Hidden Signs of GATA2 Deficiency: Why Doctors Miss This Rare Disorder
Introduction
GATA2 deficiency is the most common hereditary predisposition to pediatric myelodysplastic syndrome (MDS), yet it remains one of the most frequently overlooked genetic disorders in clinical practice. This rare, autosomal dominant condition carries a high risk of progression to myeloid malignancies, with a penetrance estimated at 75%. The risk increases sharply with age from 6% by age 10 to 81% by age 40.
Diagnosis is often delayed due to the condition’s broad and variable clinical presentation, which can differ even among affected family members. Common features include:
- Unexplained, multi-lineage cytopenias
- Recurrent or severe infections due to immunodeficiency
- Pulmonary alveolar proteinosis
- Lymphedema and, in some cases, congenital sensorineural deafness
Importantly, GATA2 deficiency is not limited to hematologic abnormalities. Its systemic manifestations can precede cytopenias or evolve independently. Despite the severity of its progression, fewer than 500 cases have been reported globally, and only half demonstrate a clear familial inheritance pattern.
The underdiagnosis is particularly concerning given its strong association with MDS. Notably, 72% of adolescents with MDS and monosomy 7 harbor GATA2 mutations. Overall, GATA2 deficiency accounts for 15% of advanced and 7% of all primary pediatric MDS cases.
Currently, allogeneic hematopoietic stem cell transplantation (HSCT) is the only curative therapy. However, outcomes are notably better when HSCT is performed early—before irreversible complications such as organ dysfunction occur.
Raising clinical awareness and improving early recognition of GATA2 deficiency are critical. Early genetic testing should be considered in any child or adolescent presenting with unexplained cytopenias, recurrent infections, or a family history suggestive of bone marrow failure or myeloid malignancies. Timely diagnosis enables appropriate monitoring and early curative intervention, markedly improving long-term outcomes.

What is GATA2 Deficiency and Why It’s Often Missed
The GATA2 gene encodes a transcription factor essential for normal development and functioning of the hematopoietic system. Unlike many genetic disorders with straightforward clinical presentations, GATA2 deficiency manifests with remarkable heterogeneity, making it a particularly challenging condition to recognize in clinical practice.
GATA2 gene function in hematopoiesis and immunity
GATA2 protein belongs to the zinc finger transcription factor family, primarily expressed in hematopoietic stem cells, progenitors, and myeloid lineages. This master regulator plays a critical role in maintaining the balance between self-renewal and differentiation of hematopoietic stem cells. At the molecular level, GATA2 binds to specific DNA sequences, controlling the expression of genes crucial for blood cell development and immune function.
The expression of GATA2 follows a precise temporal pattern during hematopoiesis. Initially high in early progenitors, its levels gradually decrease as cells differentiate into specific lineages. This carefully orchestrated expression pattern ensures proper development of:
- Monocytes and dendritic cells – critical for innate immunity
- B-lymphocyte precursors – essential for humoral immunity
- Natural killer cells – vital for anti-viral and anti-tumor responses
Additionally, GATA2 interacts with numerous other transcription factors and chromatin modifiers, forming complex regulatory networks that govern hematopoietic stem cell maintenance. When GATA2 function is compromised through mutation, these intricate networks become dysregulated, leading to profound effects across multiple hematopoietic lineages.
Notably, GATA2 also regulates endothelial cell function, which explains why some patients develop lymphatic abnormalities and pulmonary alveolar proteinosis; manifestations outside the hematopoietic system that contribute to the syndromic nature of the disorder.
Why GATA2 deficiency is classified as a syndrome
GATA2 deficiency earns its classification as a syndrome rather than a simple genetic disorder because of its extraordinarily diverse clinical manifestations across multiple organ systems. Though initially recognized through distinct clinical entities—MonoMAC syndrome (monocytopenia with mycobacterial infections), Emberger syndrome (primary lymphedema with myelodysplasia), and familial MDS/AML, these conditions were subsequently discovered to share a common genetic etiology in GATA2 mutations.
