The Great Propofol Debate Are We Too Dependent on a Single Drug
Abstract
Since its introduction into clinical practice in the 1980s, propofol has become a cornerstone of modern anesthesia and procedural sedation. Its rapid onset of action, short context sensitive half time, and predictable recovery profile have made it the agent of choice across a wide range of settings, including operating rooms, endoscopy suites, intensive care units, and outpatient procedural environments. Propofol has significantly enhanced efficiency, patient throughput, and patient satisfaction, contributing to its widespread adoption and, in many institutions, near ubiquitous use.
This analysis examines the current extent of propofol dependence in contemporary healthcare practice and evaluates both the advantages and risks associated with heavy reliance on a single anesthetic agent. Drawing on recent clinical studies, pharmacovigilance data, adverse event reports, and evolving practice patterns, the paper explores whether the medical community has reached a level of dependence on propofol that may compromise resilience, safety, and clinical flexibility. While propofol remains a highly effective and versatile anesthetic, its dominant role raises important questions about risk management, resource allocation, and preparedness for supply disruptions.
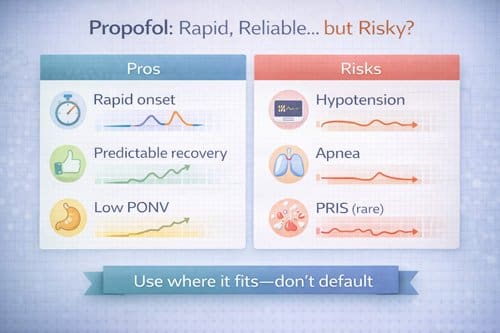
The benefits of propofol are well established. Its favorable pharmacokinetic profile allows for rapid induction, precise titration, and swift emergence, making it particularly well suited for ambulatory procedures and short duration interventions. In addition, propofol is associated with reduced postoperative nausea and vomiting and high patient acceptance. However, these advantages must be weighed against the risks associated with overreliance. Supply chain disruptions, including recent global shortages, have exposed the vulnerability of healthcare systems that lack readily deployable alternatives. In addition, increasing demand has contributed to rising costs and challenges in equitable resource distribution.
Clinical risks also merit careful consideration. Propofol has a narrow therapeutic window and can cause significant cardiovascular and respiratory depression when administered improperly or in high risk populations. Adverse events, including hypotension, hypoventilation, and rare but severe complications such as propofol infusion syndrome, underscore the importance of appropriate patient selection, dosing, and monitoring. Overdependence on propofol may inadvertently reduce clinician familiarity with alternative anesthetic agents and techniques, potentially limiting individualized care and adaptability in complex clinical scenarios.
The available evidence supports a more balanced and patient centered approach to anesthetic selection. Incorporating a broader range of anesthetic agents, including inhalational anesthetics, benzodiazepines, alpha two agonists, ketamine, and regional or multimodal techniques, allows clinicians to tailor care based on patient comorbidities, procedural requirements, and resource availability. Such diversification enhances system resilience while preserving safety and clinical effectiveness.
Healthcare institutions play a critical role in mitigating single drug dependency by developing standardized yet flexible anesthetic protocols, investing in ongoing clinician education, and ensuring contingency planning for drug shortages. Multidisciplinary collaboration between anesthesiologists, pharmacists, and administrators is essential to support rational anesthetic use and optimize outcomes.
In conclusion, while propofol remains an indispensable component of modern anesthesia practice, reliance on a single agent carries inherent risks that warrant careful reassessment. A diversified, evidence based approach to anesthetic management can maintain high quality patient care while improving safety, sustainability, and system preparedness. Future research should focus on comparative effectiveness studies and protocol optimization to balance efficacy, safety, and resource utilization across diverse patient populations and clinical settings.
