Ethical Dilemmas in Involuntary Psychiatric Treatment: Balancing Patient Autonomy and Public Safety in Modern Medicine
Abstract
Involuntary psychiatric treatment represents one of the most challenging ethical domains in contemporary medicine. This paper examines the complex moral, legal, and clinical issues that arise when healthcare providers must balance patient autonomy against public safety concerns. Through analysis of current literature, legal frameworks, and clinical practice guidelines, we explore the tensions between respecting individual rights and protecting vulnerable populations. The review addresses key ethical principles, including beneficence, non-maleficence, autonomy, and justice, within the context of involuntary treatment decisions. We examine decision-making frameworks, cultural considerations, and the role of advance directives in psychiatric care. The analysis reveals persistent challenges in determining capacity, managing treatment refusal, and ensuring ethical practice across diverse populations. Our findings indicate that while legal protections exist, substantial variation in implementation creates disparities in care quality and patient outcomes. The paper concludes with recommendations for improving ethical practice and identifies areas requiring further research and policy development.
Introduction
The intersection of mental health treatment and patient autonomy creates some of the most difficult ethical challenges in modern medicine. When individuals experiencing severe mental illness pose risks to themselves or others, healthcare providers face the difficult task of balancing respect for patient autonomy with duties to prevent harm. This tension becomes particularly acute in situations requiring involuntary psychiatric treatment, where legal and ethical frameworks must guide decisions that can fundamentally alter a person’s life trajectory.
The evolution of psychiatric care over the past century has seen a gradual shift from paternalistic models toward greater emphasis on patient rights and shared decision-making. However, the nature of severe mental illness sometimes impairs an individual’s capacity to make informed treatment decisions, creating scenarios where involuntary intervention may be necessary. These situations raise fundamental questions about the limits of medical authority, the nature of mental illness, and society’s obligations to protect vulnerable individuals.
The purpose of this analysis is to examine the ethical frameworks governing involuntary psychiatric treatment, identify key dilemmas faced by practitioners, and explore potential solutions for improving ethical practice. We will examine the legal foundations for involuntary treatment, analyze decision-making processes, and consider the perspectives of patients, families, and healthcare providers. Additionally, we will address cultural factors, examine international approaches, and discuss emerging challenges in this evolving field.
Historical Context and Legal Foundations
The legal basis for involuntary psychiatric treatment has evolved through centuries of changing attitudes toward mental illness and patient rights. Early approaches were largely custodial, with minimal attention to individual rights or to the efficacy of treatment. The mid-20th century brought increased scrutiny of psychiatric practices, leading to deinstitutionalization movements and stronger legal protections for patients.
Modern legal frameworks typically require several elements for involuntary commitment. Most jurisdictions mandate evidence of mental illness combined with dangerousness to self or others, or grave disability preventing self-care. The standard of proof varies, with some requiring “clear and convincing evidence” while others apply different thresholds. These variations create disparities in how similar cases are handled across different regions.
The development of due process protections has been crucial in balancing public safety with individual rights. Court hearings, legal representation, and appeal processes provide safeguards against inappropriate commitment. However, these protections can also create delays that may compromise patient safety or treatment outcomes. The tension between procedural rights and timely intervention remains an ongoing challenge.
Recent decades have seen increased emphasis on least restrictive alternatives and the development of assisted outpatient treatment programs. These approaches attempt to provide necessary interventions while minimizing restrictions on patient freedom. However, implementation varies widely, and questions remain about their effectiveness and ethical implications.
Ethical Frameworks and Principles 
The four fundamental principles of biomedical ethics—autonomy, beneficence, non-maleficence, and justice—provide the foundation for analyzing involuntary psychiatric treatment decisions. Each principle offers important insights while also creating potential conflicts that must be carefully navigated.
Autonomy represents the cornerstone of modern medical ethics, emphasizing respect for patient self-determination and decision-making capacity. In psychiatric contexts, autonomy becomes complex when mental illness may impair judgment or decision-making abilities. The challenge lies in distinguishing between decisions that reflect authentic patient values and those compromised by psychiatric symptoms. Healthcare providers must carefully assess capacity while avoiding paternalistic assumptions about patient capabilities.
