Investigating the Rapid Rise in Early-Onset Cancer Incidence Among Adolescents and Adults Under 50 in the United States: Trends, Risk Factors, Screening Gaps, Environmental Exposures, Lifestyle Drivers, and Implications for Prevention and Public Health Policy
Abstract
The incidence of early-onset cancer among individuals under 50 years has increased dramatically over the past three decades in the United States. This phenomenon represents a critical public health challenge that demands immediate attention from healthcare providers, policymakers, and researchers. This analysis examines current epidemiological trends, identifies potential risk factors, evaluates screening inadequacies, and explores environmental and lifestyle contributors to this alarming increase.
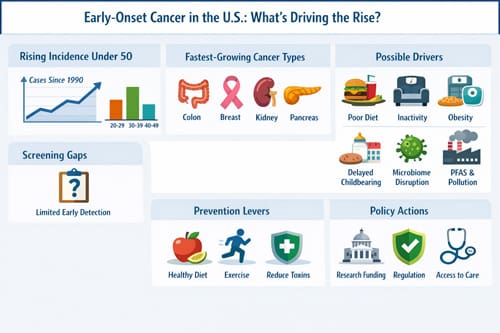
Recent studies indicate that cancer rates among adults aged 20-49 have risen by approximately 15% since 1990, with particular increases observed in colorectal, breast, kidney, and pancreatic cancers. Multiple factors contribute to this trend, including dietary changes, sedentary lifestyles, environmental toxin exposure, altered gut microbiomes, and delayed childbearing patterns. Additionally, current screening protocols fail to address the unique needs of younger populations, creating dangerous gaps in early detection.
This paper synthesizes available evidence to provide clinicians with practical insights for patient care, discusses policy implications for prevention strategies, and identifies areas requiring urgent research attention. The findings suggest that traditional age-based screening guidelines may need revision, and public health initiatives must adapt to address the specific risk factors affecting younger populations.
Recent articles. Check out our extensive video library.
Introduction
Cancer has traditionally been viewed as a disease of aging, with most diagnoses occurring after age 65. However, this paradigm is shifting as mounting evidence reveals a troubling increase in cancer incidence among younger adults and adolescents. The term “early-onset cancer” typically refers to malignancies diagnosed before age 50, though some researchers use age 40 as a cutoff depending on cancer type.
The clinical implications of this trend extend beyond mere statistics. Young cancer patients face unique challenges including fertility preservation concerns, career disruption, family planning decisions, and different treatment tolerances compared to older patients. Furthermore, early-onset cancers may exhibit distinct biological characteristics, potentially requiring modified therapeutic approaches.
Understanding the drivers behind this increase is essential for developing effective prevention strategies and updating clinical protocols. The multifactorial nature of cancer development suggests that no single cause explains this phenomenon. Instead, a complex interplay of genetic, environmental, and lifestyle factors appears to be creating conditions that favor earlier cancer development.
This investigation aims to provide healthcare professionals with evidence-based insights into early-onset cancer trends while identifying actionable strategies for patient care and public health intervention. The urgency of this issue cannot be overstated, as current generations of young adults may face unprecedented cancer risks that existing healthcare systems are inadequately prepared to address.
Current Epidemiological Trends
Overall Incidence Patterns
Data from the Surveillance, Epidemiology, and End Results (SEER) program reveals disturbing trends in early-onset cancer incidence. Between 1992 and 2019, cancer rates among adults aged 20-49 increased across multiple cancer types, with some showing particularly steep increases.
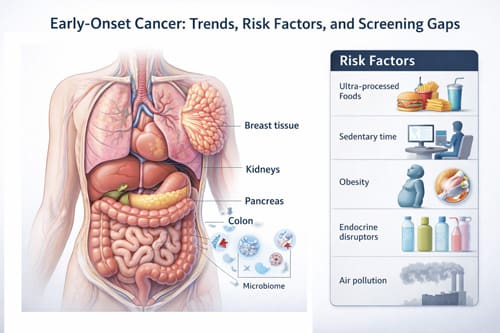
Colorectal cancer exemplifies this trend most dramatically. Incidence rates among adults under 50 have increased by approximately 2% annually since the mid-1990s. This increase contrasts sharply with declining rates among older adults, largely attributed to increased screening in the over-50 population. The American Cancer Society responded to these trends by lowering the recommended screening age from 50 to 45 years in 2018.
Breast cancer among younger women presents a more nuanced picture. While overall breast cancer incidence has stabilized in recent years, specific subtypes show concerning patterns. Triple-negative breast cancer, known for its aggressive nature and poor prognosis, appears to be increasing among women under 40. Additionally, inflammatory breast cancer, though rare, shows higher relative increases in younger age groups.
Cancer Type-Specific Trends
Kidney cancer incidence among young adults has increased substantially, with rates rising by approximately 6.2% annually among individuals aged 20-39. This increase spans both sexes but shows particularly pronounced growth among young women. The reasons for this increase remain unclear, though some researchers point to rising obesity rates and hypertension as potential contributors.
Pancreatic cancer, historically rare in young adults, has shown steady increases across younger age groups. Though absolute numbers remain relatively low, the percentage increase is notable because pancreatic cancer carries one of the poorest prognoses among all cancer types. Early detection remains extremely challenging, making prevention efforts particularly crucial.