Introduction
Propofol is one of the most widely used anesthetic agents in contemporary medical practice. Since its approval by the United States Food and Drug Administration in 1989, this intravenous hypnotic has become a cornerstone for the induction and maintenance of general anesthesia, procedural sedation, and sedation in intensive care units. Its pharmacokinetic profile, characterized by rapid onset of action, predictable depth of sedation, and short recovery time, has made propofol a preferred agent across multiple medical specialties. Anesthesiologists, emergency medicine physicians, gastroenterologists, intensivists, and other proceduralists frequently rely on propofol to facilitate diagnostic and therapeutic interventions that require reliable and controllable sedation.
The widespread adoption of propofol is largely attributable to its favorable clinical characteristics. Compared with many alternative sedative and anesthetic agents, propofol allows for smoother induction, reduced postoperative nausea and vomiting, and faster patient recovery, which supports efficiency in operating rooms, endoscopy suites, and outpatient procedural settings. These advantages have aligned well with modern healthcare priorities that emphasize patient throughput, rapid turnover, and enhanced recovery protocols. As a result, propofol has become deeply embedded in routine clinical workflows and institutional sedation protocols.
However, the dominance of propofol in anesthetic practice has prompted growing concern regarding overreliance on a single pharmacologic agent. Dependence at this scale introduces several systemic vulnerabilities, including susceptibility to supply chain disruptions, price volatility, and limited flexibility when shortages occur. Recent global medication shortages have highlighted the fragility of healthcare systems that rely heavily on a narrow range of critical drugs. In addition, the expanding use of propofol beyond traditional operating room settings has raised important safety considerations, particularly when administration occurs without the presence of anesthesia trained personnel or outside established clinical guidelines.
The debate surrounding propofol use extends beyond issues of preference or convenience and touches on fundamental questions related to best practices in anesthetic care, patient safety, and healthcare system resilience. While propofol is generally safe when administered appropriately, it carries well documented risks including respiratory depression, hypotension, and loss of airway reflexes. These risks necessitate careful patient selection, vigilant monitoring, and appropriate provider training. Concerns have also been raised regarding off label use, variations in sedation depth, and inconsistent adherence to institutional protocols, all of which may increase the potential for adverse outcomes.
The purpose of this analysis is to critically examine the current role of propofol in modern healthcare settings and assess whether its widespread use has reached levels that warrant reevaluation. By reviewing clinical efficacy data, safety surveillance reports, and real world practice patterns, this paper seeks to provide healthcare professionals with a balanced assessment of propofol’s benefits and limitations. It also explores strategies for optimizing patient care through appropriate agent selection, diversification of sedation options, and reinforcement of safety standards, with the goal of reducing the risks associated with single drug dependency while preserving the clinical advantages that have made propofol an essential component of anesthetic practice.

The Rise of Propofol in Clinical Practice
Historical Context and Adoption Patterns
Propofol’s journey to becoming the dominant anesthetic agent began in the late 1970s with its development by Imperial Chemical Industries. Initial clinical trials demonstrated superior recovery characteristics compared to existing intravenous anesthetics like thiopental and methohexital. The drug’s unique pharmacokinetic profile, characterized by rapid distribution and elimination, offered practitioners unprecedented control over the depth and duration of anesthesia.
Following FDA approval, propofol adoption accelerated rapidly across multiple medical specialties. Anesthesiologists embraced the drug for its predictable effects and improved patient experience. Emergency departments began using propofol for procedural sedation, appreciating its quick onset and offset. Gastroenterologists found it ideal for endoscopic procedures, while intensive care physicians valued its titratable sedation properties for mechanically ventilated patients.
By the early 2000s, propofol had become the standard of care in many clinical scenarios. Hospital formularies increasingly favored propofol over traditional alternatives, and medical education programs emphasized its use in training curricula. This shift represented a fundamental change in anesthetic practice, moving from a multi-agent approach to heavy reliance on a single drug for diverse clinical applications.