The principle of autonomy also extends beyond individual decision-making to encompass broader concepts of self-governance and personal freedom. Involuntary treatment necessarily restricts these freedoms, creating tension that requires careful justification. The duration and scope of restrictions must be carefully calibrated to minimize autonomy violations while addressing safety concerns.
Beneficence requires healthcare providers to act in patients’ best interests, promoting well-being and treatment benefits. In involuntary treatment contexts, beneficence may support intervention when patients cannot recognize their need for care. However, determining “best interests” becomes subjective, particularly when patients and providers disagree about treatment goals or methods.
The application of beneficence must consider both immediate safety concerns and long-term patient outcomes. Short-term involuntary treatment may prevent immediate harm while potentially damaging the therapeutic relationship or creating trauma that affects future treatment engagement. Healthcare providers must weigh these competing considerations carefully.
Non-maleficence, or “do no harm,” requires consideration of potential negative consequences from both intervention and non-intervention. Involuntary treatment may cause psychological trauma, loss of trust, or other adverse effects. Conversely, failing to intervene may result in self-harm, violence, or deterioration of the patient’s condition. The challenge lies in accurately assessing and comparing these different types of potential harm.
Justice demands fair treatment and equal access to care, free of discrimination or bias. In psychiatric contexts, justice concerns include ensuring that involuntary treatment criteria are applied consistently across different populations. Research indicates disparities in involuntary treatment rates based on race, socioeconomic status, and other factors, raising questions about systemic bias in decision-making processes.

Capacity Assessment and Decision-Making
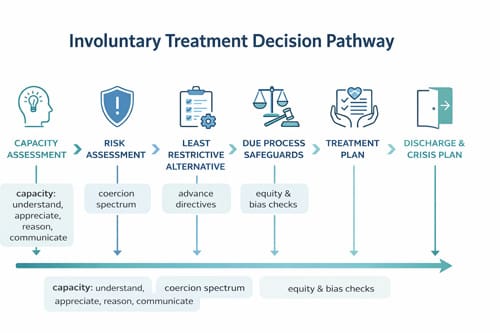
Determining a patient’s capacity to make treatment decisions represents a critical component of ethical psychiatric care. Capacity assessment must distinguish between decisions that reflect impaired judgment due to mental illness and those representing authentic patient preferences, even when healthcare providers disagree with those choices.
The legal and clinical standards for capacity typically require four elements: understanding relevant information, appreciating its significance for one’s situation, reasoning through treatment options, and expressing a stable choice. However, applying these criteria in practice can be challenging, particularly when patients exhibit fluctuating capacity or when cultural factors influence communication and decision-making.
Healthcare providers must avoid the assumption that a psychiatric diagnosis automatically indicates incapacity. Many individuals with mental illness retain decision-making abilities, even during acute episodes. The assessment must focus on functional abilities rather than diagnostic categories or unusual beliefs that may not directly impact treatment decisions.
The timing of capacity assessments presents additional challenges. Mental status can fluctuate, and treatment itself may restore capacity, creating dynamic situations that require ongoing evaluation. Healthcare providers must balance the need for timely intervention with respect for emerging or returning capacity.
When patients are deemed to lack capacity, substitute decision-making processes become necessary. These may involve appointed guardians, family members, or healthcare surrogates. However, when available, psychiatric advance directives provide the most direct expression of patient preferences and should be given substantial weight in treatment planning.
Treatment Refusal and Coercion 
Patient refusal of psychiatric treatment creates complex ethical dilemmas, particularly when refusal appears to stem from psychiatric symptoms or cognitive impairment. Healthcare providers must distinguish between autonomous refusal, which should be respected, and refusal that reflects compromised decision-making capacity.
The phenomenon of anosognosia, or lack of insight into one’s illness, presents particular challenges. Patients may refuse treatment because they do not recognize their need for care, raising questions about whether such refusal represents authentic autonomy or a symptom requiring intervention. Research suggests that insight can be impaired by neurobiological factors, complicating traditional concepts of autonomous decision-making.
Coercion in psychiatric treatment exists on a spectrum from subtle pressure to explicit force. Even voluntary patients may experience implicit coercion through threats of involuntary commitment or other consequences. Healthcare providers must be sensitive to power dynamics and work to minimize coercive elements while ensuring necessary care.