Thyroid cancer presents unique epidemiological considerations. While incidence rates have increased dramatically across all age groups, including young adults, much of this increase is attributed to improved detection methods and diagnostic practices rather than true incidence increases. However, researchers debate whether enhanced detection fully explains the observed trends.
Demographic Variations
Cancer incidence trends vary notably across demographic groups. Young Hispanic and Native American populations show particularly concerning increases in certain cancer types. Liver cancer rates among young Hispanic adults have increased substantially, likely related to hepatitis B and C infections, alcohol consumption patterns, and metabolic factors.
African American young adults face elevated risks for several cancer types, including early-onset colorectal cancer. These disparities reflect complex interactions between genetic predisposition, environmental exposures, socioeconomic factors, and healthcare access patterns. Understanding these variations is crucial for developing targeted prevention and screening strategies.
Geographic patterns also emerge in the data. Rural areas often show higher rates of certain early-onset cancers, potentially related to environmental exposures, lifestyle factors, and healthcare access limitations. Conversely, urban areas may show increased rates of other cancer types, possibly related to air pollution, lifestyle factors, and occupational exposures.
Risk Factors and Determinants 
Genetic Predisposition
Genetic factors play crucial roles in early-onset cancer development. Individuals with inherited cancer syndromes such as Lynch syndrome, familial adenomatous polyposis, and BRCA mutations face substantially elevated risks for developing cancer at young ages. However, these known genetic syndromes account for only a small percentage of early-onset cancer cases.
Recent research suggests that polygenic risk scores may better predict cancer risk in younger populations. These scores combine information from multiple genetic variants to estimate individual risk levels. While not yet ready for routine clinical use, polygenic risk assessment may eventually help identify young adults who would benefit from enhanced screening or prevention interventions.
Family history remains one of the strongest predictors of early-onset cancer risk. Individuals with first-degree relatives diagnosed with cancer before age 50 face elevated risks themselves. This observation has led to recommendations for enhanced screening in high-risk families, though implementation varies widely across healthcare systems.
Genetic counseling and testing have become increasingly important components of early-onset cancer care. Many young cancer patients undergo genetic testing to identify hereditary cancer syndromes, both for their own treatment planning and for family risk assessment. The results often influence surgical decisions, treatment choices, and family planning considerations.
Lifestyle and Behavioral Factors
Diet quality has deteriorated substantially among young adults over recent decades. Processed food consumption has increased while fresh fruit and vegetable intake has declined. Ultra-processed foods now comprise approximately 60% of caloric intake among American young adults, representing a dramatic shift from previous generations.
The Western dietary pattern, characterized by high red meat consumption, processed foods, refined sugars, and low fiber intake, has been consistently associated with increased cancer risk. This dietary pattern has become increasingly prevalent among young adults, potentially contributing to rising cancer rates.
Physical activity levels have declined dramatically among young adults. Sedentary occupations have become more common while recreational physical activity has decreased. The rise of screen-based entertainment and remote work has further reduced daily physical activity levels. These changes occur during crucial developmental periods when lifestyle habits become established.
Obesity rates among young adults have increased substantially, with current data showing approximately 40% of adults aged 20-39 classified as obese. Obesity is a well-established risk factor for multiple cancer types, including colorectal, breast, kidney, and pancreatic cancers. The timing of weight gain may be particularly important, with weight gain during young adulthood potentially carrying higher cancer risks than weight gain later in life.
Reproductive and Hormonal Factors
Reproductive patterns have changed dramatically over recent decades. Average age at first childbirth has increased, while total fertility rates have declined. These changes affect hormone exposure patterns throughout women’s lives, potentially influencing breast and ovarian cancer risks.
Breastfeeding duration has declined among American women, despite strong evidence that breastfeeding provides protection against breast and ovarian cancers. Multiple factors contribute to reduced breastfeeding rates, including workplace policies, cultural factors, and healthcare support systems.
Hormonal contraceptive use has evolved with new formulations and delivery methods. While combined hormonal contraceptives provide protection against ovarian and endometrial cancers, they may slightly increase breast and cervical cancer risks. The long-term effects of newer contraceptive methods on cancer risk remain under investigation.
Hormone replacement therapy patterns have shifted following major clinical trials demonstrating cancer risks. However, the full implications of these changes for early-onset cancer risk require continued monitoring, particularly as younger women increasingly seek hormone therapy for various indications.
Environmental Exposures and Their Impact
Chemical Exposures
Environmental chemical exposures during critical developmental periods may contribute to later cancer development. Young adults today experienced unprecedented chemical exposures during childhood and adolescence, including pesticides, plasticizers, flame retardants, and other industrial chemicals.
Endocrine-disrupting chemicals deserve particular attention. These substances can interfere with hormone systems during crucial developmental windows, potentially programming cells for later malignant transformation. Common exposures include bisphenol A from food packaging, phthalates from personal care products, and per- and polyfluoroalkyl substances (PFAS) from various consumer products.