The phenotypic spectrum of GATA2 deficiency syndrome encompasses:
- Hematologic abnormalities: Cytopenias affecting one or multiple lineages, bone marrow failure, and predisposition to myeloid malignancies
- Immunologic defects: Susceptibility to atypical infections, particularly mycobacterial, fungal, and viral pathogens
- Pulmonary manifestations: Alveolar proteinosis and recurrent pneumonia
- Vascular/lymphatic issues: Primary lymphedema, especially of lower extremities
- Dermatologic features: Unusual wart presentations and panniculitis
- Otolaryngologic findings: Sensorineural hearing loss in some cases
The age of onset and severity vary considerably, even among family members carrying identical mutations, suggesting influence from genetic modifiers and environmental factors. This clinical heterogeneity underscores why GATA2 deficiency represents a true syndrome rather than a single-manifestation disorder.
Lack of awareness among general practitioners
Despite its implications for patient management, GATA2 deficiency remains largely unfamiliar to many primary care physicians and even some specialists. Several factors contribute to this diagnostic blind spot.
First, the rarity of the condition means most physicians may never encounter a case during their career, leading to limited experience in recognizing its subtle patterns. Since individual manifestations often mimic more common conditions, practitioners typically pursue diagnostic pathways aligned with these familiar disorders instead.
Second, medical education and continuing medical education programs frequently underemphasize rare genetic disorders, particularly those discovered relatively recently. Consequently, physicians may not include GATA2 deficiency in their differential diagnoses when evaluating patients with relevant symptoms.
Third, the insidious onset and seemingly unrelated manifestations create a fragmented clinical picture that may be addressed by different specialists who fail to connect the dots. A patient might see a dermatologist for warts, a hematologist for unexplained cytopenia, and a pulmonologist for respiratory symptoms, each specialist treating their respective concern without recognizing the underlying syndrome.
Fourth, without specific alerting features or pathognomonic findings, distinguishing GATA2 deficiency from more common conditions requires a high index of suspicion. The diagnosis often emerges only after multiple treatment failures or unusual clinical courses prompt genetic testing.
Lastly, the absence of routine screening for GATA2 mutations in patients with cytopenias, immunodeficiency, or early-onset myelodysplasia contributes to diagnostic delays. Unless specifically considered and tested for, GATA2 deficiency will continue to be overlooked until complications develop or malignant transformation occurs—at which point treatment options become more limited and outcomes potentially less favorable.
Early Symptoms That Don’t Raise Red Flags
Patients with GATA2 deficiency often present with deceptively common symptoms that frequently lead physicians down incorrect diagnostic pathways. These subtle clinical manifestations can persist for years before the underlying genetic disorder is identified, creating a dangerous diagnostic delay.
Persistent warts and HPV-related lesions
Human papillomavirus (HPV) manifestations in GATA2 deficiency extend beyond typical presentations and represent a vital diagnostic clue frequently overlooked. These lesions typically exhibit:
- Unusual persistence despite conventional treatments
- Atypical distribution patterns, often involving non-genital sites
- Progressive spread despite intervention
- Early onset in adolescence or young adulthood
Remarkably, the HPV-related complications seen in GATA2 deficiency differ from those in other immunodeficiencies. The warts are often extensive and recalcitrant, while HPV-related dysplasia progresses more rapidly to neoplasia. This accelerated progression reflects the unique immunologic defects in dendritic cell and NK cell function characteristic of this disorder.
Dermatologic manifestations may also include panniculitis, erythema nodosum, and Sweet syndrome; inflammatory conditions that physicians rarely connect to an underlying genetic disorder. Unfortunately, many practitioners attribute persistent HPV infections to environmental factors or mild immunosuppression rather than considering a primary immunodeficiency syndrome.