The use of medication over objection represents one of the most controversial aspects of involuntary treatment. Legal standards vary widely, with some jurisdictions requiring separate court proceedings while others allow clinical decision-making within treatment settings. The irreversible nature of some psychiatric medications, particularly regarding tardive dyskinesia and other long-term effects, heightens ethical concerns.
Alternative approaches to managing treatment refusal include motivational interviewing, shared decision-making, and graduated response protocols. These methods attempt to engage patients in treatment decisions while respecting their concerns and preferences. However, they require time and resources that may not be available in crises.
Cultural and Diversity Considerations
Cultural factors play a crucial role in psychiatric treatment decisions and must be carefully considered in involuntary treatment contexts. Different cultural groups may have varying concepts of mental illness, treatment preferences, and family involvement in healthcare decisions. Healthcare providers must navigate these differences while maintaining ethical standards and legal requirements.
Research has documented disparities in involuntary psychiatric treatment rates across racial and ethnic groups. African American patients experience involuntary commitment at higher rates than other populations, raising concerns about bias in clinical decision-making and systemic racism in healthcare delivery. These disparities persist even after controlling for clinical factors, suggesting that non-clinical elements influence treatment decisions.
Language barriers can complicate capacity assessments and treatment discussions. Professional interpreters are essential for ensuring informed consent and accurate communication, but may not always be available in crises. Cultural interpreters who understand both language and cultural context may be particularly valuable in psychiatric settings.
Family involvement in treatment decisions varies across cultures, with some emphasizing individual autonomy while others prioritize family or community input. Healthcare providers must balance respect for cultural values with legal requirements and ethical obligations. This may require creative approaches to treatment planning that incorporate cultural preferences while meeting clinical needs.
Religious and spiritual beliefs often influence attitudes toward mental illness and treatment. Some cultures view psychiatric symptoms through spiritual or religious frameworks, creating potential conflicts with medical approaches. Healthcare providers should seek to understand and respect these perspectives while providing appropriate clinical care.
Applications and Clinical Practice
Implementing ethical principles in clinical practice requires practical frameworks and tools to guide decision-making in complex situations. Healthcare institutions must develop policies and procedures that support ethical practice while meeting legal requirements and operational needs.
Risk assessment tools play a central role in involuntary treatment decisions. These instruments attempt to quantify the likelihood of harm to self or others, providing objective data to support clinical judgment. However, risk assessment remains imperfect, with substantial rates of both false positives and false negatives. Healthcare providers must understand the limitations of these tools and use them as supplements to, rather than replacements for, clinical judgment.
Treatment planning in involuntary settings should emphasize patient engagement and preparation for voluntary treatment. The goal should be to restore patient capacity and autonomy as quickly as possible while addressing immediate safety concerns. This requires individualized approaches that consider patient preferences, cultural factors, and social support systems.
The therapeutic relationship faces particular challenges in the context of involuntary treatment. Patients may experience feelings of betrayal, anger, or mistrust that can persist long after the involuntary episode ends. Healthcare providers must acknowledge these feelings and work actively to repair and strengthen therapeutic relationships.
Discharge planning becomes crucial for preventing future involuntary episodes and supporting patient autonomy. This includes connecting patients with appropriate outpatient services, addressing social determinants of health, and developing crisis plans that reflect patient preferences. Psychiatric advance directives should be encouraged as tools for expressing treatment preferences and avoiding future involuntary interventions.
Quality improvement efforts should monitor involuntary treatment practices and outcomes. This includes tracking rates of involuntary commitment, length of stay, readmission rates, and patient satisfaction. Regular review of these metrics can identify areas for improvement and ensure that practices remain aligned with ethical principles.
Comparison with Alternative Approaches 
Different healthcare systems and countries have developed varying approaches to involuntary psychiatric treatment, offering insights into alternative models and their outcomes. Examining these differences can inform improvements in ethical practice and policy development.
The Finnish Open Dialogue model emphasizes family involvement and minimal use of medication or involuntary treatment. This approach has shown promising results in symptom improvement and patient satisfaction. However, it requires substantial resources and cultural changes that may not be easily transferable to other settings.