Air pollution exposure has been linked to multiple cancer types, including lung, bladder, and breast cancers. Young adults living in urban areas face higher exposure levels to particulate matter, nitrogen oxides, and other air pollutants. The health effects of these exposures may manifest years or decades later as increased cancer risk.
Occupational exposures among young workers may contribute to later cancer development. Many young adults work in service industries with potential chemical exposures, including restaurants, salons, dry cleaners, and retail environments. These occupational exposures often receive less attention than traditional industrial exposures but may cumulatively contribute to cancer risk.
Water and Food Contamination
Drinking water contamination affects millions of Americans and may contribute to cancer risk. Contaminants of concern include arsenic, nitrates, trihalomethanes, and PFAS. Young adults may be particularly vulnerable to these exposures due to higher water consumption rates and longer expected lifespans over which effects may manifest.
Food contamination presents complex challenges. Pesticide residues on fruits and vegetables, antibiotics and hormones in animal products, and packaging chemicals that migrate into food all represent potential cancer risk factors. The cumulative effects of these low-level exposures over decades remain poorly understood but may contribute to observed cancer trends.
Processed meat consumption has increased among young adults despite strong evidence linking these products to colorectal cancer risk. Processing methods introduce various chemicals, including nitrates, nitrites, and polycyclic aromatic hydrocarbons, which may contribute to carcinogenesis.
Food preparation methods have changed substantially, with increased reliance on processed foods and reduced home cooking. These changes affect not only nutritional quality but also exposure to food additives, preservatives, and packaging chemicals that may influence cancer risk.
Screening Gaps and Diagnostic Challenges 
Age-Based Screening Limitations
Current cancer screening guidelines primarily focus on older adults, creating potential gaps in early detection for younger populations. While these age-based recommendations reflect cancer incidence patterns and cost-effectiveness analyses, rising early-onset cancer rates challenge traditional approaches.
Colorectal cancer screening exemplifies these challenges. The recent reduction in recommended screening age from 50 to 45 represents progress, but some experts argue for even earlier screening in high-risk populations. However, extending screening to younger ages raises questions about test performance, cost-effectiveness, and potential harm from false-positive results.
Breast cancer screening in younger women faces unique challenges. Mammography sensitivity decreases in younger women due to denser breast tissue, while false-positive rates increase. These factors complicate screening decisions for women in their 30s and early 40s, particularly those with family histories or other risk factors.
Cervical cancer screening has evolved with improved understanding of human papillomavirus (HPV) biology. Current guidelines recommend less frequent screening than previous recommendations, but implementation varies. Some young women may not receive appropriate screening due to healthcare access barriers or lack of awareness about recommendations.
Healthcare Access and Utilization
Young adults face unique healthcare access challenges that may delay cancer diagnosis. Many lack health insurance coverage, particularly during transitions between educational institutions, employment changes, or family coverage modifications. These coverage gaps can result in delayed or foregone healthcare, potentially missing opportunities for early cancer detection.
Healthcare utilization patterns among young adults differ from older populations. Young adults are less likely to have established relationships with primary care providers and may be more likely to seek care in urgent care or emergency department settings. These care patterns may not be optimal for cancer screening or early symptom recognition.
Symptom recognition and healthcare-seeking behavior among young adults may contribute to diagnostic delays. Young adults may attribute symptoms to stress, lifestyle factors, or minor illnesses, potentially delaying medical evaluation. Healthcare providers may also attribute symptoms to more common conditions, leading to diagnostic delays.
Cost considerations affect healthcare utilization among young adults, who often face high deductible health plans or limited financial resources. Cancer screening tests, diagnostic workups, and specialty consultations may create financial barriers that delay appropriate care.
Table 1: Early-Onset Cancer Screening Considerations by Age Group
|
Age Group |
Cancer Types for Consideration |
Screening Modalities |
Risk Factors to Assess |
|---|---|---|---|
|
20-29 years |
Cervical, Testicular, Thyroid |
HPV testing, Physical exam, Neck palpation |
Sexual history, Family history, Radiation exposure |
|
30-39 years |
Cervical, Breast, Colorectal |
HPV testing, Clinical breast exam, Consider colonoscopy if high risk |
Family history, Reproductive history, IBD, Lynch syndrome |
|
40-49 years |
Breast, Colorectal, Lung |
Mammography (individualized), Colonoscopy at 45, LDCT if smoking history |
BRCA mutations, Smoking history, Family history |
Gut Microbiome and Cancer Development
Microbiome Disruption Patterns
The gut microbiome plays crucial roles in immune function, metabolism, and cancer development. Young adults today have experienced unprecedented microbiome disruption through antibiotic exposure, dietary changes, and lifestyle factors. These disruptions may contribute to increased cancer susceptibility.
Antibiotic use during childhood and young adulthood has increased substantially over recent decades. While antibiotics provide essential medical benefits, they also profoundly alter gut microbiome composition. Some studies suggest associations between early antibiotic exposure and later cancer development, though causation remains to be established.
Diet quality directly influences microbiome composition and function. The Western dietary pattern promotes inflammatory bacterial species while reducing beneficial bacteria that produce short-chain fatty acids and other protective compounds. These microbiome changes may create conditions favorable for cancer development, particularly in the colorectum.
