Food Allergy Desensitization: Is Oral Immunotherapy Ready for Prime Time?
Abstract
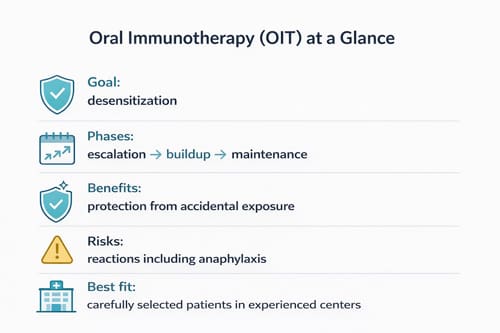
Food allergies affect millions of people worldwide and can cause severe, life-threatening reactions. Traditional management has focused on strict food avoidance and emergency treatment. Oral immunotherapy (OIT) has emerged as a promising treatment that gradually introduces small amounts of allergens to reduce sensitivity. This paper examines the current state of oral immunotherapy for food allergies, analyzing clinical evidence, safety data, and practical considerations for implementation in clinical practice. We reviewed recent clinical trials, meta-analyses, and real-world studies to assess effectiveness and safety outcomes. Results show that OIT can achieve desensitization in many patients, but questions remain about long-term benefits, safety profiles, and patient selection criteria. While OIT shows promise, challenges, including adverse reactions, treatment burden, and variable response rates, suggest careful patient selection and specialized care are essential. The evidence supports OIT as a viable treatment option for select patients when performed in experienced centers, but widespread implementation requires additional research and standardized protocols.
Introduction
Food allergies represent a growing public health concern affecting approximately 8% of children and 5% of adults in developed countries. These immune-mediated reactions can range from mild symptoms to severe anaphylaxis, which can be fatal. The prevalence of food allergies has increased over the past several decades, particularly in peanut, tree nut, and shellfish allergies.
For many years, the standard approach to food allergy management has relied on three main strategies: strict avoidance of trigger foods, patient and family education about allergen identification, and emergency treatment with epinephrine auto-injectors. While this approach has helped prevent many severe reactions, it places a heavy burden on patients and families. The constant vigilance required for food avoidance can limit social activities, create anxiety, and reduce quality of life.
The need for more effective treatments has driven research into immunotherapy approaches. Oral immunotherapy has gained attention as a potential treatment that could reduce the severity of allergic reactions or even eliminate them. This approach involves gradually increasing patients’ exposure to their allergen over time to train the immune system to tolerate the food.
Understanding whether OIT is ready for widespread clinical use requires examining the evidence for effectiveness, safety considerations, practical implementation challenges, and comparing it to other available treatments. This analysis is crucial for clinicians considering whether to offer OIT to their patients and for developing appropriate guidelines for its use.
Background and Pathophysiology
Food allergies involve an abnormal immune response to specific food proteins. In individuals with allergies, the immune system mistakenly identifies harmless food proteins as threats. This leads to the production of immunoglobulin E (IgE) antibodies specific to those proteins. When the person eats the food again, these antibodies trigger the release of inflammatory substances, such as histamine, from mast cells and basophils.
The allergic reaction can involve multiple organ systems. Skin reactions include hives, swelling, and itching. Gastrointestinal symptoms may include nausea, vomiting, diarrhea, and abdominal pain. Respiratory symptoms can range from a runny nose and cough to severe breathing difficulties. The most serious reaction is anaphylaxis, which involves multiple organ systems and can cause dangerous drops in blood pressure, severe breathing problems, and loss of consciousness.
Eight foods account for about 90% of allergic reactions: milk, eggs, peanuts, tree nuts, fish, shellfish, wheat, and soy. Peanut allergy has received particular attention because it tends to be lifelong, can cause severe reactions, and affects a large number of people. Unlike milk and egg allergies, which children often outgrow, peanut allergies typically persist into adulthood.