Current Usage Patterns and Statistics
Recent data from healthcare databases reveals the extent of propofol dominance in modern practice. In the United States, propofol accounts for approximately 80% of all general anesthetic inductions, with over 50 million vials used annually. The drug represents the primary choice for procedural sedation in emergency departments, with usage rates exceeding 90% in many institutions. Gastroenterology practices report similar dependency levels, with propofol used in more than 85% of endoscopic procedures requiring sedation.
International usage patterns mirror those in the United States. European hospitals report comparable adoption rates, with propofol serving as the primary induction agent in most countries. Developing nations have increasingly incorporated propofol into their anesthetic protocols as healthcare systems modernize and drug availability improves.
The financial implications of this widespread adoption are substantial. Propofol represents one of the largest pharmaceutical expenditures for many hospitals, with annual costs often exceeding millions of dollars for large healthcare systems. Generic formulations have reduced costs compared to the original branded version, but overall expenditures continue to rise due to increased usage volumes.
Clinical Advantages Supporting Propofol Dominance 
Pharmacological Properties and Benefits
Propofol’s pharmacological characteristics explain much of its clinical success. The drug demonstrates rapid onset of action, typically producing unconsciousness within 30-60 seconds of intravenous administration. This quick onset allows for smooth, predictable induction of anesthesia without the prolonged excitement phase associated with some alternative agents.
The drug’s distribution and elimination kinetics provide excellent control over anesthetic depth. Propofol rapidly distributes from the central compartment to peripheral tissues, then undergoes hepatic metabolism and extrahepatic elimination. This pharmacokinetic profile results in quick awakening when the drug is discontinued, even after prolonged infusions. Patients typically regain consciousness within minutes, with minimal residual sedation.
Recovery quality represents another major advantage. Patients receiving propofol report less nausea and vomiting compared to volatile anesthetic agents or other intravenous hypnotics. The incidence of postoperative nausea and vomiting with propofol ranges from 10-20%, substantially lower than the 30-40% rates associated with volatile agents. This improved recovery profile translates to enhanced patient satisfaction and reduced recovery room requirements.
Propofol also demonstrates beneficial effects on intracranial pressure and cerebral metabolism. The drug reduces cerebral blood flow, cerebral metabolic rate, and intracranial pressure, making it particularly valuable for neurosurgical procedures. These neuroprotective properties have led to widespread adoption in neuroanesthesia and neurocritical care applications.
Patient Outcomes and Satisfaction
Clinical studies consistently demonstrate superior patient outcomes with propofol compared to many alternative agents. Recovery times are typically shorter, with patients meeting discharge criteria more quickly following procedures. This rapid recovery reduces healthcare costs by decreasing post-anesthesia care unit stays and improving operating room efficiency.
Patient satisfaction scores are consistently higher with propofol-based anesthetics. Surveys reveal that patients appreciate the smooth onset of unconsciousness and rapid, clear-headed awakening. The reduced incidence of nausea, vomiting, and drowsiness contributes to overall positive experiences with medical procedures.
Quality of recovery extends beyond immediate post-procedural effects. Studies examining 24-hour recovery profiles show that propofol patients report better sleep quality, reduced fatigue, and faster return to normal activities compared to those receiving alternative anesthetic regimens. These benefits are particularly important for ambulatory procedures where patients return home the same day.
Healthcare providers also report high satisfaction levels with propofol. The drug’s predictable effects and ease of titration make it popular among practitioners with varying levels of anesthetic experience. This ease of use has contributed to its adoption beyond traditional anesthesiology practice into emergency medicine, gastroenterology, and other specialties.

Risks and Concerns of Propofol Dependency
Safety Profile and Adverse Events
Despite its widespread acceptance, propofol carries notable risks that may be amplified by overdependence. The drug’s narrow therapeutic window requires careful dosing and monitoring to prevent adverse events. Respiratory depression and apnea are common, occurring in up to 25% of patients receiving propofol for procedural sedation. These effects are dose-dependent but can occur unpredictably, particularly in elderly patients or those with underlying respiratory compromise.