Modern lifestyle factors contribute to microbiome disruption. Reduced exposure to diverse environmental microorganisms, increased sanitization practices, and decreased physical activity all influence microbiome development and maintenance. The long-term consequences of these changes for cancer risk require further investigation.
Microbiome-Cancer Interactions
Specific bacterial species have been implicated in cancer development. Fusobacterium nucleatum, typically associated with oral health, has been found in colorectal tumors and may promote tumor development and progression. The mechanisms by which oral bacteria translocate to distant sites and influence cancer development remain under active investigation.
Helicobacter pylori infection, while declining in prevalence, remains an important cause of gastric cancer. Young adults today are less likely to be infected with H. pylori compared to previous generations, which may partially explain declining gastric cancer rates. However, other microorganisms may fill ecological niches and potentially influence cancer risk through different mechanisms.
The microbiome influences immune system development and function throughout life. Disrupted microbiomes may result in altered immune responses that affect cancer surveillance and tumor development. These effects may be particularly important during critical developmental periods when immune system programming occurs.
Microbiome-derived metabolites affect host physiology in ways that may influence cancer risk. Short-chain fatty acids produced by beneficial bacteria have anti-inflammatory and anti-cancer properties. Reduced production of these protective compounds may contribute to increased cancer susceptibility among individuals with disrupted microbiomes.
Clinical Implications for Healthcare Providers
Risk Assessment Strategies
Healthcare providers must adapt risk assessment approaches to address rising early-onset cancer rates. Traditional risk calculators may underestimate risk in younger populations, necessitating more nuanced approaches that consider family history, lifestyle factors, and emerging risk markers.
Family history assessment requires particular attention in young adult patients. Detailed three-generation pedigrees help identify hereditary cancer syndromes and guide screening and prevention recommendations. Many healthcare providers lack training in genetic risk assessment, highlighting the need for improved education and referral pathways.
Lifestyle risk factor assessment should encompass diet quality, physical activity, weight history, reproductive factors, and environmental exposures. Standardized tools for assessing these factors can help providers identify high-risk patients who may benefit from enhanced screening or prevention interventions.
Genetic counseling referrals should be considered for young adults with personal or family histories suggesting hereditary cancer syndromes. Genetic counselors can provide detailed risk assessment, coordinate appropriate testing, and help patients understand implications for themselves and family members.
Prevention and Risk Reduction
Primary prevention strategies must address modifiable risk factors affecting young adults. Diet counseling should emphasize whole foods, adequate fiber intake, limited processed meat consumption, and reduced ultra-processed food intake. Practical approaches that acknowledge time constraints and economic considerations are most likely to be successful.
Physical activity promotion requires individualized approaches that consider personal preferences, time constraints, and physical capabilities. Even modest increases in physical activity can provide health benefits, and healthcare providers should help patients identify feasible ways to incorporate movement into daily routines.
Weight management support should focus on sustainable lifestyle changes rather than restrictive dieting approaches. Young adults experiencing weight gain may benefit from early intervention to prevent obesity-related cancer risks from accumulating over time.
Smoking cessation and substance use counseling remain important components of cancer prevention. Young adults may use tobacco products including e-cigarettes, hookah, and smokeless tobacco, all of which carry cancer risks. Counseling should address all forms of tobacco use and provide evidence-based cessation resources.
Early Detection Approaches
Enhanced screening protocols may be appropriate for young adults with elevated cancer risks. Risk-stratified screening approaches consider individual risk factors rather than relying solely on age-based recommendations. These approaches require careful consideration of benefits, risks, and cost-effectiveness.
Symptom awareness education helps young adults recognize concerning symptoms that warrant medical evaluation. Educational efforts should address common early cancer symptoms while avoiding unnecessary anxiety. Healthcare providers should encourage patients to seek evaluation for persistent or concerning symptoms.
Diagnostic workup approaches may need modification for younger patients. Healthcare providers should maintain appropriate suspicion for cancer in young adults with concerning symptoms, even when cancer is statistically uncommon. Delayed diagnosis can have particularly devastating consequences for young patients with many expected life-years remaining.
Follow-up care coordination becomes crucial when cancer is suspected or diagnosed in young adults. Timely specialty referrals, efficient diagnostic workups, and coordinated care teams help minimize delays that could affect treatment outcomes.
Public Health Policy Implications 
Screening Guideline Evolution
Cancer screening guidelines must evolve to address changing epidemiological patterns. Professional organizations should regularly review age-based recommendations and consider risk-stratified approaches that may identify high-risk young adults who would benefit from earlier screening.
Cost-effectiveness analyses need updating to reflect changing cancer incidence patterns and improved screening technologies. Traditional models may not accurately reflect the costs and benefits of screening younger populations, potentially leading to suboptimal policy decisions.
Healthcare payment policies should support appropriate screening for high-risk young adults. Insurance coverage decisions significantly influence screening utilization, and policies must balance cost considerations with public health benefits.
Quality metrics for healthcare systems should include measures of appropriate cancer screening in younger populations. Current quality measures focus primarily on older adults and may not capture important gaps in care for younger patients.
