompetent controls (1.00, 0.98 to 1.01, I2=0%; 0.97, 0.83 to 1.00, I2=89%) [34].
The proportion of non-responders seemed higher among solid organ transplant recipients (range 18–100%) and patients with haematological malignancy (range 14–61%), and lower in patients with cancer (range 2–36%) and patients on dialysis (range 2–30%). Risk factors for non-response included older age, use of corticosteroids, immunosuppressive or anti-CD20 agents [35].
Benefits of Additional Doses
The value of booster vaccinations in immunocompromised populations has been demonstrated in multiple studies. The investigators found that the risk for any SARS-CoV-2 infection, COVID-19-related hospitalisation, and death was reduced with a fourth dose of the vaccine. This effect held in several subgroups except for patients treated with rituximab. The investigators found that the risk for any SARS-CoV-2 infection, COVID-19-related hospitalisation, and death was reduced with a fourth dose of the vaccine. This effect held in several subgroups except for patients treated with rituximab. In this emulated target trial, we found that a fourth dose of COVID-19 mRNA vaccine was associated with a significantly lower risk of SARS-CoV-2 infection and COVID-19-related admission to hospital or death compared with not receiving a fourth dose among patients with systemic autoimmune rheumatic diseases using DMARDs [36] [37] [38].
Results indicated that individuals receiving booster doses experienced superior outcomes compared to those without boosters. Elevated antibody levels post-booster dose vaccination in the population signaled robust immune responses, underscoring the benefits of supplementary vaccine doses. This systematic review highlights preliminary evidence supporting the immunologic outcomes and safety of COVID-19 vaccine boosters in enhancing immune responses against SARS-CoV-2 [39] [40].
Risk-Benefit Analysis in Specific Autoimmune Conditions
Systemic Lupus Erythematosus
Patients with systemic lupus erythematosus (SLE) represent a particularly well-studied population regarding COVID-19 vaccination. Patients with SLE have worse immune responses following SARS-CoV-2 vaccination than healthy controls. Patients with SLE have worse immune responses following SARS-CoV-2 vaccination than healthy controls. The efficacy of the COVID-19 vaccines seems to be further reduced by immunosuppressive medications, such as glucocorticoids (GC), methotrexate (MTX), mycophenolate/mycophenolic acid (MMF), and rituximab (RTX) [41] [42].
Despite reduced immunogenicity, vaccination remains beneficial for SLE patients. The danger of not administering the COVID-19 vaccination to SLE patients is significantly larger than the likelihood of its adverse effects, which are most likely caused by intrinsic immune failure and demographic differences. Historical data from influenza vaccination provides additional context: Trivalent split influenza vaccine without adjuvant seems to be safe and immunogenic in patients with SLE and RA, provided that only patients with low and/or stable disease activity are selected [43].
SLE patients, regardless of background immunosuppressive therapy, had lower vaccine IgG levels than health care workers. Mycophenolate, tacrolimus, and belimumab significantly reduced IgG response to vaccination, highlighting the importance of considering specific immunosuppressive regimens when counseling patients.
Rheumatoid Arthritis
Rheumatoid arthritis patients also demonstrate reduced but clinically meaningful responses to COVID-19 vaccination. Prevention of bacterial infection, which is a leading cause of morbidity in patients with rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE), is a priority. Pneumococcal vaccination was not associated with an appreciable deterioration in any clinical or laboratory measure of disease activity in either group. One month after vaccination, patients in both groups had significant increases in geometric mean concentrations of pneumococcal polysaccharide-specific IgG to all seven serotypes tested, as did control subjects [44] [45].
Several trials have shown that the vaccine does not induce clinical exacerbation of RA and that it does induce an adequate humoral response, albeit one lower than that in healthy controls. This pattern of preserved safety with reduced but adequate immunogenicity appears consistent across different vaccine types and autoimmune conditions.
Safety Profile and Adverse Events
Overall Safety Assessment
The safety profile of COVID-19 vaccines in immunocompromised populations has been generally favorable. Severe flares and hospitalisation were rare. Thus, vaccination remains safe and highly recommended [46]. This conclusion from the extensive CONVIN-SING study provides reassurance regarding the overall safety profile.