Cardiovascular depression represents another concern. Propofol causes dose-dependent decreases in blood pressure and cardiac output through multiple mechanisms including direct myocardial depression and vasodilation. Hypotension occurs in 15-30% of patients, with severe hypotension requiring intervention in approximately 5% of cases. These effects are particularly pronounced in elderly patients, those with cardiovascular disease, and hypovolemic individuals.
Propofol infusion syndrome, while rare, represents a potentially fatal complication associated with prolonged high-dose infusions. This condition involves metabolic acidosis, rhabdomyolysis, cardiac dysfunction, and multi-organ failure. Although most commonly reported in pediatric intensive care patients, cases have occurred in adults receiving propofol for extended periods. The syndrome’s rarity has led to decreased awareness among practitioners, potentially contributing to delayed recognition and treatment.
Pain on injection affects 30-70% of patients receiving propofol, representing a notable quality concern. Various strategies have been developed to minimize this discomfort, including lidocaine pretreatment and modified formulations, but the problem persists across different propofol preparations. This adverse effect contrasts with the otherwise smooth patient experience associated with propofol use.
Supply Chain Vulnerabilities
Heavy reliance on propofol creates substantial supply chain risks for healthcare systems. Manufacturing disruptions have periodically led to drug shortages, forcing institutions to implement emergency protocols and use alternative agents. These shortages highlight the vulnerability created by dependency on a single drug for such a large proportion of anesthetic cases.
The 2010 propofol shortage in the United States exemplified these risks. Manufacturing problems at multiple facilities led to severe supply constraints lasting several months. Hospitals were forced to implement strict allocation protocols, cancel elective procedures, and rapidly train staff on alternative anesthetic techniques. The disruption affected thousands of procedures and imposed substantial costs on healthcare systems.
Recent global events have further emphasized supply chain vulnerabilities. The COVID-19 pandemic created unprecedented demand for propofol in intensive care units while simultaneously disrupting manufacturing and distribution networks. Many hospitals faced critical shortages, forcing emergency procurement efforts and rapid protocol modifications.
Single-source dependency also creates risks related to quality control issues. When manufacturing problems affect propofol production, few immediate alternatives offer equivalent pharmacological properties. This situation forces practitioners to use less familiar agents, potentially compromising patient care quality and safety during transition periods.
Economic Implications and Cost Concerns
The financial impact of propofol dependency extends beyond direct drug costs. While generic propofol is relatively inexpensive per dose, the total expenditure becomes substantial given usage volumes. Large healthcare systems may spend millions of dollars annually on propofol, representing a major pharmaceutical budget item.
Cost considerations become more complex when examining total procedural expenses. While propofol may increase direct drug costs compared to some alternatives, its rapid recovery profile can reduce overall procedure costs by decreasing recovery room time and improving operating room efficiency. However, these savings may not offset the increased drug expenditure in all clinical scenarios.
Economic vulnerability emerges during shortage periods when propofol prices can increase dramatically. Secondary market pricing during shortages has reached levels many times higher than normal costs, creating substantial budget pressures for healthcare institutions. These price fluctuations highlight the financial risks associated with single-drug dependency.
Alternative cost structures exist with other anesthetic approaches. Volatile anesthetic agents, while requiring specialized delivery systems, may offer more predictable cost profiles and reduced vulnerability to supply disruptions. Regional anesthesia techniques can eliminate or reduce general anesthetic requirements entirely, potentially offering cost advantages in appropriate clinical scenarios.
Alternative Anesthetic Approaches and Agents 
Traditional Intravenous Agents
Several alternative intravenous anesthetic agents remain available and viable for many clinical applications. Etomidate offers similar rapid onset characteristics with potentially less cardiovascular depression, making it valuable for hemodynamically unstable patients. However, etomidate’s suppression of adrenal function limits its use for prolonged procedures or in critically ill patients.