The concept behind immunotherapy is based on the principle of immune tolerance. Exposing the immune system to small, controlled amounts of an allergen may help retrain the immune response. This process involves complex changes in immune cell populations, including shifts from allergic T-helper cell responses to more tolerant responses, as well as changes in antibody production.
Research has shown that oral immunotherapy can lead to several types of immune changes. These include increases in allergen-specific IgG4 antibodies, which may have protective effects, and changes in T-cell responses that favor tolerance rather than allergic reactions. However, the exact mechanisms remain under study, and individual responses can vary considerably.

Current Evidence for Oral Immunotherapy 
Clinical Trial Results
Numerous clinical trials have examined OIT for various food allergies, with the largest body of evidence focusing on peanut allergy. The landmark PALISADE trial, published in 2018, was a large randomized controlled trial involving 551 participants aged 4 to 55 years with peanut allergy. Participants received either peanut protein powder or a placebo daily for approximately one year.
The results showed that 67% of participants in the treatment group could tolerate at least 600 mg of peanut protein (about 2 peanuts) at the end of treatment, compared with only 4% in the placebo group. This level of tolerance could protect against accidental exposures, which typically involve smaller amounts of allergen.
Similar studies have been conducted for other food allergies. Milk OIT trials have generally shown high rates of desensitization, with many participants able to tolerate full milk servings after treatment. Egg OIT has also shown promising results, with some studies reporting desensitization rates of 75% or higher.
A meta-analysis published in 2020 examined data from 31 randomized controlled trials of food OIT involving over 1,900 participants. The analysis found that OIT was effective for achieving desensitization across different food allergies. The pooled results showed that patients receiving OIT were much more likely to pass food challenges compared to those receiving placebo or standard care.
Long-term Outcomes
While short-term desensitization can be achieved in many patients, questions remain about long-term benefits. Some studies have followed patients for several years after completing OIT protocols. These long-term studies show that some patients maintain their tolerance even after stopping regular allergen consumption, a state called sustained unresponsiveness or tolerance.
However, long-term outcomes are variable. Some patients who achieve desensitization during treatment lose their tolerance if they stop consuming the allergen regularly. Others maintain protection against severe reactions even if they cannot consume normal amounts of the food. This variability makes it difficult to predict individual outcomes and has implications for treatment recommendations.
A follow-up study of the PALISADE trial participants found that continued daily consumption of peanut protein was necessary to maintain desensitization in most patients. When participants stopped taking the treatment, many gradually lost their tolerance over time. This finding suggests that OIT may require long-term maintenance rather than providing a permanent cure.
Real-world Evidence
Clinical trials are conducted under carefully controlled conditions, but real-world implementation can face different challenges. Several studies have examined OIT outcomes in clinical practice settings. These studies generally show lower success rates than controlled trials, reflecting the challenges of implementing OIT outside research settings.
Real-world studies have identified several factors that affect outcomes. Patient adherence to treatment protocols is crucial but can be challenging to maintain over the months or years required for treatment. Access to specialized care and monitoring is essential but may be limited in some areas. Family support and understanding of the treatment process also play important roles in success.
Safety Considerations
Adverse Reactions
Safety is a major concern with OIT because the treatment involves deliberately giving allergens to allergic patients. Adverse reactions are common and can range from mild to severe. Most patients experience adverse reactions during treatment, particularly in the early phases as doses are increased.
Mild reactions include oral itching, abdominal discomfort, and skin symptoms like hives. These reactions are often manageable with antihistamines and typically decrease over time as patients become desensitized. More serious reactions can include vomiting, breathing difficulties, and anaphylaxis requiring epinephrine treatment.
The PALISADE trial provided detailed safety data showing that 21% of participants in the treatment group experienced severe allergic reactions compared to 6% in the placebo group. Most of these reactions occurred during the dose-escalation phase, when patients were gradually increasing their allergen intake. About 11% of patients discontinued treatment due to adverse reactions.