Mild cytopenias without clear cause
Subtle blood count abnormalities often represent the earliest hematologic signs of GATA2 deficiency but frequently go unrecognized as such. These include:
- Monocytopenia (often the earliest and most consistent finding)
- Neutropenia (mild to moderate)
- B and NK lymphocytopenia
- Occasional thrombocytopenia or anemia
What makes these findings particularly challenging to recognize is their:
- Gradual onset over years
- Fluctuating severity, with periods of near-normal counts
- Initial absence of clinical symptoms despite laboratory abnormalities
- Subtle degree of cytopenia that doesn’t trigger immediate concern
Certainly, many clinicians interpret isolated mild cytopenias as laboratory error, transient viral suppression, or idiopathic findings. The absence of pronounced symptoms in early stages further diminishes clinical suspicion. Meanwhile, the monocytopenia—arguably the most specific finding—is easily overlooked during routine complete blood count interpretation, as practitioners typically focus more on neutrophil, platelet, and hemoglobin values.
Crucially, these hematologic abnormalities typically precede the development of myelodysplastic syndrome or acute myeloid leukemia by several years, representing a missed opportunity for early intervention.
Recurrent sinus or skin infections
The infectious manifestations of GATA2 deficiency often mimic common community-acquired infections but exhibit subtle distinguishing features:
- Disproportionate severity relative to immunocompetent individuals
- Incomplete response to standard antimicrobial courses
- Involvement of atypical pathogens, particularly nontuberculous mycobacteria
- Recurrence despite adequate treatment
- Predominance of respiratory tract involvement
While severe infections eventually prompt immunologic evaluation, milder recurrent infections are frequently dismissed as bad luck or environmental exposure. Interestingly, the infection pattern in GATA2 deficiency differs from that seen in neutropenia alone, reflecting the complex immunologic defects beyond simple cell count reductions.
Respiratory infections deserve special attention as they may represent the first clinical manifestation of pulmonary alveolar proteinosis—a serious complication of GATA2 deficiency. Early respiratory symptoms may include:
- Exertional dyspnea initially attributed to deconditioning
- Nonproductive cough resistant to conventional treatments
- Recurrent “pneumonia” with incomplete radiographic resolution
- Disproportionate fatigue following respiratory infections
Moreover, susceptibility to herpes family viruses, particularly HPV and EBV, stands in contrast to the preservation of antibody-mediated immunity. This distinctive pattern of susceptibility provides another subtle diagnostic clue that can help distinguish GATA2 deficiency from other immunodeficiency syndromes.
The nonspecific nature of these early manifestations, combined with their occurrence in isolation before the full syndrome develops, creates a perfect storm for diagnostic oversight. Essentially, each symptom appears attributable to common conditions until the constellation becomes apparent—typically after irreversible complications have developed.

Overlapping Diagnoses That Delay Detection
Diagnosing GATA2 deficiency presents a considerable clinical challenge, as its manifestations often mimic more common hematologic and immunologic conditions. This diagnostic complexity frequently leads to treatment delays, inappropriate therapies, and missed opportunities for early intervention.
Misdiagnosis as aplastic anemia or idiopathic cytopenia
The bone marrow failure pattern in GATA2 deficiency commonly resembles idiopathic aplastic anemia (AA), creating a major diagnostic pitfall. Both conditions share several clinical features:
- Peripheral blood cytopenias
- Bone marrow hypocellularity
- History of recurrent infections
- Initial absence of dysplastic features
A study of GATA2-deficient patients revealed that a substantial subset had previously received an AA diagnosis based solely on cytopenias and hypocellular bone marrow biopsies. This confusion occurs primarily because early-stage GATA2 deficiency may present with pancytopenia without clinically evident immunodeficiency.