No deaths were recorded after the disease relapsed. At the same time, 4.7% of patients with new-onset conditions died (P = 0.0013) [47] [48], suggesting that vaccine-related autoimmune flares may have a more favorable prognosis than new-onset autoimmune diseases.
According to the criteria for post-vaccine adverse events established by the World Health Organization, a minority of individuals may develop adverse events, including autoimmune syndromes. The exact mechanisms for the development of these autoimmune syndromes are under study, and to date, a cause-and-effect relationship has not been established [49].
Comparison with COVID-19 Infection Risks
When evaluating vaccine safety, it is crucial to consider the comparative risks of SARS-CoV-2 infection itself. Patients with COVID-19 presented an increased risk of developing pernicious anaemia [adjusted Hazard Ratio (aHR): 1.72; 95% Confidence Interval (CI): 1.12-2.64]; spondyloarthritis [aHR: 1.32 (95% CI: 1.03-1.69)]; rheumatoid arthritis [aHR: 1.29 (95% CI: 1.09-1.54)]; other autoimmune arthritis [aHR: 1.43 (95% CI: 1.33-1.54)]; psoriasis [aHR: 1.42 (95% CI: 1.13-1.78)]; pemphigoid [aHR: 2.39 (95% CI: 1.83-3.11)]; Graves’ disease [aHR: 1.30 (95% CI: 1.10-1.54)]; anti-phospholipid antibody syndrome [aHR: 2.12 (95% CI: 1.47-3.05)]; immune mediated thrombocytopenia [aHR: 2.1 (95% CI: 1.82-2.43)]; multiple sclerosis [aHR: 2.66 (95% CI: 1.17-6.05)]; vasculitis [aHR: 1.46 (95% CI: 1.04-2.04)]. Among COVID-19 patients, completion of two doses of the COVID-19 vaccine shows a decreased risk of pemphigoid, Graves’ disease, anti-phospholipid antibody syndrome, immune-mediated thrombocytopenia, systemic lupus erythematosus, and other autoimmune arthritis [50].
This data suggests that SARS-CoV-2 infection itself carries substantial risks for triggering autoimmune diseases, and that vaccination may provide protective effects against some of these autoimmune complications.
Clinical Implications and Recommendations
Individualized Risk Assessment
The decision to vaccinate patients with autoimmune diseases requires individualized assessment considering multiple factors. While additional data is needed to determine the effects of immunocompromising medical conditions and immunosuppressing medications on the efficacy of the vaccine, the benefits of vaccination are anticipated to outweigh theoretical risks. While additional data is needed to determine the effects of immunocompromising medical conditions and immunosuppressing medications on the efficacy of the vaccine, the benefits of vaccination are anticipated to outweigh theoretical risks [51] [52].
Patients with AIADs, PIDs, and SIDs: (1) Do not present contraindications to COVID-19 vaccines if an mRNA vaccine is used and administered in a stabilized disease phase without active infection. (2) Should usually not discontinue immunosuppressive therapy, which may be modulated depending on the patient’s clinical condition. (3) When eligible, should have priority access to vaccination [53].
Timing Considerations
The timing of vaccination relative to disease activity and immunosuppressive therapy represents a critical clinical consideration. Disease stability appears to be a key factor in optimizing both safety and efficacy. Twenty-four patients with low and/or stable disease activity 14 with SLE (mean age 43.42+/-12.18 years; 13 women) and 10 with RA (mean age 51+/-14.57 years; 9 women), diagnosed based on the American College of Rheumatology criteria, have been immunized with trivalent split influenza vaccine without adjuvant [54] demonstrates the historical approach of vaccinating during stable disease periods.
Monitoring and Management
Post-vaccination monitoring strategies should be tailored to individual patient risk profiles. These reports could help guide clinical assessment and management of autoimmune manifestations after COVID-19 vaccination. These reports could help guide clinical assessment and management of autoimmune manifestations after COVID-19 vaccination [55] [56].
Healthcare providers should be aware of the temporal relationship between vaccination and potential flares, with most occurring within the first two weeks. There was a moderately high rate of AIIRD flares after mRNA vaccination, but also improvement in several patients [57], suggesting that some patients may experience disease improvement following vaccination.