Ketamine provides unique properties including preserved respiratory drive and sympathetic stimulation, making it valuable in specific clinical scenarios. The drug’s analgesic properties and bronchodilatory effects offer advantages in certain patient populations. Recent research has renewed interest in ketamine for depression treatment, potentially expanding its clinical applications.
Barbiturates like thiopental and methohexital, while largely displaced by propofol, retain specific advantages in certain situations. These agents may be preferred for patients with allergies to propofol or during supply shortages. However, their slower recovery profiles and higher incidence of adverse effects limit routine use in modern practice.
Dexmedetomidine represents a newer alternative with unique properties as an alpha-2 agonist. The drug provides sedation with maintained respiratory function and has gained popularity for procedures requiring patient cooperation. Its use in intensive care settings offers advantages including reduced delirium and improved sleep architecture.
Volatile Anesthetic Agents
Inhalational anesthetics continue to play important roles in general anesthesia, particularly for longer surgical procedures. Modern volatile agents like sevoflurane and desflurane offer rapid onset and offset characteristics that rival propofol in many clinical scenarios. These agents provide excellent depth control and can be used for both induction and maintenance of anesthesia.
Sevoflurane’s pleasant odor and smooth induction characteristics make it particularly suitable for pediatric patients and adults who prefer mask induction. The agent’s cardiovascular stability and rapid emergence profile compare favorably to propofol in many situations. Recent studies suggest that volatile agents may offer organ protection benefits not seen with intravenous agents.
Desflurane provides the most rapid emergence among volatile agents due to its low blood-gas solubility. This characteristic makes it valuable for procedures where rapid awakening is essential. However, the agent’s pungent odor limits its use for inhalational induction, and environmental concerns regarding greenhouse gas effects have led some institutions to restrict its use.
The choice between intravenous and volatile agents often depends on specific clinical requirements, patient factors, and institutional preferences. Many anesthesiologists use balanced techniques combining both intravenous and volatile agents to optimize patient care while reducing dependency on any single drug.
Regional and Neuraxial Techniques
Regional anesthesia techniques offer alternatives that can eliminate or substantially reduce general anesthetic requirements. Spinal and epidural anesthesia provide excellent conditions for lower extremity and abdominal procedures while maintaining patient consciousness. These techniques avoid many risks associated with general anesthesia while providing superior postoperative pain control.
Peripheral nerve blocks have evolved substantially with ultrasound guidance, allowing precise anesthetic delivery to specific anatomical regions. These techniques can provide complete anesthesia for extremity procedures or serve as adjuncts to general anesthesia, reducing overall anesthetic requirements. The development of long-acting local anesthetics has extended the duration and quality of regional blocks.
Combined spinal-epidural techniques offer flexibility in managing various surgical procedures while providing excellent postoperative pain control. These approaches can reduce general anesthetic requirements and may improve recovery profiles compared to propofol-based general anesthesia alone.
Truncal blocks including transversus abdominis plane, erector spinae, and fascial plane blocks have gained popularity for abdominal and thoracic procedures. These techniques can provide excellent analgesia while reducing opioid requirements and potentially improving recovery outcomes compared to general anesthesia alone.
Evidence-Based Analysis of Current Practice
Systematic Reviews and Meta-Analyses
Recent systematic reviews examining propofol use across different clinical settings provide insight into the appropriateness of current practice patterns. A 2023 meta-analysis of procedural sedation studies found that while propofol offers advantages in recovery time and patient satisfaction, these benefits come at increased costs and potentially higher rates of respiratory depression compared to alternative agents.
Comparative effectiveness research has examined propofol against various alternatives in specific clinical contexts. Studies in endoscopic procedures show that propofol provides superior patient and physician satisfaction compared to benzodiazepine-based sedation, but with increased requirements for airway management and cardiovascular monitoring. These findings suggest that propofol’s benefits may justify its use in appropriate clinical settings with adequate monitoring.