Nevertheless, critical differences exist. The marrow of GATA2 patients typically shows severely reduced monocytes, B cells, and NK cells; absent hematogones; and inverted CD4:CD8 ratios. Atypical megakaryocytes and abnormal cytogenetics appear more frequently in GATA2-related marrow disorders than in true AA.
Idiopathic cytopenia of undetermined significance (ICUS) represents another common misdiagnosis. ICUS diagnostic criteria include cytopenia persistent for at least 6 months, no dysplastic morphology, normal karyotype, and absence of any underlying disorder. Patients with GATA2 deficiency often initially fulfill these criteria before developing more characteristic features.
Most concerning, inappropriate treatments often follow these misdiagnoses. Current management protocols for acquired AA include immunosuppressive regimens, which may be contraindicated for constitutional bone marrow failure diseases like GATA2 deficiency. This treatment mismatch can worsen outcomes and delay appropriate intervention.
Confusion with autoimmune disorders
Autoimmune manifestations frequently complicate the GATA2 deficiency clinical picture, leading physicians down incorrect diagnostic pathways. The disorder can present with:
- Lupus-like symptoms
- Autoimmune hepatitis
- Sarcoidosis-like presentations
- Sweet’s syndrome and panniculitis
- Immune thrombocytopenia-like manifestations
According to published case series, autoimmune or chronic inflammatory disorders represent recurrent features in GATA2 deficiency. Interestingly, serologic testing often shows positive autoimmune markers, reinforcing the initial misdiagnosis.
This diagnostic confusion arises from the complex immune dysregulation in GATA2 deficiency. While primarily characterized by immunodeficiency, paradoxical immune hyperactivity occurs in some patients, presumably due to disrupted immune regulatory mechanisms. Hence, some patients receive immunosuppressive treatments for presumed primary autoimmune conditions, potentially exacerbating their underlying immune defect.
A mild defect in immunoglobulin production or weak vaccinal response has also been reported in GATA2 deficiency, further complicating the clinical picture. Consequently, autoimmune manifestations may represent the predominant clinical feature for years before more characteristic GATA2-related symptoms emerge.
Overlap with common variable immunodeficiency (CVID)
Common variable immunodeficiency shares multiple clinical features with GATA2 deficiency syndrome, creating another diagnostic challenge. Both conditions feature:
- Recurrent bacterial infections, often respiratory
- Late-onset presentation compared to other primary immunodeficiencies
- Variable clinical penetrance even within families
- Heterogeneous genetic basis
CVID is characterized by hypogammaglobulinemia, poor antibody response to vaccines, and recurrent infections that cannot be explained by previous exposures or treatments. Some patients also develop autoimmunity, granulomatous disease, or cancer—features that overlap with GATA2 deficiency.
Whereas CVID typically preserves normal B cell numbers while lacking plasma cells, GATA2 deficiency shows marked reduction in B-cell precursors. Additionally, GATA2 deficiency typically presents with monocytopenia and preserved immunoglobulin levels—a pattern distinct from classic CVID.
Ultimately, distinction between these conditions requires thorough immunophenotyping and genetic analysis. Despite similar clinical presentations, the treatment approaches differ substantially. CVID management primarily involves immunoglobulin replacement, whereas GATA2 deficiency may eventually require hematopoietic stem cell transplantation.
Given these overlapping features, accurate diagnosis requires heightened clinical suspicion and appropriate genetic testing. Data reveals a distinctly high rate of diagnostic errors—approximately 40% of patients initially diagnosed with MDS were subsequently found to have incorrect diagnoses upon expert review.
Hidden Clues in Blood and Bone Marrow
Laboratory analysis often reveals subtle yet distinctive abnormalities in GATA2 deficiency long before overt clinical symptoms emerge. These hematologic fingerprints, when properly identified, can substantially expedite diagnosis and appropriate intervention.
Monocytopenia with preserved immunoglobulin levels
The most striking laboratory finding in GATA2 deficiency syndrome is profound peripheral blood monocytopenia, observed in approximately 78% of affected individuals. Absolute monocyte counts typically fall below 100 cells/microliter, a level much lower than seen in other conditions associated with decreased monocytes such as hairy cell leukemia.