Risk Factors for Severe Reactions
Research has identified several factors that increase the risk of severe reactions during OIT. Patients with a history of severe reactions to their allergen may be at higher risk during treatment. High levels of allergen-specific IgE antibodies and positive skin test results have been associated with increased reaction risk.
Co-factors can also trigger reactions in patients who normally tolerate their maintenance dose. Exercise, illness, alcohol consumption, and certain medications can lower the threshold for allergic reactions. Patients undergoing OIT need education about these risk factors and may need to modify their activities during treatment.
Asthma is another important risk factor. Patients with poorly controlled asthma are at higher risk for severe reactions during OIT. Many protocols require that asthma be well-controlled before starting treatment and include regular monitoring of respiratory function during therapy.
Monitoring and Management
Safe implementation of OIT requires careful monitoring and management protocols. Patients typically start treatment in supervised clinical settings where emergency treatment is available. Initial doses are often given in the clinic with observation periods to monitor for reactions.
Regular follow-up visits are essential to assess tolerance, adjust doses, and monitor for adverse effects. Many protocols include standardized scales for assessing reaction severity and clear guidelines for dose modifications. Patients and families need training in recognizing and managing allergic reactions, including when to use epinephrine.
Emergency action plans are crucial components of OIT programs. These plans should specify which symptoms require epinephrine use, when to seek emergency medical care, and how to contact the treatment team for guidance. Regular review and updates of these plans help ensure an appropriate response to reactions.
Treatment Protocols and Implementation 
Standard OIT Protocols
Most OIT protocols follow a similar general structure with three main phases. The initial escalation phase involves starting with very small doses and gradually increasing them over several weeks or months. This phase typically requires frequent clinic visits and careful monitoring for reactions.
The buildup phase continues with dose increases but usually with less frequent visits. The goal is to reach a target maintenance dose that protects against accidental exposures. This phase can take several months to complete and requires good patient adherence and tolerance of the treatment.
The maintenance phase involves taking the same dose regularly, typically daily, to maintain desensitization. The duration of maintenance therapy varies across protocols, with some recommending indefinite continuation and others including planned discontinuation to assess sustained tolerance.
Dose escalation schedules vary among different protocols. Some use rapid escalation over days or weeks, while others prefer slower increases over many months. Faster protocols may achieve desensitization more quickly but may also have higher rates of adverse reactions. Slower protocols may be better tolerated but require longer treatment periods.
Patient Selection Criteria
Appropriate patient selection is crucial for OIT success and safety. Most protocols include specific inclusion and exclusion criteria based on research evidence and safety considerations. Age requirements vary, but many programs treat children and adolescents, with some also including adults.
Confirmation of food allergy through appropriate testing is essential. This typically includes a combination of clinical history, skin tests, blood tests for specific IgE antibodies, and sometimes food challenges. The severity and pattern of previous reactions help guide treatment decisions.
Medical conditions that might increase treatment risks need careful evaluation. Poorly controlled asthma is often an exclusion criterion, while well-controlled asthma may be acceptable with extra monitoring. Other conditions affecting immune function or the ability to communicate symptoms may also affect eligibility.
Psychosocial factors are also important considerations. Families need to understand the treatment commitment required and demonstrate the ability to follow complex protocols. Access to emergency care and the ability to attend regular follow-up visits are practical requirements for safe treatment.
Clinical Infrastructure Requirements
Implementing OIT requires specialized clinical infrastructure and expertise. Treatment centers need staff trained in allergy management and emergency treatment of severe reactions. Equipment for managing anaphylaxis, including medications and monitoring capabilities, must be readily available.
Standardized protocols help ensure consistent and safe treatment delivery. These protocols should cover dose preparation, administration procedures, reaction assessment and management, and criteria for dose adjustments. Regular staff training and protocol updates help maintain quality and safety standards.