Limitations and Future Directions
Current Knowledge Gaps
Several significant limitations exist in the current evidence base. However, whether the association between the COVID-19 vaccine and autoimmune manifestations is coincidental or causal remains to be elucidated. Although information about the risk of autoimmune disease as a consequence of vaccination is controversial, we merely propose our current understanding of autoimmune manifestations associated with the COVID-19 vaccine. We do not aim to disavow the overwhelming benefits of mass COVID-19 vaccination in preventing COVID-19 morbidity and mortality [58] [59].
Nevertheless, the causal relationship between COVID-19 vaccines and these autoimmune diseases remains to be demonstrated. Whether there is a causal relationship between COVID-19 vaccination and these autoimmune phenomena needs to be further explored [60] [61].
Areas for Future Research
Future avenues include exploring flare profiles and optimizing vaccine strategies for this group [62]. Additional research priorities include:
- Long-term follow-up studies to assess the durability of vaccine protection in immunocompromised populations
- Mechanistic studies to better understand the pathophysiology of vaccine-induced autoimmune phenomena
- Development of predictive biomarkers to identify patients at the highest risk for post-vaccination flares
- Optimization of vaccination timing relative to immunosuppressive therapy cycles
- Investigation of novel vaccine platforms that may provide improved safety profiles in autoimmune populations
In future pandemics, including vulnerable populations (VPs) in vaccine and monoclonal antibody (mAb) trials is crucial to develop safe, effective immunization strategies, address gaps in vaccine efficacy and safety data, and create tailored guidelines for at-risk groups. In future pandemics, including vulnerable populations (VPs) in vaccine and monoclonal antibody (mAb) trials is crucial to develop safe, effective immunization strategies, address gaps in vaccine efficacy and safety data, and create tailored guidelines for at-risk groups [63] [64].
Discussion
The evidence presented in this analysis reveals a nuanced picture of COVID-19 vaccination in patients with autoimmune diseases. While the risk of post-vaccination flares is real and clinically significant, occurring in approximately 10-18% of patients with autoimmune inflammatory rheumatic diseases, the majority of these flares are mild to moderate in severity and manageable with standard therapeutic approaches.
The protective benefits of vaccination appear to outweigh the risks of autoimmune flares substantially. COVID-19 vaccines demonstrate meaningful efficacy against severe outcomes even in immunocompromised populations, with vaccine effectiveness ranging from 64-90% against SARS-CoV-2 infection and 70-100% against severe illness. The reduced immunogenicity observed in these populations is offset by the significant morbidity and mortality reduction achieved through vaccination.
The mechanistic understanding of vaccine-induced autoimmune phenomena continues to evolve. Molecular mimicry, bystander activation, and adjuvant effects represent plausible pathways through which vaccination might trigger autoimmune responses. However, it is essential to note that SARS-CoV-2 infection itself carries substantial risks for triggering autoimmune diseases, often exceeding the risks associated with vaccination.
The temporal relationship between vaccination and autoimmune flares, with most occurring within 2 weeks of immunization, supports a causal relationship in at least some cases. However, the observation that some patients experience disease improvement following vaccination suggests that the immune stimulation provided by vaccines may have variable effects on underlying autoimmune processes.
Clinical decision-making should be individualized, considering factors such as disease activity, immunosuppressive medication regimens, local COVID-19 epidemiology, and patient preferences. The concept of shared decision-making becomes particularly important in this context, where patients and providers must weigh complex risk-benefit considerations.
The success of additional vaccine doses in improving protection among immunocompromised patients supports current recommendations for enhanced vaccination schedules in this population. The data suggesting that fourth doses provide meaningful protection against infection, hospitalization, and death reinforces the importance of following updated vaccination guidelines.

Conclusion 
This comprehensive analysis of autoimmunity and COVID-19 vaccines reveals that while the risk of vaccine-induced autoimmune flares exists and should not be dismissed, the protective benefits of vaccination substantially outweigh these risks in most patients with autoimmune diseases. The evidence supports current recommendations for COVID-19 vaccination in immunocompromised populations, with appropriate modifications for enhanced protection through additional doses.
Key findings include:
- Flare Incidence: Autoimmune disease flares occur in approximately 10-18% of patients following COVID-19 vaccination, with most being mild to moderate in severity.
- Protective Efficacy: Despite reduced immunogenicity, COVID-19 vaccines provide meaningful protection against severe COVID-19 outcomes in immunocompromised patients, with effectiveness ranging from 64-90% against infection and 70-100% against severe illness.