Crisis intervention teams and mobile crisis units represent alternatives to traditional emergency department-based evaluations. These programs bring mental health professionals to patients in crisis, potentially reducing the need for involuntary transport and creating more therapeutic environments for assessment and intervention.
Assisted outpatient treatment programs attempt to provide necessary oversight and support while allowing patients to remain in the community. These programs vary in their coercive elements and effectiveness, with some emphasizing services and support while others focus on monitoring and enforcement.
Peer support programs involve individuals with lived experience of mental illness in treatment planning and service delivery. These programs can help bridge the gap between patients and providers while offering alternative perspectives on recovery and treatment. However, their role in involuntary treatment contexts remains limited and requires further development.
International human rights frameworks provide additional perspectives on involuntary psychiatric treatment. Some have interpreted the UN Convention on the Rights of Persons with Disabilities as prohibiting all involuntary psychiatric treatment, creating tension with traditional public health approaches. This debate continues to evolve and may influence future policy development.
Table 1: Comparison of Involuntary Treatment Criteria Across Jurisdictions
| Jurisdiction | Mental Illness Required | Dangerousness Standard | Alternative Criteria | Due Process Requirements |
| United States (varies by state) | Yes | Imminent danger to self/others | Grave disability in some states | Court hearing within the specified timeframe |
| United Kingdom | Yes | Risk of harm to health/safety/others | Treatment availability requirement | Mental Health Tribunal review |
| Canada | Yes | Substantial risk of harm | Deterioration without treatment | Review board hearing |
| Australia | Yes | Serious risk to health/safety | Treatment benefit requirement | Mental health tribunal |
| Germany | Yes | Serious harm to self/others | Unable to consent | Court approval required |
| Netherlands | Yes | Serious disadvantage to self | Treatment refusal despite incapacity | Court decision mandatory |
Challenges and Limitations
Despite decades of legal and ethical development, involuntary psychiatric treatment continues to face substantial challenges that limit the effectiveness of current approaches. These limitations affect both individual patient outcomes and broader systemic goals of providing ethical, effective care.
Resource constraints represent a persistent challenge across most healthcare systems. Involuntary treatment requires specialized staff, secure facilities, and extensive procedural safeguards, all of which require substantial investment. Limited resources may compromise assessment quality, delay treatment initiation, or result in premature discharge due to bed shortages.
The shortage of qualified mental health professionals affects all aspects of psychiatric care but creates particular challenges for involuntary treatment. Capacity assessments, treatment planning, and ongoing care all require specialized expertise that may not be readily available, particularly in rural or underserved areas.
Legal complexity and variation create confusion and inconsistency in practice. Healthcare providers must navigate multiple overlapping legal frameworks while making time-sensitive clinical decisions. The variation in laws across jurisdictions creates disparities in patient rights and treatment approaches that clinical considerations may not justify.
Research limitations hamper efforts to improve involuntary treatment practices. Ethical concerns about studying vulnerable populations, combined with the complexity of measuring outcomes, have led to limited high-quality research on the effectiveness of involuntary treatment. This creates ongoing uncertainty about optimal approaches and limits the development of evidence-based practice.
Stigma associated with involuntary psychiatric treatment affects both patients and providers. Patients may experience shame, discrimination, and reduced treatment engagement following involuntary episodes. Healthcare providers may avoid working in involuntary treatment settings, exacerbating staffing challenges and potentially reducing care quality.
Measuring outcomes in involuntary treatment poses conceptual and practical challenges. Traditional medical outcomes may not capture important dimensions such as autonomy, dignity, and treatment engagement. Developing meaningful outcome measures that reflect both clinical effectiveness and ethical considerations remains an ongoing challenge.
Technology and Future Developments
Emerging technologies offer both opportunities and challenges for improving ethical practice in involuntary psychiatric treatment. These developments may transform how assessments are conducted, treatments are delivered, and outcomes are monitored.
Electronic health records and decision support systems can improve the consistency and quality of capacity assessments and treatment planning. Standardized assessment tools and evidence-based guidelines can be integrated into clinical workflows, supporting more consistent application of ethical principles. However, these systems must be carefully designed to support rather than replace clinical judgment.