Quality assurance measures are important for maintaining treatment standards. This may include regular review of patient outcomes, adverse event reporting, and comparison with established benchmarks. Some programs participate in registries or research networks that help track outcomes and identify best practices.
Comparison with Alternative Approaches
Epicutaneous Immunotherapy
Epicutaneous immunotherapy (EPIT) represents an alternative approach to oral immunotherapy. Instead of consuming allergens, EPIT uses skin patches that deliver small amounts of allergen through the skin barrier. This approach may have some safety advantages, as the doses delivered are much lower than those used in OIT.
Clinical trials of peanut EPIT have shown modest effectiveness compared to OIT. The treatment is well tolerated, with fewer severe reactions, but desensitization rates are generally lower than those achieved with OIT. EPIT may be most suitable for patients who cannot tolerate OIT or those seeking a lower-risk treatment option.
The convenience of patch application compared to daily food consumption is another potential advantage of EPIT. However, skin reactions at the patch site are common and can sometimes lead to treatment discontinuation. Long-term studies are still needed to fully evaluate the effectiveness and safety of this approach.
Sublingual Immunotherapy
Sublingual immunotherapy (SLIT) involves placing allergen extracts under the tongue for absorption through the oral mucosa. This approach uses smaller doses than OIT and may have a better safety profile. However, clinical trials have generally shown lower rates of desensitization compared to OIT.
SLIT may be appropriate for patients who cannot tolerate higher doses used in OIT. The treatment is typically well tolerated, with most adverse reactions being mild oral symptoms. However, the lower effectiveness compared to OIT may limit its clinical utility for achieving meaningful protection against accidental exposures.
Some research has examined combination approaches that use SLIT as an initial treatment followed by OIT. This staged approach might allow some patients to eventually achieve higher levels of desensitization while minimizing the risk of initial reactions. However, more research is needed to establish the optimal protocols for combined treatments.
Biological Therapies
Biological therapies target specific components of the allergic response and may be used alone or in combination with immunotherapy. Omalizumab is an anti-IgE antibody that binds to allergic antibodies and prevents them from triggering reactions. Studies have shown that omalizumab can reduce reaction severity during OIT and may allow some patients to tolerate the treatment who would otherwise be unable to.
Other biological agents under investigation target different parts of the allergic response. These include treatments that block specific inflammatory substances or modify immune cell function. While promising, most of these approaches remain experimental and are not yet available for routine clinical use.
The main limitations of biological therapies include high costs, the need for regular injections, and potential side effects. These treatments may be most appropriate for patients with severe allergies who cannot tolerate other approaches, or as adjuncts to improve the safety of immunotherapy.

Current Clinical Applications
FDA-Approved Treatments
The first OIT product approved by the FDA was Palforzia for the treatment of peanut allergy in patients aged 4 to 17 years. This approval in 2020 marked a milestone in food allergy treatment, providing a standardized treatment option backed by rigorous clinical trial data. Palforzia contains precisely measured amounts of peanut protein in capsules that can be opened and mixed with food.
The approval came with specific requirements for administration only in certified healthcare settings by providers trained in the treatment protocol. This requirement reflects the serious nature of potential adverse reactions and the need for appropriate monitoring and emergency management capabilities.
Insurance coverage for FDA-approved OIT treatments varies and can be a barrier to access. The specialized nature of treatment and monitoring requirements also limits availability to centers with appropriate expertise and infrastructure. These factors mean that access remains limited despite regulatory approval.
Off-Label Use
Many allergy specialists offer OIT using food-based protocols that are not FDA-approved but are based on published research protocols. These approaches typically use actual foods, such as peanut flour or dried milk powder, rather than pharmaceutical products. While these treatments can be effective, they lack the standardization and quality control of approved products.
The use of food-based protocols requires careful attention to allergen content variability and to dose standardization. Different batches of food products may contain varying amounts of allergenic proteins, which could affect treatment outcomes and safety. Some centers have developed specialized procedures for food preparation and testing to address these concerns.