- Mechanistic Understanding: Molecular mimicry, bystander activation, and adjuvant effects represent plausible mechanisms for vaccine-induced autoimmune phenomena, though causality remains incompletely established.
- Risk-Benefit Balance: The comparative analysis strongly favors vaccination, as SARS-CoV-2 infection itself carries substantial risks for triggering autoimmune diseases that often exceed vaccination-related risks.
- Clinical Approach: Individualized risk assessment considering disease activity, immunosuppressive therapy, and patient-specific factors remains essential for optimal outcomes.
The evolving evidence base continues to support the fundamental principle that the benefits of COVID-19 vaccination in patients with autoimmune diseases outweigh the risks. Healthcare providers should maintain confidence in recommending vaccination while remaining vigilant for post-vaccination flares and prepared to manage them appropriately when they occur.
Future research should focus on optimizing vaccination strategies for immunocompromised populations, developing predictive biomarkers for flare risk, and ensuring that vulnerable populations are included in future vaccine development programs. The lessons learned from the COVID-19 pandemic will prove invaluable for managing future infectious disease threats in patients with autoimmune conditions.
As the pandemic continues to evolve and new variants emerge, the importance of maintaining high vaccination rates in vulnerable populations cannot be overstated. The current evidence provides a strong foundation for continuing to recommend COVID-19 vaccination in patients with autoimmune diseases, with appropriate clinical monitoring and individualized care approaches.
References:
- Guo, M., Liu, X., Chen, X., & Li, Q. (2023). Insights into new-onset autoimmune diseases after COVID-19 vaccination. Autoimmunity Reviews, 22(7), 103340. https://doi.org/10.1016/j.autrev.2023.103340
- Chen, Y., Xu, Z., Wang, P., Li, X. M., Shuai, Z. W., Ye, D. Q., & Pan, H. F. (2022). New-onset autoimmune phenomena post-COVID-19 vaccination. Immunology, 165(4), 386-401. https://doi.org/10.1111/imm.13443
- Ma, M., Santosa, A., Fong, W., et al. (2023). Post-mRNA vaccine flares in autoimmune inflammatory rheumatic diseases: Results from the COronavirus National Vaccine registry for ImmuNe diseases SINGapore (CONVIN-SING). Journal of Autoimmunity, 134, 102959. https://doi.org/10.1016/j.jaut.2022.102959
- Naveen, R., Nikiphorou, E., Joshi, M., et al. (2023). Flares in autoimmune rheumatic diseases in the post-COVID-19 vaccination period-a cross-sequential study based on COVAD surveys. International Journal of Rheumatic Diseases, 27(1), e14961. https://doi.org/10.1111/1756-185X.14961
- Furer, V., Eviatar, T., Zisman, D., et al. (2022). Autoimmune and autoinflammatory conditions after COVID-19 vaccination. New case reports and updated literature review. Journal of Autoimmunity, 132, 102898. https://doi.org/10.1016/j.jaut.2022.102898
- Braverman, G., Barbhaiya, M., Nong, M., & Mandl, L. A. (2025). Flares of Systemic Autoimmune Rheumatic Disease Following Coronavirus Disease 2019 Vaccination: A Narrative Review. Rheumatic Disease Clinics of North America, 51(1), 75-92. https://doi.org/10.1016/j.rdc.2024.08.005
- Chang, R., Yen-Ting Chen, T., Wang, S. I., et al. (2023). Risk of autoimmune diseases following COVID-19 and the potential protective effect from vaccination: a population-based cohort study. eClinicalMedicine, 63, 102177. https://doi.org/10.1016/j.eclinm.2023.102177
- Izmirly, P. M., Kim, M. Y., Samanovic, M., et al. (2022). Effect of Systemic Lupus Erythematosus and Immunosuppressive Agents on COVID-19 Vaccination Antibody Response. Arthritis & Rheumatology, 74(2), 284-294. https://doi.org/10.1002/art.41937
- Rodríguez, Y., Novelli, L., Rojas, M., et al. (2020). Autoinflammatory and autoimmune conditions at the crossroad of COVID-19. Journal of Autoimmunity, 114, 102506. https://doi.org/10.1016/j.jaut.2020.102506
- Salemi, S., & D’Amelio, R. (2010). Could autoimmunity be induced by vaccination? International Reviews of Immunology, 29(3), 247-269. https://doi.org/10.3109/08830181003746304
Within article:
[1] Insights into new-onset autoimmune diseases after COVID-19 vaccination – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/37075917/
[2] Insights into new-onset autoimmune diseases after COVID-19 vaccination – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/37075917/
[3] Effectiveness of a fourth dose of COVID-19 mRNA vaccine in patients with systemic autoimmune rheumatic diseases using disease-modifying anti-rheumatic drugs: an emulated target trial – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S2665991323002722
[4] Molecular mimicry and autoimmunity – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0896841118305365
[5] Molecular/antigenic mimicry and immunological crossreactivity explains SARS-CoV-2-induced autoimmunity – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S1568997225000710
[6] Could autoimmunity be induced by vaccination? – PubMed – pubmed.ncbi.nlm.nih.govhttps://pubmed.ncbi.nlm.nih.gov/20521925/?dopt=Abstract