Paradoxically, despite marked B-lymphocytopenia, immunoglobulin levels remain normal or even elevated. This unusual combination creates a distinctive laboratory profile:
- Severe monocytopenia with preserved tissue macrophages
- Normal or elevated immunoglobulin levels despite B-cell deficiency
- Polyclonal plasma cells remain abundant in bone marrow
This phenomenon likely reflects the preservation of long-lived plasma cells alongside persistent defects in monocyte production. Importantly, this pattern distinguishes GATA2 deficiency from common variable immunodeficiency, where hypogammaglobulinemia typically accompanies B-cell abnormalities.
Loss of dendritic cells and B-cell precursors
Flow cytometric analysis of bone marrow and peripheral blood provides crucial diagnostic clues that often go unnoticed during routine evaluation. Beyond monocytopenia, GATA2-deficient patients exhibit a characteristic pattern of cellular deficiencies.
In the bone marrow, B-cell progenitors (defined as CD19+CD10+CD34+) are markedly reduced or absent. This finding corresponds with diminished intronRSS-Kde recombination excision circles, a marker for de novo B-cell production. First, CD56bright NK cells virtually disappear, followed by progressive loss of naive B cells, with a relative increase in memory B-cell populations.
Although T-cell numbers typically remain less affected, careful analysis often reveals inversion of CD4:CD8 ratios. Dendritic cell populations, particularly plasmacytoid dendritic cells, show consistent depletion in nearly all cases.
The disproportionate loss of these immune populations can be detected using routine clinical flow cytometry panels. In fact, this pattern helps differentiate GATA2 deficiency from idiopathic aplastic anemia, which typically shows preservation of immune populations reflecting its immunologic basis.
Hypocellular marrow with multilineage dysplasia
Bone marrow examination in GATA2 deficiency generally reveals hypocellular marrow with distinctive morphologic abnormalities. Approximately 84% of patients meet diagnostic criteria for myelodysplastic syndrome, primarily showing multilineage dysplasia with blasts below 5%.
Megakaryocytic dysplasia presents almost universally (92% of cases), even in patients without overt myelodysplastic syndrome. These abnormalities include separation of nuclear lobes, mononuclear megakaryocytes, and micromegakaryocytes. Additionally, reticulin fibrosis appears in roughly 16% of cases.
Other characteristic findings include:
- Erythroid predominance with inverted myeloid:erythroid ratio
- Dyserythropoiesis with binucleation, nuclear budding, and megaloblastic changes
- Hypogranular and pelgeroid neutrophils reflecting dysmyelopoiesis
- Immunophenotypic dysplasia, including loss of CD38 or aberrant CD7 expression on myeloblasts
Interestingly, despite monocytopenia in circulation, macrophages remain abundant in the marrow as demonstrated by immunohistochemistry for CD68 or CD163. This contradiction provides another subtle diagnostic clue that may trigger suspicion for GATA2 deficiency.
Overall, these marrow findings offer critical diagnostic insights, especially when evaluating GATA2 variants of uncertain significance or assessing patients for potential hematopoietic stem cell transplantation. The presence of these distinctive laboratory abnormalities should prompt consideration of GATA2 deficiency, even before classic clinical manifestations emerge.
Genetic Testing Gaps and Diagnostic Pitfalls
Even with advanced genetic testing technologies, accurate diagnosis of GATA2 deficiency syndrome continues to face substantial technical obstacles. These diagnostic barriers often lead to delayed recognition or complete oversight of this condition in affected individuals.