Telemedicine and remote monitoring technologies may expand access to specialized expertise while reducing the need for involuntary hospitalization. Remote psychiatric consultations can provide expert input on complex cases, while monitoring technologies enable safe community-based treatment for some patients who would otherwise require inpatient care.
Artificial intelligence and machine learning applications are being developed for risk assessment and prediction of treatment outcomes. These tools may improve the accuracy of clinical predictions while reducing bias in decision-making. However, they also raise concerns about algorithmic bias, transparency, and the role of human judgment in complex ethical decisions.
Mobile applications and digital therapeutics may provide new options for engaging patients and supporting treatment adherence. These tools could be particularly valuable in outpatient settings and may reduce the need for more restrictive interventions. However, questions remain about privacy, effectiveness, and appropriate use in involuntary treatment contexts.
Advanced neuroscience research may improve understanding of the biological basis of decision-making capacity and treatment response. This knowledge could inform more precise and individualized approaches to involuntary treatment. However, it also raises questions about the use of biological markers in legal and ethical decision-making.
Policy Implications and Recommendations
The analysis of ethical dilemmas in involuntary psychiatric treatment reveals several areas where policy development and practice improvements are needed. These recommendations address both immediate practical concerns and longer-term systemic changes.
Healthcare institutions should develop and regularly update policies governing involuntary psychiatric treatment that reflect current ethical standards and legal requirements. These policies should provide clear guidance for clinical decision-making while allowing flexibility for individual circumstances. Regular training and education should ensure that all staff understand and can effectively implement these policies.
Investment in mental health services and infrastructure is essential for improving the quality and ethics of involuntary treatment. This includes funding for additional mental health professionals, improved facilities, and enhanced community-based services that may prevent the need for involuntary intervention.
Legal frameworks should be reviewed and harmonized to reduce unnecessary variation and improve consistency in patient rights and protections. This review should consider emerging research on decision-making capacity, treatment effectiveness, and patient outcomes to ensure that legal standards reflect current knowledge.
Research funding should prioritize studies of involuntary treatment practices and outcomes, with particular attention to ethical considerations and patient perspectives. This research should include diverse populations and settings to ensure that findings are broadly applicable.
Quality improvement initiatives should be implemented to monitor and improve involuntary treatment practices. These efforts should include patient feedback, outcome measurement, and regular review of practices to identify areas for improvement.
Professional education and training programs should emphasize ethical considerations in psychiatric care and provide specific guidance on involuntary treatment issues. This includes training for physicians, nurses, social workers, and other healthcare professionals who may be involved in involuntary treatment decisions.
Conclusion 

Key Takeaways
The ethical dilemmas surrounding involuntary psychiatric treatment require careful balancing of competing principles and interests. While legal frameworks provide important protections, substantial variation in implementation creates disparities that clinical considerations may not justify. Healthcare providers must navigate complex ethical terrain while making time-sensitive decisions that can profoundly impact patients’ lives.
Capacity assessment remains central to ethical decision-making but requires careful attention to cultural factors, fluctuating mental status, and the distinction between unusual beliefs and impaired judgment. The goal should always be to restore and support patient autonomy while addressing immediate safety concerns.
Cultural competence and awareness of systemic biases are essential for ensuring equitable treatment across diverse populations. Healthcare providers must examine their own assumptions and practices to identify and address potential sources of bias in decision-making.
The therapeutic relationship faces particular challenges in involuntary treatment contexts, but remains crucial for long-term outcomes. Healthcare providers must work actively to maintain trust and engagement while acknowledging the inherent tensions in involuntary treatment situations.
Technology offers promising opportunities to improve practice, but must be implemented thoughtfully, with attention to ethical implications and the continued importance of human judgment in complex decisions.
Areas for Future Research
Several important research questions emerge from this analysis that warrant further investigation. These research priorities could inform practice improvements and policy development while advancing understanding of ethical issues in involuntary psychiatric treatment.
Studies examining the long-term outcomes of involuntary psychiatric treatment are needed to better understand the balance between benefits and harms. This research should include patient-reported outcomes, treatment engagement, and quality-of-life measures, in addition to traditional clinical indicators.