[7] New-onset autoimmune phenomena post-COVID-19 vaccination – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34957554/
[8] New-onset autoimmune phenomena post-COVID-19 vaccination – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34957554/
[9] Autoimmune response after SARS-CoV-2 infection and SARS-CoV-2 vaccines – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S1568997223002422
[10] Insights into new-onset autoimmune diseases after COVID-19 vaccination – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/37075917/
[11] Bystander activation and autoimmunity – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31326230/
[12] Bystander activation and autoimmunity – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31326230/
[13] Safety of vaccine adjuvants: Focus on autoimmunity – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0264410X15001309
[14] Safety of vaccine adjuvants: Focus on autoimmunity – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0264410X15001309
[15] Acquired autoimmunity after viral vaccination is caused by molecular mimicry and antigen complimentarity in the presence of an immunologic adjuvant and specific HLA patterns – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/17630224/
[16] Bystander activation and autoimmunity – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31326230/
[17] Immunological and clinical efficacy of COVID-19 vaccines in immunocompromised populations: a systematic review – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S1198743X21005668
[18] Immunological and clinical efficacy of COVID-19 vaccines in immunocompromised populations: a systematic review – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S1198743X21005668
[19] Post-mRNA vaccine flares in autoimmune inflammatory rheumatic diseases: Results from the COronavirus National Vaccine registry for ImmuNe diseases SINGapore (CONVIN-SING) – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0896841122001676
[20] Post-mRNA vaccine flares in autoimmune inflammatory rheumatic diseases: Results from the COronavirus National Vaccine registry for ImmuNe diseases SINGapore (CONVIN-SING) – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0896841122001676
[21] Post-mRNA vaccine flares in autoimmune inflammatory rheumatic diseases: Results from the COronavirus National Vaccine registry for ImmuNe diseases SINGapore (CONVIN-SING) – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0896841122001676
[22] Flares in autoimmune rheumatic diseases in the post-COVID-19 vaccination period-a cross-sequential study based on COVAD surveys – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36961331/
[23] Autoimmune and autoinflammatory conditions after COVID-19 vaccination. New case reports and updated literature review – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0896841122001068
[24] Post-mRNA vaccine flares in autoimmune inflammatory rheumatic diseases: Results from the COronavirus National Vaccine registry for ImmuNe diseases SINGapore (CONVIN-SING) – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0896841122001676
[25] Autoimmune and autoinflammatory conditions after COVID-19 vaccination. New case reports and updated literature review – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0896841122001068
[26] New-onset autoimmune phenomena post-COVID-19 vaccination – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34957554/
[27] New-onset autoimmune phenomena post-COVID-19 vaccination – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34957554/
[28] Autoimmune and autoinflammatory conditions after COVID-19 vaccination. New case reports and updated literature review – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0896841122001068
[29] Immunogenicity and safety of pneumococcal vaccination in patients with rheumatoid arthritis or systemic lupus erythematosus – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/11740700/
[30] Immunogenicity and safety of pneumococcal vaccination in patients with rheumatoid arthritis or systemic lupus erythematosus – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/11740700/
[31] The Use of COVID-19 Vaccines in Patients with SLE – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34767100/
[32] Influenza vaccine administration in patients with systemic lupus erythematosus and rheumatoid arthritis. Safety and immunogenicity – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/16466833/
[33] Influenza vaccine administration in patients with systemic lupus erythematosus and rheumatoid arthritis. Safety and immunogenicity – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/16466833/
[34] COVID-19 vaccine effectiveness among immunocompromised populations: a targeted literature review of real-world studies – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35112973/
[35] Short-term effectiveness of COVID-19 vaccines in immunocompromised patients: A systematic literature review and meta-analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34982962/