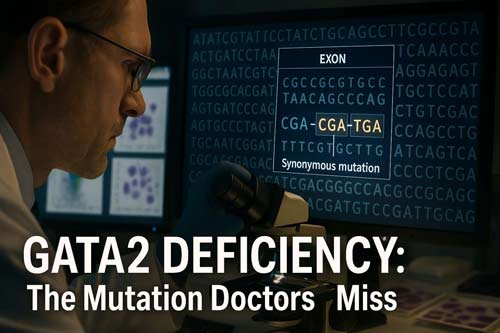
Missed synonymous mutations in GATA2
Synonymous mutations, long considered “silent” due to unchanged amino acid sequences, account for a surprising 8.2% of all GATA2-deficient cases. These variants represent 14.8% of exonic substitutions in GATA2 yet are routinely filtered out during standard genetic analyzes.
Recent studies have identified five distinct synonymous GATA2 variants with profound clinical impact:
- c.351C>G (p.T117T) – the most common, found in multiple families
- c.649C>T (p.L217L)
- c.981G>A (p.G327G)
- c.1023C>T (p.A341A)
- c.1416G>A (p.P472P)
Unlike typical silent mutations, these variants cause selective loss of mutant RNA through various mechanisms. For instance, the c.351C>G mutation activates a cryptic splice site, creating an aberrantly spliced transcript with a 136-bp internal deletion. Other synonymous mutations induce severe RNA loss without disrupting splicing.
Consequently, approximately 5% of individuals with classic GATA2 deficiency clinical presentations show no detectable mutations using standard genetic approaches, highlighting critical gaps in current testing paradigms.
Limitations of exome sequencing without RNA analysis
Whole exome sequencing, while powerful, often misses vital GATA2 variants affecting RNA processing. First, standard pipelines typically exclude intronic regions containing regulatory elements vital for proper gene expression. Second, exome analysis alone cannot detect aberrant splicing caused by synonymous mutations.
RNA sequencing provides essential complementary data, revealing functional consequences of variants otherwise deemed benign. In hereditary cancer testing, paired RNA-DNA analysis detects pathogenic variants in 1 of every 950 patients missed by DNA testing alone. Moreover, RNA evidence resolves variant findings in approximately 1 in 79 patients.
This approach proves particularly valuable for minority populations, where higher rates of variants of uncertain significance exist due to underrepresentation in genomic databases.
Importance of testing non-myeloid tissue for germline confirmation
The distinction between somatic and germline mutations remains important, yet challenging in GATA2 deficiency diagnosis. Blood, bone marrow, and even saliva samples contain hematopoietic cells potentially contaminated by malignant clones.
Furthermore, somatic reversion—where mutations spontaneously correct in blood cells—occurs frequently in GATA2 deficiency. This phenomenon creates false negatives when testing hematopoietic tissues, as the pathogenic variant may disappear from blood cells while remaining present in other tissues.
Thus, non-hematopoietic tissues provide the only reliable source for germline confirmation. Cultured skin fibroblasts represent the gold standard, though hair follicles offer a less invasive alternative. These tissues, derived from different embryological origins than blood cells, provide accurate germline status assessment unaffected by hematologic disease processes.
When to Suspect GATA2 Deficiency Syndrome
Recognizing the clinical constellation that warrants testing for GATA2 deficiency represents a critical step toward timely diagnosis and intervention. Certain presentations, even without overt hematologic malignancy, should prompt consideration of this disorder.
Cytopenia with immunodeficiency in young adults
The combination of unexplained cytopenia and unusual infections in adolescents or young adults constitutes the most common presentation warranting GATA2 testing. Key patterns include:
- Monocytopenia with preserved immunoglobulin levels
- B cell lymphopenia with normal T cell counts
- NK cell depletion
- Recurrent or severe viral infections, primarily HPV and herpesviruses
Typically, symptoms first manifest in late teens or early twenties, with patients developing life-threatening opportunistic infections including nontuberculous mycobacteria, fungi, and recalcitrant HPV. Also, diagnosis delays range from 1-24.5 years after initial presentation, highlighting the need for increased vigilance among clinicians.