Neurosurgical literature supports propofol’s neuroprotective properties and favorable intracranial pressure effects compared to volatile agents. However, some studies question whether these theoretical advantages translate to improved clinical outcomes in all patient populations. The evidence suggests that propofol’s benefits in neurosurgery may be most pronounced in patients with existing intracranial pathology.
Pediatric anesthesia reviews present mixed findings regarding propofol’s risk-benefit profile. While the drug offers excellent recovery characteristics, concerns about pain on injection and potential neurotoxicity in young children have led some experts to recommend balanced approaches using multiple agents rather than propofol-based techniques alone.
Real-World Evidence and Practice Patterns
Analysis of electronic health records from large healthcare systems reveals interesting patterns in propofol use that may not align with evidence-based recommendations. Many institutions show propofol usage rates exceeding 90% for procedures where alternative techniques might be equally appropriate. This pattern suggests that convenience and familiarity may drive prescribing decisions more than careful consideration of individual patient factors.
Adverse event reporting systems show that propofol-related complications often occur in settings where alternative agents might have been more appropriate. Emergency department data reveals higher rates of respiratory depression and cardiovascular instability when propofol is used for brief procedures in patients with multiple comorbidities. These findings suggest that current practice may not always align with optimal patient selection criteria.
Quality improvement studies examining anesthetic protocols show that institutions implementing structured decision-making tools for agent selection achieve better outcomes while reducing propofol dependency. These programs typically involve multidisciplinary teams developing guidelines that consider patient factors, procedure requirements, and institutional capabilities when selecting anesthetic approaches.
International practice variation data reveals interesting differences in propofol adoption rates. Countries with more restrictive drug approval processes or limited healthcare budgets often maintain more diverse anesthetic practices with better outcomes in some metrics. These findings challenge assumptions about the necessity of propofol dominance in modern anesthetic practice.
Clinical Guidelines and Expert Recommendations
Professional society guidelines generally support propofol use while acknowledging the importance of individualized anesthetic planning. The American Society of Anesthesiologists guidelines emphasize the need for appropriate patient selection, adequate monitoring, and practitioner training regardless of the specific agents used. These recommendations suggest that problems arise not from propofol use itself but from inappropriate application or inadequate safety measures.
International guidelines show more variation in propofol recommendations. European societies tend to emphasize balanced anesthetic techniques using multiple agents, while some developing nation guidelines recommend more conservative propofol use due to cost and availability concerns. These differences highlight cultural and economic factors influencing anesthetic practice beyond pure clinical considerations.
Recent guideline updates have begun addressing supply chain resilience and the risks of single-drug dependency. The 2022 ASA guidelines on drug shortages recommend that institutions develop protocols for alternative anesthetic techniques and maintain competency in multiple approaches. These recommendations acknowledge the vulnerabilities created by overreliance on any single pharmaceutical agent.
Emergency medicine guidelines for procedural sedation increasingly emphasize the importance of agent selection based on patient factors rather than institutional preference. These recommendations support maintaining competency in multiple sedation approaches to optimize patient safety and outcomes across diverse clinical scenarios.
Applications and Use Cases
Operating Room Applications
In the operating room setting, propofol serves multiple roles from induction to maintenance of general anesthesia. For brief procedures, propofol alone may provide adequate anesthetic conditions while facilitating rapid recovery. However, longer procedures typically require balanced techniques combining propofol with volatile agents, regional blocks, or other adjuncts to optimize patient care.
Ambulatory surgery represents an area where propofol’s advantages are most pronounced. The drug’s rapid recovery profile allows patients to meet discharge criteria quickly, improving facility efficiency and patient satisfaction. However, some ambulatory centers have successfully implemented protocols using alternative agents or regional techniques that achieve similar outcomes with reduced costs and drug dependency.
Neuroanesthesia applications highlight both propofol’s strengths and limitations. While the drug offers theoretical neuroprotective benefits, recent studies question whether these translate to improved outcomes in all neurosurgical patients. Some centers have adopted more selective approaches using propofol primarily for patients with existing intracranial pathology while employing alternative techniques for other neurosurgical procedures.