Off-label OIT protocols may offer greater flexibility in target foods and treatment approaches. For food allergies without approved treatments, carefully implemented food-based protocols may be the only available immunotherapy option. However, the increased complexity and variability require additional expertise and caution.
Integration into Clinical Practice
Incorporating OIT into clinical practice requires careful consideration of patient population, available resources, and institutional capabilities. Many allergy practices have developed specialized programs with dedicated staff and protocols for OIT delivery. These programs often serve as regional referral centers due to the specialized nature of the treatment.
Collaboration between different specialists may be beneficial for OIT programs. Partnerships with emergency medicine, pediatrics, and other relevant specialties can help ensure appropriate patient care and emergency management. Some programs also work with dietitians and mental health professionals to address the broader impacts of food allergies.
Patient education and support services are crucial components of successful OIT programs. Families need extensive education about treatment protocols, reaction management, and lifestyle modifications. Support groups and educational resources can help patients and families navigate the challenges of treatment and long-term management.
| Treatment Comparison Table |
| Treatment Type |
| Oral Immunotherapy (OIT) |
| Epicutaneous Immunotherapy (EPIT) |
| Sublingual Immunotherapy (SLIT) |
| Avoidance + Emergency Treatment |
Challenges and Limitations 
Treatment Burden and Adherence
OIT requires a substantial commitment from patients and families. Daily dosing schedules, frequent medical visits, and ongoing monitoring create a treatment burden that can be difficult to maintain over the extended periods required for therapy. Studies show that adherence rates decline over time, with some patients discontinuing treatment before completing protocols.
The complexity of treatment protocols can also create challenges. Patients must carefully measure doses, follow timing requirements, and monitor for reactions. Travel, illness, and schedule disruptions can interfere with treatment adherence. Some patients find the daily reminder of their food allergy through required dosing to be psychologically burdensome.
Family dynamics and support systems play crucial roles in treatment success. Parents or caregivers often bear primary responsibility for managing treatment protocols, which can create stress and family conflicts. Adolescent patients may struggle with independence and responsibility for their own treatment management.
Variable Treatment Response
Not all patients respond equally well to OIT. While clinical trials report average success rates, individual responses vary considerably. Some patients achieve full tolerance to normal serving sizes, while others gain only limited protection against small accidental exposures. Predicting individual response remains challenging despite ongoing research into biomarkers and predictive factors.
The definition of treatment success also varies among studies and clinical programs. Some focus on the ability to consume normal food servings, while others emphasize protection against accidental exposures. These different goals may require different treatment approaches and create confusion about expected outcomes.
Factors affecting treatment response include baseline allergy severity, age, adherence to protocols, and individual immune system characteristics. Genetic factors may also play a role, though specific predictive markers have not yet been identified. This variability makes it difficult to counsel patients about their likely outcomes before starting treatment.
Long-term Sustainability
Questions remain about the long-term sustainability of OIT benefits. Many patients require ongoing daily allergen consumption to maintain their desensitization, effectively creating a lifelong treatment commitment. For patients who achieve sustained tolerance, the duration of protection and factors affecting long-term outcomes are still being studied.
The practical implications of long-term maintenance create additional challenges. Patients must continue to purchase and consume allergen-containing products regularly. For some allergens like peanuts, this may be relatively straightforward, but for others like milk or eggs, it may require ongoing dietary modifications.
Some patients experience a decline in tolerance over time, even with maintenance dosing. This may require dose adjustments or additional treatment cycles. The optimal long-term management strategies for these situations are still being developed through ongoing research and clinical experience.
Cost and Access Issues
The cost of OIT can be substantial, including expenses for medical visits, monitoring, emergency medications, and the treatment products themselves. FDA-approved treatments like Palforzia come with high prices that insurance plans may not fully cover. Even food-based protocols involve costs for specialized medical care and monitoring.