Prior to overt disease, distinctive laboratory abnormalities may emerge. In particular, pediatric patients may display monocytosis rather than the monocytopenia characteristically seen in adults with GATA2 deficiency.
Family history of cytopenia or leukemia
Family history provides key diagnostic clues, given that approximately 50% of GATA2 deficiency cases are hereditary. Each child of an affected parent has a 50% chance of inheriting the mutation, yet penetrance remains incomplete.
By age 20, about 50% of mutation carriers develop symptoms, while by age 60, this figure climbs to 95%. Even asymptomatic family members require monitoring, as several cases of unexpected myeloid malignancies have emerged during surveillance of apparently healthy mutation carriers.
First-degree relatives with any of the following should trigger consideration for GATA2 testing:
- Myelodysplastic syndrome, particularly with monosomy 7
- Acute myeloid leukemia before age 40
- Chronic monocytopenia or neutropenia
- Recurrent mycobacterial infections
Presence of Emberger syndrome features
Emberger syndrome—characterized by primary lymphedema, predisposition to myelodysplasia, and hematologic abnormalities—represents a distinct phenotype within the GATA2 deficiency spectrum. Hallmark features include:
- Lymphedema predominantly affecting lower limbs and genitals
- Sensorineural hearing loss
- Predisposition to acute myeloid leukemia
- Severe cutaneous warts
- Inverted CD4:CD8 ratio
The syndrome follows an autosomal dominant inheritance pattern with variable expressivity. In cases of lymphedema coupled with any hematologic abnormality, GATA2 testing should be considered. Given that lymphedema appears in 11-20% of GATA2 patients, its presence alongside any cytopenias or immunodeficiency strongly suggests underlying GATA2 deficiency.

Conclusion
GATA2 deficiency presents a major diagnostic challenge due to its broad clinical spectrum and overlap with more common conditions. This rare genetic disorder can manifest as a puzzling array of symptoms—ranging from persistent cytopenias and severe viral infections to pulmonary disease, lymphedema, and early-onset myeloid malignancies—often leading to delayed or missed diagnoses.
Recognizing key clinical patterns is critical for timely identification:
- Chronic monocytopenia with preserved immunoglobulin levels
- Refractory HPV infections
- Hypocellular bone marrow with megakaryocytic dysplasia
- Family history of early-onset MDS or AML
- Unusual constellations of lymphedema, pulmonary dysfunction, and cytopenias
Despite its rarity, GATA2 deficiency accounts for approximately 72% of adolescent MDS cases with monosomy 7 and 15% of advanced pediatric MDS, emphasizing the need for heightened clinical suspicion and targeted screening in high-risk populations.
Standard genetic testing often fails to detect pathogenic variants, particularly synonymous mutations affecting RNA splicing. When suspicion remains high despite negative results, RNA sequencing and analysis of non-hematopoietic tissues should be pursued for a more accurate diagnosis.
The only curative treatment, allogeneic hematopoietic stem cell transplantation (HSCT), is most effective when performed early, before the onset of severe infections or malignant progression. Delays in diagnosis drastically reduce transplant success and long-term outcomes.
Ultimately, the greatest obstacle is not a lack of treatment options, but failure to recognize the disease. Clinicians must maintain a high index of suspicion when encountering unexplained cytopenias, recurrent infections, or family histories of hematologic malignancies. Early identification enables proactive monitoring, infection prevention, and timely HSCT—interventions that can dramatically alter the disease course.
Improved outcomes depend on multidisciplinary collaboration among hematologists, immunologists, geneticists, dermatologists, and infectious disease specialists. With greater awareness and broader genetic testing strategies, we can reduce diagnostic delays and offer life-saving interventions to those affected by this complex yet treatable disorder.