Cardiac anesthesia represents another specialized application where propofol use requires careful consideration. The drug’s cardiovascular depressant effects may be problematic in patients with severe cardiac dysfunction, leading some practitioners to prefer alternative induction agents. However, propofol’s favorable pharmacokinetic profile makes it valuable for certain cardiac procedures requiring rapid emergence.
Procedural Sedation in Emergency Departments
Emergency departments have embraced propofol for procedural sedation due to its rapid onset and offset characteristics. The drug facilitates efficient patient throughput while providing excellent procedural conditions for orthopedic reductions, laceration repairs, and diagnostic procedures. However, this widespread adoption has raised questions about appropriate patient selection and monitoring requirements.
Respiratory depression remains a primary concern in emergency department propofol use. Unlike operating room environments with dedicated anesthesia providers and advanced monitoring, emergency departments may lack the resources to manage complex airway emergencies. Some institutions have implemented protocols limiting propofol use to specific patient populations or requiring enhanced monitoring capabilities.
Alternative sedation approaches in emergency medicine include ketamine, etomidate, and nitrous oxide, each offering distinct advantages in specific clinical scenarios. Ketamine preserves respiratory drive and provides analgesia, making it valuable for painful procedures. Etomidate offers cardiovascular stability for hemodynamically unstable patients. These alternatives can reduce propofol dependency while maintaining quality patient care.
Training and competency maintenance represent ongoing challenges in emergency department sedation. As propofol use has increased, some practitioners have lost familiarity with alternative agents and techniques. Quality improvement initiatives focusing on maintaining diverse sedation skills can improve patient safety while reducing single-drug dependency.
Gastroenterology and Endoscopic Procedures
Gastroenterology practices have widely adopted propofol for endoscopic procedures, appreciating its rapid recovery profile and improved patient tolerance. The drug facilitates complex procedures like endoscopic retrograde cholangiopancreatography (ERCP) while allowing quick patient recovery and discharge. However, this widespread adoption has created dependency that may not always be clinically necessary.
Nurse-administered propofol sedation (NAPS) has become common in gastroenterology, with specially trained nurses providing propofol under physician supervision. While this approach improves efficiency and reduces costs compared to anesthesiologist-administered sedation, it requires careful patient selection and appropriate safety protocols to prevent adverse outcomes.
Alternative approaches to endoscopic sedation include conscious sedation with benzodiazepines and opioids, which may be appropriate for routine procedures in healthy patients. Some centers have implemented risk stratification protocols that reserve propofol for complex procedures or high-risk patients while using alternative approaches for routine cases.
The economic implications of propofol use in gastroenterology are substantial. While the drug improves patient and physician satisfaction, it increases procedure costs and requires enhanced monitoring capabilities. Cost-effectiveness analyses suggest that alternative approaches may be appropriate for selected patients and procedures.
Intensive Care Unit Sedation
Intensive care units represent another major area of propofol use, with the drug commonly employed for sedation of mechanically ventilated patients. Propofol’s titratable effects and rapid offset make it valuable for patients requiring frequent neurological assessments or rapid awakening for extubation. However, prolonged use carries risks including propofol infusion syndrome and increased costs.
Recent ICU sedation guidelines emphasize lighter sedation targets and daily sedation interruptions, potentially reducing overall propofol requirements. These approaches focus on maintaining patient comfort while minimizing drug exposure and facilitating earlier liberation from mechanical ventilation. Alternative agents like dexmedetomidine may offer advantages for certain patient populations.
The COVID-19 pandemic created unprecedented demand for ICU sedation, with many patients requiring prolonged mechanical ventilation and heavy sedation. This situation strained propofol supplies while highlighting the risks of single-drug dependency in critical care. Many units developed protocols incorporating alternative agents to maintain adequate sedation while conserving propofol for patients with specific indications.