Geographic access to qualified treatment centers remains limited. OIT requires specialized expertise that may not be available in all areas, particularly rural or underserved communities. This geographic disparity in access creates inequities in treatment availability and may require patients to travel long distances for care.
Healthcare system capacity is another limitation. The intensive monitoring and specialized care required for OIT limit the number of patients that individual providers can treat. Scaling up access to OIT will require expanding specialized training programs and developing more efficient treatment protocols.
Future Directions and Research
Improved Treatment Protocols
Research continues into optimizing OIT protocols to improve effectiveness while reducing risks. Studies are examining different dosing schedules, including accelerated protocols that might achieve desensitization more quickly. Other research focuses on identifying optimal maintenance doses and treatment durations.
Combination approaches that use multiple treatment modalities are under investigation. For example, combining biological therapies like omalizumab with OIT may allow higher doses to be tolerated and improve success rates. Probiotic supplements and other adjunct treatments are also being studied for their potential to enhance treatment outcomes.
Personalized treatment approaches based on individual patient characteristics represent another area of active research. Biomarkers that predict treatment response or risk of adverse reactions enable more tailored protocols. Genetic testing and advanced immune monitoring could guide future treatment decisions.
Novel Delivery Methods
Researchers are exploring alternative ways to deliver allergen immunotherapy that might be more convenient or safer than current approaches. Modified allergen proteins that retain their ability to induce tolerance while reducing allergic reactions are under development. These engineered proteins might allow for more effective treatment with fewer adverse effects.
Encapsulation technologies that could provide controlled release of allergens or protect them from digestion are also being investigated. These approaches might allow for less frequent dosing or more predictable allergen delivery. Nanoparticle-based delivery systems represent another promising area of research.
Alternative routes of administration beyond oral, skin, and sublingual approaches are being explored. These include nasal sprays, inhaled treatments, and injectable depot formulations. Each approach has potential advantages and limitations that need to be evaluated through clinical research.
Biomarker Development
Identifying reliable biomarkers to predict treatment response and monitor progress is a major research priority. Current monitoring relies mainly on clinical outcomes and periodic food challenges, which are burdensome and may not capture subtle changes in tolerance. Blood tests that could predict success or identify optimal treatment endpoints would improve clinical management.
Research is examining various immune markers, including specific antibody levels, immune cell responses, and inflammatory mediators. Machine learning approaches are being applied to identify patterns in these markers that might predict outcomes. Genetic markers are also under investigation for their potential to guide treatment decisions.
Point-of-care testing that could provide rapid results during clinic visits would be particularly valuable. Such tests could guide dose adjustments, identify patients at risk for reactions, and monitor treatment progress more effectively than current approaches.
Population-Level Implementation
Research into population-level implementation of OIT examines how these treatments might be scaled up to reach more patients safely and effectively. Studies are evaluating different models of care delivery, including shared care approaches between specialists and primary care providers.
Training and certification programs for healthcare providers are being developed to expand access to OIT. Standardized protocols and safety guidelines could allow more providers to offer these treatments while maintaining appropriate safety standards. Telemedicine approaches might help extend specialist expertise to underserved areas.
Public health approaches to food allergy prevention and treatment are also under investigation. Early-life interventions that might prevent the development of food allergies represent a complementary approach to treating established allergies. Population screening and early identification programs could help optimize treatment timing.
Conclusion 

Key Takeaways
Oral immunotherapy represents a major advance in food allergy treatment, offering the first therapy that can potentially reduce allergic sensitivity rather than simply managing reactions. The evidence from clinical trials demonstrates that OIT can desensitize many patients, protecting against accidental allergen exposures that could otherwise cause severe reactions.
However, OIT is not a simple cure for food allergies. The treatment requires substantial commitment from patients and families, carries risks of serious allergic reactions, and may need to be continued long-term to maintain benefits. Success rates vary among individuals, and not all patients are suitable candidates for treatment.