Environmental Regulation
Regulatory policies addressing environmental cancer risk factors require strengthening. Many chemicals in commerce lack adequate safety testing, particularly regarding cancer risks. Regulatory frameworks should prioritize assessment and control of chemicals with potential carcinogenic effects.
Food safety regulations should address emerging concerns about food additives, pesticide residues, and packaging chemicals. Current regulations may not adequately protect against long-term cancer risks from cumulative low-level exposures during critical developmental periods.
Air quality standards need continued improvement to address cancer risks from air pollution exposure. Young adults living in urban areas face higher exposure levels that may contribute to later cancer development. Stronger emissions controls and air quality standards could provide long-term public health benefits.
Water quality protection requires attention to emerging contaminants that may contribute to cancer risk. PFAS, pharmaceutical residues, and other contaminants of emerging concern need better monitoring and control to protect public health.
Healthcare System Adaptations
Healthcare systems must adapt to address the needs of young cancer patients. These patients face unique challenges including fertility preservation, career concerns, financial toxicity, and different treatment tolerances compared to older patients.
Workforce training should address early-onset cancer recognition, risk assessment, and management. Healthcare providers need updated knowledge about changing cancer epidemiology and evidence-based approaches for younger patients.
Patient navigation services should address the specific needs of young cancer patients. Navigation programs can help patients understand complex healthcare systems, coordinate care, and access support resources tailored to their unique circumstances.
Research priorities should emphasize early-onset cancer causes, prevention, and treatment optimization. Current research portfolios may not adequately address the specific needs of younger cancer patients, creating gaps in evidence-based care approaches.
Lifestyle Modification Strategies
Dietary Interventions
Evidence-based dietary recommendations for cancer prevention emphasize plant-rich eating patterns with adequate fiber, limited processed meat, and reduced ultra-processed food consumption. The Mediterranean dietary pattern has strong evidence for cancer prevention and provides a practical framework for dietary counseling.
Meal planning and food preparation skills have declined among young adults, contributing to increased reliance on processed foods. Educational programs that teach practical cooking skills and meal planning can help young adults adopt healthier eating patterns that may reduce cancer risk.
Workplace nutrition programs can address the reality that many young adults consume meals away from home. Employer-sponsored programs that provide healthy food options, nutrition education, or meal planning resources may help workers adopt healthier eating patterns.
Community-based interventions should address food access issues that affect dietary quality. Food deserts, high costs of healthy foods, and limited access to grocery stores create barriers to healthy eating that require policy-level interventions to address effectively.
Physical Activity Promotion
Physical activity recommendations for cancer prevention suggest at least 150 minutes of moderate-intensity activity per week, along with muscle-strengthening activities. However, these recommendations may seem overwhelming to sedentary individuals, suggesting the need for graduated approaches that start with modest goals.
Workplace physical activity programs can address the reality that many young adults spend most waking hours in sedentary occupations. Programs that encourage walking meetings, provide on-site fitness facilities, or offer activity breaks during the workday may help workers incorporate more movement into daily routines.
Community infrastructure affects physical activity levels through availability of safe walking and cycling routes, recreational facilities, and public transportation options. Policy interventions that create activity-friendly environments may have population-level effects on physical activity and cancer risk.
Technology-based interventions using fitness trackers, smartphone apps, or online platforms may appeal to young adults and provide convenient ways to monitor and increase physical activity levels. However, the long-term effectiveness of these approaches requires further evaluation.

Future Research Directions
Biomarker Development
Early detection biomarkers could revolutionize cancer screening in younger populations. Current research focuses on circulating tumor DNA, protein markers, and metabolomic signatures that might detect cancer before symptoms develop. These approaches could enable precision screening based on individual risk profiles.
Risk prediction models need improvement to better identify young adults at elevated cancer risk. Models that incorporate genetic, lifestyle, environmental, and biomarker data may provide more accurate risk estimates than current approaches based primarily on age and family history.
Pharmacogenomic research may identify individuals who respond differently to environmental exposures based on genetic variations in metabolism, DNA repair, or detoxification pathways. This information could guide personalized prevention recommendations and environmental exposure limits.
Longitudinal studies tracking individuals from childhood through adulthood are needed to understand how early exposures and experiences influence later cancer risk. These studies require substantial time and resource investments but could provide crucial insights into cancer prevention strategies.
Intervention Studies
Lifestyle intervention trials should test whether changes in diet, physical activity, and other modifiable factors can reduce cancer risk in younger populations. Most existing evidence comes from observational studies, and randomized controlled trials would strengthen the evidence base for prevention recommendations.
Screening trial designs need adaptation to address early-onset cancer detection. Traditional screening trials require large sample sizes and long follow-up periods, making them challenging to conduct in younger populations with lower baseline cancer rates.
Environmental intervention studies could test whether reducing specific exposures affects cancer risk. These studies might focus on dietary interventions that reduce exposure to contaminants, air filtration systems that reduce air pollution exposure, or water treatment approaches that eliminate specific contaminants.
Microbiome intervention studies should explore whether modifying gut microbiome composition affects cancer risk. Interventions might include dietary changes, prebiotic or probiotic supplements, or other approaches to promote beneficial bacterial communities.