[36] Vaccination of the immune-compromised patients with focus on patients with autoimmune-inflammatory diseases – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/21325695/
[37] Vaccination of the immune-compromised patients with focus on patients with autoimmune-inflammatory diseases – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/21325695/
[38] Vaccination of the immune-compromised patients with focus on patients with autoimmune-inflammatory diseases – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/21325695/
[39] Efficacy, immunogenicity, and safety of the Novavax COVID-19 vaccine in immunocompromised patients: A targeted literature review – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/39892114/
[40] Efficacy, immunogenicity, and safety of the Novavax COVID-19 vaccine in immunocompromised patients: A targeted literature review – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/39892114/
[41] Safety and efficacy of vaccination against streptococcus pneumonia in patients with rheumatic diseases – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/17412304/
[42] Safety and efficacy of vaccination against streptococcus pneumonia in patients with rheumatic diseases – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/17412304/
[43] Influenza vaccination in patients with rheumatic diseases. Safety and efficacy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/312949/
[44] Effect of Systemic Lupus Erythematosus and Immunosuppressive Agents on COVID-19 Vaccination Antibody Response – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36714913/
[45] Effect of Systemic Lupus Erythematosus and Immunosuppressive Agents on COVID-19 Vaccination Antibody Response – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36714913/
[46] Post-mRNA vaccine flares in autoimmune inflammatory rheumatic diseases: Results from the COronavirus National Vaccine registry for ImmuNe diseases SINGapore (CONVIN-SING) – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0896841122001676
[47] Autoimmune and autoinflammatory conditions after COVID-19 vaccination. New case reports and updated literature review – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0896841122001068
[48] Autoimmune and autoinflammatory conditions after COVID-19 vaccination. New case reports and updated literature review – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0896841122001068
[49] Effectiveness of a fourth dose of COVID-19 mRNA vaccine in patients with systemic autoimmune rheumatic diseases using disease-modifying anti-rheumatic drugs: an emulated target trial – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S2665991323002722
[50] Risk of autoimmune diseases following COVID-19 and the potential protective effect from vaccination: a population-based cohort study – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/37637754/
[51] Shielding the immunocompromised: COVID-19 prevention strategies for patients with primary and secondary immunodeficiencies – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0264410X25001501
[52] Shielding the immunocompromised: COVID-19 prevention strategies for patients with primary and secondary immunodeficiencies – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0264410X25001501
[53] Vaccine-induced autoimmunity: the role of molecular mimicry and immune crossreaction – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/29503439/
[54] Influenza vaccination in patients with rheumatic diseases. Safety and efficacy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/312949/
[55] SARS-CoV-2 vaccines and autoimmune diseases amidst the COVID-19 crisis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33515320/
[56] SARS-CoV-2 vaccines and autoimmune diseases amidst the COVID-19 crisis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33515320/
[57] Post-mRNA vaccine flares in autoimmune inflammatory rheumatic diseases: Results from the COronavirus National Vaccine registry for ImmuNe diseases SINGapore (CONVIN-SING) – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0896841122001676
[58] New-onset autoimmune phenomena post-COVID-19 vaccination – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34957554/
[59] New-onset autoimmune phenomena post-COVID-19 vaccination – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34957554/
[60] Insights into new-onset autoimmune diseases after COVID-19 vaccination – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S1568997223000745
[61] Insights into new-onset autoimmune diseases after COVID-19 vaccination – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S1568997223000745
[62] Flares in autoimmune rheumatic diseases in the post-COVID-19 vaccination period-a cross-sequential study based on COVAD surveys – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36961331/
[63] Systematic lupus erythematous patients following COVID-19 vaccination: Its flares up and precautions – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S2049080122010421
[64] Systematic lupus erythematous patients following COVID-19 vaccination: Its flares up and precautions – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S2049080122010421