The current evidence supports OIT as a treatment option for carefully selected patients when performed in experienced medical centers with appropriate safety protocols. The treatment is most appropriate for patients with confirmed food allergies who are motivated to complete lengthy treatment protocols and can access specialized care for monitoring and management.
Safety considerations require that OIT be performed only by healthcare providers with expertise in allergy management and emergency treatment of severe reactions. Patients and families need extensive education about treatment protocols, reaction recognition, and emergency management. Access to emergency care and ongoing specialist support are essential components of safe treatment delivery.
The field continues to evolve rapidly with ongoing research into improved protocols, novel approaches, and better methods for predicting and monitoring treatment outcomes. Future developments may address current limitations and expand access to effective treatments for food allergies.
Frequently Asked Questions: 
Q: How long does oral immunotherapy treatment take?
A: Most OIT protocols require 6 to 24 months to reach maintenance doses, depending on the specific approach and individual patient response. The initial escalation phase typically takes several weeks to months, followed by a buildup phase that can last additional months. Once maintenance doses are reached, continued daily treatment is usually required to maintain desensitization.
Q: What are the success rates for oral immunotherapy?
A: Success rates vary depending on the food allergen and how success is defined. For peanut OIT, studies typically show desensitization rates of 60-80% for achieving tolerance to at least small amounts of peanut protein. However, fewer patients achieve tolerance to full serving sizes, and success rates may be lower in real-world clinical practice compared to research studies.
Q: Is oral immunotherapy safe for all patients with food allergies?
A: No, OIT is not appropriate for all patients. Candidates must be carefully selected based on factors including confirmed food allergy, controlled asthma, ability to follow treatment protocols, and access to specialized care. Patients with poorly controlled asthma, certain other medical conditions, or an inability to adhere to treatment protocols may not be suitable candidates.
Q: Can patients stop treatment once they complete oral immunotherapy?
A: Most patients need to continue consuming their allergen regularly to maintain desensitization. Some patients may achieve sustained tolerance that persists even without continued allergen exposure, but this cannot be reliably predicted. Stopping treatment often leads to gradual tolerance loss.
Q: How much does oral immunotherapy cost?
A: Costs vary depending on the specific treatment approach and location. FDA-approved treatments like Palforzia can cost thousands of dollars annually, and insurance coverage varies. Food-based protocols may have lower product costs but still require expensive, specialized medical care and monitoring. Many insurance plans do not fully cover OIT treatments.
Q: What should patients do if they have a reaction during treatment?
A: Patients should follow their individualized emergency action plans developed with their healthcare providers. Mild reactions may be managed with antihistamines, while severe reactions require epinephrine and emergency medical care. All reactions should be reported to the treatment team for evaluation and potential protocol adjustments.
Q: Can oral immunotherapy cure food allergies permanently?
A: OIT is not considered a permanent cure for most patients. While some individuals may achieve sustained tolerance that persists without continued treatment, many require ongoing allergen consumption to maintain their desensitization. The treatment is better understood as a management approach that can reduce reaction severity rather than a cure.
Q: How does oral immunotherapy compare to avoiding trigger foods?
A: Food avoidance remains the standard approach and is highly effective when complete avoidance can be achieved. OIT may provide additional protection against accidental exposures and could improve the quality of life for some patients. However, OIT carries risks that avoidance does not, and both approaches may be used together rather than one replacing the other.
References: 
Vickery, B. P., Vereda, A., Casale, T. B., Beyer, K., du Toit, G., Hourihane, J. O., Jones, S. M., Shreffler, W. G., Marcantonio, A., Zawadzki, R., Sher, L., Carr, W. W., Fineman, S., Greos, L., Rachid, R., Ibanez, M. D., Tilles, S., Assa’ad, A. H., Nilsson, C., Rupp, G. R., … PALISADE Group of Clinical Investigators. (2018). AR101 oral immunotherapy for peanut allergy. New England Journal of Medicine, 379(21), 1991-2001.