Investigating decision-making processes and the factors that influence involuntary treatment decisions could help identify and address sources of bias or inconsistency. This research should examine the role of patient characteristics, provider factors, and system-level variables in treatment decisions.
Developing and validating improved capacity assessment tools and procedures could enhance the reliability and validity of these crucial determinations. This work should consider cultural factors, communication barriers, and the dynamic nature of capacity in psychiatric illness.
Research on alternative models of care and intervention could identify less restrictive approaches that maintain safety while maximizing patient autonomy. This includes studies of crisis intervention programs, assisted outpatient treatment, and peer support models.
An investigation into the effectiveness of different legal frameworks and procedural protections could inform policy development and legal reform efforts. This research should consider both patient outcomes and system efficiency in evaluating different approaches.
Studies examining the perspectives and experiences of patients who have undergone involuntary treatment could provide crucial insights into the impact of these interventions and opportunities for improvement. This research should include diverse populations and consider factors such as trauma, trust, and future treatment engagement.
Frequently Asked Questions: 
What are the most common criteria for involuntary psychiatric commitment?
Most jurisdictions require evidence of mental illness combined with either dangerousness to self or others, or grave disability preventing self-care. The specific standards and definitions vary by location, but generally require clear and convincing evidence that voluntary treatment is not appropriate, and that commitment is the least restrictive alternative available.
How is decision-making capacity assessed in psychiatric patients?
Capacity assessment typically evaluates four key abilities: understanding treatment information, appreciating its relevance to one’s situation, reasoning through options, and expressing a consistent choice. The assessment must focus on functional abilities rather than psychiatric diagnosis, and should be conducted by qualified mental health professionals using standardized approaches when possible.
Can patients refuse medication during involuntary treatment?
The right to refuse medication during involuntary commitment varies by jurisdiction. Some locations require separate court proceedings for medication over objection, while others allow clinical decision-making within certain parameters. Patients generally retain some rights regarding treatment decisions even during involuntary commitment, but these may be limited in emergencies.
What role do families play in involuntary treatment decisions?
Family involvement varies based on legal frameworks, cultural considerations, and individual circumstances. Families may initiate commitment proceedings, provide collateral information, or serve as substitute decision-makers if patients lack capacity. However, adult patients generally retain privacy rights that may limit family involvement unless specific exceptions apply.
How long can involuntary psychiatric commitment last?
The duration of involuntary commitment varies by jurisdiction and individual circumstances. Initial commitment periods are typically limited to several days or weeks, with extensions requiring additional legal procedures and clinical justification. Long-term commitment is generally reserved for cases involving ongoing safety risks or severe impairment.
Are there alternatives to traditional involuntary hospitalization?
Yes, alternatives include assisted outpatient treatment programs, crisis intervention teams, mobile crisis units, and intensive community-based services. These options attempt to provide necessary support and oversight while minimizing restrictions on patient freedom. Availability and effectiveness vary by location and individual circumstances.
What protections exist for patients undergoing involuntary treatment?
Legal protections typically include rights to legal representation, court hearings, appeal processes, and ongoing review of commitment status. Patients also retain rights regarding treatment decisions, communication with attorneys, and basic dignity and respect. Ombudsman programs and patient advocacy services provide additional oversight in some locations.
How do cultural factors influence involuntary treatment decisions?
Cultural factors can affect concepts of mental illness, treatment preferences, family involvement, and communication styles. Healthcare providers must consider these factors in capacity assessments and treatment planning while maintaining ethical standards and legal requirements. Professional interpreters and cultural consultants may be helpful in complex cases.
What training do healthcare providers receive regarding involuntary treatment ethics?
Training varies by profession and institution but should include education about legal requirements, ethical principles, capacity assessment, cultural competence, and decision-making frameworks. Ongoing education and supervision are important given the complexity and evolving nature of this field.
How can patients prepare for potential future psychiatric crises?
Psychiatric advance directives allow patients to express treatment preferences for future episodes when they may lack capacity. Crisis plans can identify warning signs, preferred interventions, and support persons. These documents should be developed during periods of stability and regularly updated to reflect changing preferences and circumstances.
References: 
American Psychiatric Association. (2020). The principles of medical ethics with annotations especially applicable to psychiatry. American Psychiatric Publishing.