Frequently Asked Questions:
FAQs
Q1. What are the early signs of GATA2 deficiency that doctors often miss? Early signs include persistent warts or HPV-related lesions, mild unexplained cytopenias, and recurrent sinus or skin infections. These symptoms can be subtle and are often attributed to more common conditions, leading to diagnostic delays.
Q2. How does GATA2 deficiency affect the immune system? GATA2 deficiency impacts multiple aspects of the immune system, causing deficiencies in monocytes, B cells, NK cells, and dendritic cells. This leads to increased susceptibility to certain infections, particularly viral and mycobacterial, while paradoxically preserving immunoglobulin levels.
Q3. Why is GATA2 deficiency often misdiagnosed? GATA2 deficiency is frequently misdiagnosed because its symptoms overlap with more common conditions like aplastic anemia, autoimmune disorders, and common variable immunodeficiency. The rarity of the condition and lack of awareness among general practitioners also contribute to misdiagnosis.
Q4. What genetic testing challenges exist for diagnosing GATA2 deficiency? Challenges include missed synonymous mutations, limitations of exome sequencing without RNA analysis, and the importance of testing non-myeloid tissue for germline confirmation. These factors can lead to false negatives in genetic testing, even when clinical suspicion is high.
Q5. When should a doctor suspect GATA2 deficiency syndrome? Doctors should suspect GATA2 deficiency in young adults with unexplained cytopenias and immunodeficiency, individuals with a family history of early-onset myeloid malignancies or cytopenias, and patients presenting with features of Emberger syndrome (lymphedema, predisposition to myelodysplasia, and severe warts).
References:
[1] – https://pmc.ncbi.nlm.nih.gov/articles/PMC4281830/
[2] – https://pubmed.ncbi.nlm.nih.gov/25359990/
[3] – https://pmc.ncbi.nlm.nih.gov/articles/PMC6803162/
[4] – https://pmc.ncbi.nlm.nih.gov/articles/PMC6068047/
[5] – https://www.acpjournals.org/doi/10.7326/aimcc.2022.1087
[6] – https://www.nejm.org/doi/full/10.1056/NEJMoa1512234
[7] – https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-018-0127-x
[8] – https://consultqd.clevelandclinic.org/national-data-show-misdiagnoses-common-for-patients-with-myelodysplastic-syndromes
[9] – https://ashpublications.org/blood/article/123/6/809/32599/GATA2-deficiency-a-protean-disorder-of
[10] – https://www.verywellhealth.com/monocytopenia-5219343
[11] – https://haematologica.org/article/view/6030
[12] – https://ashpublications.org/blood/article/141/13/1524/493407/The-spectrum-of-GATA2-deficiency-syndrome
[13] – https://www.merckmanuals.com/professional/hematology-and-oncology/leukopenias/monocytopenia
[14] – https://pmc.ncbi.nlm.nih.gov/articles/PMC5013954/
[15] – https://pubmed.ncbi.nlm.nih.gov/27013649/
[16] – https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.865773/full
[17] – https://haematologica.org/article/view/7736
[18] – https://pmc.ncbi.nlm.nih.gov/articles/PMC5087571/
[19] – https://pmc.ncbi.nlm.nih.gov/articles/PMC2830758/
[20] – https://www.pathologyoutlines.com/topic/myeloproliferativeRCMD.html
[21] – https://pubmed.ncbi.nlm.nih.gov/32555368/
[22] – https://www.nature.com/articles/s41375-020-0899-5
[23] – https://ashpublications.org/blood/article/132/11/1211/39369/A-novel-disease-causing-synonymous-exonic-mutation
[24] – https://www.niaid.nih.gov/sites/default/files/GATA2-Factsheet.pdf
[25] – https://www.insideprecisionmedicine.com/news-and-features/pairing-rna-and-dna-more-accurate-for-hereditary-cancer-testing/
[26] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10625669/
[27] – https://ascopubs.org/doi/10.1200/EDBK_432218
[28] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9923095/
[29] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10582742/