Limitations and Challenges
Data Quality Considerations
Cancer registry data, while essential for monitoring trends, have limitations that may affect interpretation of early-onset cancer patterns. Changes in diagnostic practices, screening behaviors, and healthcare access can influence apparent incidence trends independent of true changes in cancer occurrence.
Exposure assessment challenges limit understanding of environmental and lifestyle contributions to early-onset cancer. Measuring lifetime exposures to multiple chemicals, dietary components, and other factors presents methodological difficulties that may obscure important risk relationships.
Confounding factors complicate interpretation of observational studies examining early-onset cancer risk factors. Lifestyle factors, environmental exposures, and genetic predisposition interact in complex ways that make it difficult to identify independent causal relationships.
Selection bias may affect studies of early-onset cancer patients, who may differ systematically from typical cancer patients in ways that influence study results. Healthcare-seeking behavior, socioeconomic factors, and other characteristics may create biased study populations.
Healthcare System Barriers
Healthcare provider knowledge gaps regarding early-onset cancer recognition and management may contribute to diagnostic delays and suboptimal care. Medical education curricula may not adequately address changing cancer epidemiology or evidence-based approaches for younger patients.
Insurance coverage limitations may create barriers to appropriate screening, genetic testing, and specialized care for young adults at high cancer risk. Prior authorization requirements, high deductibles, and limited provider networks can delay or prevent appropriate care.
Healthcare system fragmentation may impede coordinated care for young cancer patients who require multidisciplinary management. Communication gaps between providers, care transitions, and lack of care coordination can adversely affect patient outcomes.
Cost considerations affect both patients and healthcare systems in addressing early-onset cancer. Screening, diagnostic workups, and treatment for younger patients may not be cost-effective under traditional health economic models, creating tensions between individual and population-level decision-making.
Research Infrastructure Needs
Funding priorities may not adequately address early-onset cancer research needs. Traditional research funding mechanisms may favor studies of more common cancers affecting older adults, potentially limiting investment in early-onset cancer research.
Research infrastructure limitations may impede large-scale studies needed to understand early-onset cancer causes and develop prevention strategies. Cohort studies, biobanking initiatives, and data sharing platforms require substantial resources and coordination.
Regulatory frameworks for cancer prevention research may not accommodate novel study designs or interventions. Traditional clinical trial regulations may be overly restrictive for prevention studies, while environmental health research may face regulatory barriers.
Interdisciplinary collaboration requirements for early-onset cancer research may challenge traditional academic structures. Understanding complex interactions between genetics, environment, lifestyle, and cancer development requires expertise from multiple disciplines working together effectively.

Conclusion 

Key Takeaways
The rapid increase in early-onset cancer incidence represents a critical public health challenge requiring immediate attention from healthcare providers, policymakers, and researchers. Current trends suggest that traditional approaches to cancer prevention and screening may be inadequate for addressing the needs of younger populations at risk.
Healthcare providers must adapt clinical practices to address rising early-onset cancer rates through improved risk assessment, enhanced screening approaches for high-risk individuals, and evidence-based prevention counseling. Family history assessment, lifestyle factor evaluation, and appropriate genetic counseling referrals are essential components of comprehensive care.
Public health policy must evolve to address environmental and lifestyle factors contributing to early-onset cancer. Stronger environmental regulations, improved food safety standards, and healthcare system adaptations are needed to protect younger populations from cancer risks and ensure appropriate care when cancer occurs.
Research priorities should emphasize understanding the causes of early-onset cancer, developing better prevention and detection strategies, and optimizing treatment approaches for younger patients. Long-term studies tracking individuals from childhood through adulthood could provide crucial insights into cancer development and prevention.
Individual-level interventions focusing on modifiable lifestyle factors remain important for cancer prevention. Diet quality improvement, physical activity promotion, weight management, and tobacco cessation provide evidence-based approaches for reducing cancer risk among young adults.
The complexity of factors contributing to early-onset cancer suggests that no single intervention will solve this problem. Instead, coordinated efforts addressing environmental exposures, lifestyle factors, healthcare system gaps, and research needs are required to reverse current trends and protect future generations from preventable cancers.
Frequently Asked Questions: 
What age groups are considered “early-onset” for cancer diagnosis?
Early-onset cancer typically refers to cancers diagnosed before age 50, though some researchers use age 40 as a cutoff depending on the specific cancer type. The definition varies among different medical organizations and research studies, but most focus on cancers occurring in adults under 50 years of age.
Which types of cancer show the largest increases in younger adults?
Colorectal cancer shows the most dramatic increases, with rates rising approximately 2% annually among adults under 50 since the mid-1990s. Other cancers showing notable increases include kidney, pancreatic, and certain breast cancer subtypes. The patterns vary by specific cancer type and demographic groups.
Should screening guidelines be changed for younger adults?
Some screening guidelines have already been updated, such as the American Cancer Society’s recommendation to begin colorectal cancer screening at age 45 instead of 50. However, decisions about screening in younger adults should be individualized based on family history, risk factors, and clinical judgment rather than applying universal age-based recommendations.
What lifestyle factors most strongly influence early-onset cancer risk?