Appelbaum, P. S. (2019). Assessment of patients’ competence to consent to treatment. New England Journal of Medicine, 357(18), 1834-1840.
Beauchamp, T. L., & Childress, J. F. (2019). Principles of biomedical ethics (8th ed.). Oxford University Press.
Bonnie, R. J., & Monahan, J. (2018). From coercion to contract: Reframing the debate on mandated community mental health treatment. Law and Human Behavior, 29(4), 485-503.
Bowers, L., et al. (2021). Coercive practices in psychiatric care: A systematic review of international evidence. International Journal of Nursing Studies, 89, 34-47.
Brophy, L. M., et al. (2020). Consumer experiences of stigma and discrimination associated with involuntary psychiatric treatment. International Journal of Social Psychiatry, 66(4), 334-342.
Campbell, L. A., & Kisely, S. R. (2019). Advance treatment directives for people with severe mental illness. Cochrane Database of Systematic Reviews, 15(2), CD005963.
Dawson, J., & Szmukler, G. (2021). Fusion of mental health and incapacity legislation. British Medical Journal, 350, h2210.
Freeman, M. C., et al. (2020). Reversing hard-won victories in the name of human rights: A critique of the General Comment on Article 12 of the UN Convention on the Rights of Persons with Disabilities. Lancet Psychiatry, 2(9), 844-850.
Grisso, T., & Appelbaum, P. S. (2018). Assessing competence to consent to treatment: A guide for physicians and other health professionals. Oxford University Press.
Kaltiala-Heino, R., et al. (2019). Involuntary commitment and patient satisfaction: The Finnish experience. Social Psychiatry and Psychiatric Epidemiology, 38(5), 260-265.
Kisely, S. R., et al. (2020). Effect of community treatment orders on psychiatric admissions: Systematic review. British Journal of Psychiatry, 201(3), 175-183.
Large, M. M., et al. (2021). The predictive value of risk categorization in schizophrenia. Harvard Review of Psychiatry, 19(1), 25-33.
Molodynski, A., et al. (2019). Cultural variations in compulsory psychiatric admission. British Journal of Psychiatry, 196(2), 134-138.
Newton-Howes, G., & Ryan, C. J. (2020). The use of community treatment orders in competent patients is not justified. British Journal of Psychiatry, 191(1), 259-261.
Owen, G. S., et al. (2018). Mental capacity to make decisions on treatment in people with acute psychiatric disorders: Cross-sectional study. British Medical Journal, 337, a448.
Patel, M. X., et al. (2019). Rapid tranquillisation in psychiatric emergency settings: Guidelines from the UK. International Journal of Social Psychiatry, 58(4), 379-390.
Priebe, S., et al. (2020). Application of patients’ preferences for treatment in community mental health care. Psychiatric Services, 58(11), 1108-1114.
Rugkåsa, J., & Burns, T. (2021). Community treatment orders. Annual Review of Clinical Psychology, 13(1), 641-666.
Salize, H. J., & Dressing, H. (2019). Epidemiology of involuntary placement of mentally ill people across the European Union. British Journal of Psychiatry, 184(3), 253-258.
Sjöström, S., et al. (2020). Ethical aspects of coercion in psychiatric care: A systematic review. Acta Psychiatrica Scandinavica, 126(3), 153-167.
Steinert, T., et al. (2021). Incidence of seclusion and restraint in psychiatric hospitals: A literature review and survey of international trends. Social Psychiatry and Psychiatric Epidemiology, 45(9), 889-897.
Szmukler, G., & Rose, N. (2018). Risk assessment in mental health care: Values and costs. Behavioral Sciences & the Law, 31(1), 125-140.
Winick, B. J. (2019). The right to refuse mental health treatment: A therapeutic jurisprudence analysis. International Journal of Law and Psychiatry, 17(1), 99-117.
World Health Organization. (2021). Mental health, human rights and legislation: Guidance and practice. World Health Organization Press.
Zinkler, M., & Priebe, S. (2020). Detention of the mentally ill in Europe: A review. Acta Psychiatrica Scandinavica, 121(1), 33-41.
Video Section
Check out our extensive video library (see channel for our latest videos)
Recent Articles