Nurmatov, U., Dhami, S., Arasi, S., Pajno, G. B., Fernandez-Rivas, M., Muraro, A., Roberts, G., Akdis, C., Akdis, M., Alvaro-Lozano, M., Beyer, K., Bindslev-Jensen, C., Burks, W., du Toit, G., Ebisawa, M., Eigenmann, P., Knol, E., Makela, M., Nadeau, K. C., O’Mahony, L., … Sheikh, A. (2017). Allergen immunotherapy for IgE-mediated food allergy: a systematic review and meta-analysis. Allergy, 72(8), 1133-1147.
Wasserman, R. L., Factor, J. M., Baker, J. W., Mansfield, L. E., Katz, Y., Hague, A. R., Paul, M. M., Sugerman, R. W., Lee, J. O., Lockey, R. F., Christie, L., Fordice, S., Murphy, K., Zeldin, R. K., Wenzel, J., Lasley, M. V., O’Brien, M. P., Mendelson, L. M., Fowler, J. A., Uvalle, C. E., … Adelman, D. C. (2011). Oral immunotherapy for peanut allergy: multipractice experience with epinephrine-treated reactions. Journal of Allergy and Clinical Immunology: In Practice, 2(1), 91-96.
Pajno, G. B., Fernandez-Rivas, M., Arasi, S., Roberts, G., Akdis, C. A., Alvaro-Lozano, M., Beyer, K., Bindslev-Jensen, C., Burks, W., Ebisawa, M., Eigenmann, P., Knol, E., Nadeau, K. C., Poulsen, L. K., van Ree, R., Santos, A. F., du Toit, G., Dhami, S., Nurmatov, U., Boloh, Y., … Sheikh, A. (2018). EAACI Guidelines on allergen immunotherapy: IgE-mediated food allergy. Allergy, 73(4), 799-815.
Wood, R. A., Kim, J. S., Lindblad, R., Nadeau, K., Henning, A. K., Dawson, P., Plaut, M., Sampson, H. A., & Consortium of Food Allergy Research (CoFAR). (2013). A randomized, double-anonymized, placebo-controlled study of omalizumab combined with oral immunotherapy for the treatment of cow’s milk allergy. Journal of Allergy and Clinical Immunology, 133(6), 1594-1602.
Jones, S. M., Sicherer, S. H., Burks, A. W., Leung, D. Y., Lindblad, R. W., Dawson, P., Henning, A. K., Berin, M. C., Chiang, D., Vickery, B. P., Pesek, R. D., Cho, C. B., Davidson, W. F., Plaut, M., Sampson, H. A., & Consortium of Food Allergy Research (CoFAR). (2017). Epicutaneous immunotherapy for the treatment of peanut allergy in children and young adults. Journal of Allergy and Clinical Immunology, 139(4), 1242-1252.
Fleischer, D. M., Burks, A. W., Vickery, B. P., Scurlock, A. M., Wood, R. A., Jones, S. M., Sicherer, S. H., Liu, A. H., Stablein, D., Henning, A. K., Mayer, L., Lindblad, R., Plaut, M., Sampson, H. A., & Consortium of Food Allergy Research. (2013). Sublingual immunotherapy for peanut allergy: a randomized, double-anonymized, placebo-controlled crossover trial. Journal of Allergy and Clinical Immunology, 131(1), 119-127.
Anagnostou, K., Islam, S., King, Y., Foley, L., Pasea, L., Bond, S., Palmer, C., Deighton, J., Ewan, P., & Clark, A. (2014). Assessing the efficacy of oral immunotherapy for the desensitisation of peanut allergy in children (STOP II): a phase 2 randomised controlled trial. Lancet, 383(9925), 1297-1304.
Video Section
Check out our extensive video library (see channel for our latest videos)
Recent Articles