Diet quality, physical activity levels, obesity, and tobacco use represent the most important modifiable lifestyle factors. The Western dietary pattern high in processed foods and low in fiber, combined with sedentary lifestyles and rising obesity rates, appears to contribute substantially to increased cancer risk among younger adults.
How do environmental exposures contribute to early-onset cancer?
Environmental factors including air pollution, chemical exposures from food packaging and personal care products, water contamination, and occupational exposures may contribute to cancer risk. The effects of these exposures may not become apparent until years or decades later, making it difficult to establish direct causal relationships.
What role does genetics play in early-onset cancer?
While inherited cancer syndromes like Lynch syndrome and BRCA mutations account for some early-onset cancers, they represent only a small percentage of cases. Family history remains an important risk factor, and genetic counseling may be appropriate for individuals with strong family histories of cancer at young ages.
How has the gut microbiome contributed to changing cancer rates?
Antibiotic use, dietary changes, and lifestyle factors have altered gut microbiome composition in ways that may increase cancer risk, particularly for colorectal cancer. Disrupted microbiomes may reduce production of protective compounds and alter immune function in ways that favor cancer development.
What should young adults do to reduce their cancer risk?
Young adults should focus on maintaining healthy diets rich in fruits, vegetables, and whole grains while limiting processed foods and red meat. Regular physical activity, maintaining healthy weight, avoiding tobacco, limiting alcohol consumption, and staying current with recommended screenings are important prevention strategies.
How can healthcare providers better address early-onset cancer?
Providers should conduct thorough family history assessments, evaluate lifestyle and environmental risk factors, maintain appropriate clinical suspicion for cancer symptoms in young patients, and consider genetic counseling referrals when indicated. Staying current with evolving screening guidelines and evidence-based prevention strategies is essential.
What research is needed to better understand early-onset cancer?
Priority research areas include identifying biomarkers for early detection, conducting longitudinal studies to understand how childhood and young adult exposures affect later cancer risk, testing lifestyle interventions for cancer prevention, and developing better risk prediction models that incorporate genetic, environmental, and lifestyle factors.
References: 
American Cancer Society. (2023). Cancer facts and figures 2023. American Cancer Society.
Anderson, W. F., Rosenberg, P. S., Prat, A., Perou, C. M., & Sherman, M. E. (2014). How many etiological subtypes of breast cancer: Two, three, four, or more? Journal of the National Cancer Institute, 106(8), dju165.
Araghi, M., Soerjomataram, I., Bardot, A., Ferlay, J., Cabasag, C. J., Morrison, D. S., … & Arnold, M. (2019). Changes in colorectal cancer incidence in seven high-income countries: A population-based study. The Lancet Gastroenterology & Hepatology, 4(7), 511-518.
Bailey, C. E., Hu, C. Y., You, Y. N., Bednarski, B. K., Rodriguez-Bigas, M. A., Skibber, J. M., … & Chang, G. J. (2015). Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975-2010. JAMA Surgery, 150(1), 17-22.
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 68(6), 394-424.
Chen, H., Zheng, X., Zheng, Y. (2014). Age at diagnosis of cancer in China during 2003-2012: A population-based study. Cancer Medicine, 3(4), 1098-1102.
Cheng, E., Sobolev, B., Jerzak, K. J., Rosenberg, S., & Weberpals, J. I. (2022). The association between socioeconomic status and cancer incidence, stage at diagnosis, treatment and survival: A systematic review and meta-analysis. Cancer Causes & Control, 33(1), 1-18.
Collaborators, G. B. D. (2019). Health effects of dietary risks in 195 countries, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. The Lancet, 393(10184), 1958-1972.
Connell, L. C., Mota, J. M., Braghiroli, M. I., & Hoff, P. M. (2017). The rising incidence of younger patients with colorectal cancer: Questions about screening, biology, and treatment. Current Treatment Options in Oncology, 18(4), 23.
Force, U. S. P. S. T. (2021). Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA, 325(19), 1965-1977.
Giaquinto, A. N., Sung, H., Miller, K. D., Kramer, J. L., Newman, L. A., Minihan, A., … & Siegel, R. L. (2022). Breast cancer statistics, 2022. CA: A Cancer Journal for Clinicians, 72(6), 524-541.
Kehm, R. D., Yang, W., Tehranifar, P., & Terry, M. B. (2019). 40 years of change in age- and stage-specific cancer incidence rates in US women and men. JNCI Cancer Spectrum, 3(3), pkz038.
Liu, P. H., Wu, K., Ng, K., Zauber, A. G., Nguyen, L. H., Song, M., … & Giovannucci, E. L. (2019). Association of obesity with risk of early-onset colorectal cancer among women. JAMA Oncology, 5(1), 37-44.
Mauri, G., Sartore-Bianchi, A., Russo, A. G., Marsoni, S., Bardelli, A., & Siena, S. (2019). Early-onset colorectal cancer in young individuals. Molecular Oncology, 13(2), 109-131.
Murphy, C. C., Harlan, L. C., Lund, J. L., Lynch, C. F., & Geiger, A. M. (2015). Patterns of colorectal cancer care in the United States: 1990-2010. Journal of the National Cancer Institute, 107(10), djv198.
Patel, P., De, P. (2016). Trends in colorectal cancer incidence and related lifestyle risk factors in 15-49-year-olds in Canada, 1969-2010. Cancer Epidemiology, 42, 90-100.
Patel, S. G., Karlitz, J. J., Yen, T., Lieu, C. H., & Boland, C. R. (2022). The rising tide of early-onset colorectal cancer: A comprehensive review of epidemiology, clinical features, biology, risk factors, prevention, and early detection. The Lancet Gastroenterology & Hepatology, 7(3), 262-274.
Rosato, V., Bosetti, C., Levi, F., Polesel, J., Zucchetto, A., Negri, E., & La Vecchia, C. (2013). Risk factors for young-onset colorectal cancer. Cancer Causes & Control, 24(2), 335-341.
Saraiva, M. R., Rosa, I., Borralho, P., Cravo, M., & de Sousa Guerreiro, C. (2023). Inflammatory bowel disease and colorectal cancer risk: An overview from pathophysiology to pharmacological prevention. Digestive Diseases and Sciences, 68(5), 1842-1857.
Scott, R. B., Rangel, L. E., Osler, T. M., & Hyman, N. H. (2016). Rectal cancer in patients under the age of 50 years: The delayed diagnosis. American Journal of Surgery, 211(6), 1014-1018.
Siegel, R. L., Fedewa, S. A., Anderson, W. F., Miller, K. D., Ma, J., Rosenberg, P. S., & Jemal, A. (2017). Colorectal cancer incidence patterns in the United States, 1974-2013. Journal of the National Cancer Institute, 109(8), djw322.
Siegel, R. L., Miller, K. D., Fuchs, H. E., & Jemal, A. (2022). Cancer statistics, 2022. CA: A Cancer Journal for Clinicians, 72(1), 7-33.
Siegel, R. L., Torre, L. A., Soerjomataram, I., Hayes, R. B., Bray, F., Weber, T. K., & Jemal, A. (2019). Global patterns and trends in colorectal cancer incidence in young adults. Gut, 68(12), 2179-2185.
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., & Bray, F. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 71(3), 209-249.
Wolf, A. M., Fontham, E. T., Church, T. R., Flowers, C. R., Guerra, C. E., LaMonte, S. J., … & Andrews, K. S. (2018). Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA: A Cancer Journal for Clinicians, 68(4), 250-281.
Zaborowski, A. M., Abdile, A., Adamina, M., Aigner, F., d’Allens, L., Allmer, C., … & Winter, D. C. (2023). Characteristics of early-onset vs late-onset colorectal cancer: A review. JAMA Surgery, 158(7), 767-774.
Implications for health care professionals: ![]()
Recent Articles 
Integrative Perspectives on Cognition, Emotion, and Digital Behavior

Sleep-related:
Longevity/Nutrition & Diet:
Philosophical / Happiness:
Other:
Modern Mind Unveiled
Developed under the direction of David McAuley, Pharm.D., this collection explores what it means to think, feel, and connect in the modern world. Drawing upon decades of clinical experience and digital innovation, Dr. McAuley and the GlobalRPh initiative translate complex scientific ideas into clear, usable insights for clinicians, educators, and students.
The series investigates essential themes—cognitive bias, emotional regulation, digital attention, and meaning-making—revealing how the modern mind adapts to information overload, uncertainty, and constant stimulation.
At its core, the project reflects GlobalRPh’s commitment to advancing evidence-based medical education and clinical decision support. Yet it also moves beyond pharmacotherapy, examining the psychological and behavioral dimensions that shape how healthcare professionals think, learn, and lead.
Through a synthesis of empirical research and philosophical reflection, Modern Mind Unveiled deepens our understanding of both the strengths and vulnerabilities of the human mind. It invites readers to see medicine not merely as a science of intervention, but as a discipline of perception, empathy, and awareness—an approach essential for thoughtful practice in the 21st century.
The Six Core Themes
I. Human Behavior and Cognitive Patterns
Examining the often-unconscious mechanisms that guide human choice—how we navigate uncertainty, balance logic with intuition, and adapt through seemingly irrational behavior.
II. Emotion, Relationships, and Social Dynamics
Investigating the structure of empathy, the psychology of belonging, and the influence of abundance and selectivity on modern social connection.
III. Technology, Media, and the Digital Mind
Analyzing how digital environments reshape cognition, attention, and identity—exploring ideas such as gamification, information overload, and cognitive “nutrition” in online spaces.
IV. Cognitive Bias, Memory, and Decision Architecture
Exploring how memory, prediction, and self-awareness interact in decision-making, and how external systems increasingly serve as extensions of thought.
V. Habits, Health, and Psychological Resilience
Understanding how habits sustain or erode well-being—considering anhedonia, creative rest, and the restoration of mental balance in demanding professional and personal contexts.
VI. Philosophy, Meaning, and the Self
Reflecting on continuity of identity, the pursuit of coherence, and the construction of meaning amid existential and informational noise.
Keywords
Cognitive Science • Behavioral Psychology • Digital Media • Emotional Regulation • Attention • Decision-Making • Empathy • Memory • Bias • Mental Health • Technology and Identity • Human Behavior • Meaning-Making • Social Connection • Modern Mind
Video Section 