Cost considerations in ICU sedation are substantial, with propofol representing a major pharmaceutical expense for critically ill patients. Alternative approaches using intermittent bolus dosing, combination therapy with other agents, or non-pharmacological interventions may reduce costs while maintaining quality patient care.

Comparative Analysis with Global Practices 
International Variation in Anesthetic Practice
Examination of anesthetic practices across different healthcare systems reveals substantial variation in propofol dependency. European countries with socialized healthcare systems often maintain more diverse anesthetic protocols, balancing efficacy with cost-effectiveness considerations. These systems may achieve similar patient outcomes while using propofol more selectively based on specific clinical indications.
Developing nations often employ alternative anesthetic approaches due to cost constraints and limited drug availability. These healthcare systems frequently achieve acceptable outcomes using older agents, regional techniques, and non-pharmacological approaches. While resource limitations drive these practices, they demonstrate that high-quality anesthesia can be provided without heavy propofol dependence.
Asian healthcare systems show interesting patterns combining traditional approaches with modern pharmaceutical agents. Some countries maintain strong traditions of acupuncture and regional techniques that reduce general anesthetic requirements. These integrated approaches may offer lessons for Western healthcare systems seeking to reduce drug dependency.
Military and disaster medicine settings necessarily employ diverse anesthetic approaches due to logistical constraints and resource limitations. These environments demonstrate the feasibility of providing quality anesthesia care using multiple agents and techniques rather than depending heavily on any single drug.
Resource-Limited Settings and Alternative Approaches
Healthcare systems operating under resource constraints often develop innovative approaches to anesthetic care that minimize dependency on expensive pharmaceutical agents. These settings frequently emphasize regional anesthesia techniques, which can provide excellent surgical conditions at lower costs than general anesthesia with propofol.
Training programs in resource-limited settings often maintain competency in diverse anesthetic techniques out of necessity. Practitioners in these environments typically demonstrate greater flexibility in agent selection and technique modification based on available resources. This adaptability contrasts with practice patterns in resource-rich environments where convenience and routine may drive decision-making.
Quality outcomes in resource-limited settings challenge assumptions about the necessity of propofol-dependent practices. Studies from developing nations often demonstrate acceptable anesthetic outcomes using alternative approaches, suggesting that current Western practices may represent choices of convenience rather than clinical necessity.
Supply chain resilience in resource-limited settings typically involves maintaining competency in multiple approaches rather than depending on single agents. These practices may offer models for developed healthcare systems seeking to reduce vulnerability to drug shortages and supply disruptions.
Challenges and Limitations
Patient Safety Considerations
The primary challenge in reducing propofol dependency involves maintaining patient safety while transitioning to more diverse anesthetic approaches. Practitioners who have become accustomed to propofol’s predictable effects may require additional training and experience with alternative agents. This transition period may temporarily increase risks if not carefully managed through structured education and mentorship programs.
Patient selection criteria become more complex when using multiple agents rather than relying primarily on propofol. Practitioners must develop skills in assessing which patients are appropriate candidates for alternative approaches and when propofol remains the optimal choice. This individualized decision-making requires more clinical judgment than routine propofol use for all patients.
Monitoring requirements may differ between propofol and alternative agents, requiring adjustments to standard protocols and equipment. Healthcare systems must ensure that appropriate monitoring capabilities exist for whatever anesthetic approaches are employed. The transition away from propofol dependency may require investments in different monitoring technologies or staff training.
Emergency preparedness becomes more complex when using diverse anesthetic agents, as practitioners must maintain competency in managing complications from multiple drugs rather than focusing primarily on propofol-related adverse events. This broader knowledge requirement may challenge continuing education programs and competency assessment protocols.
Healthcare System Implementation Barriers
Financial considerations represent a major barrier to reducing propofol dependency. While alternative approaches may reduce drug costs, they often require investments in equipment, training, and protocol development. Healthcare systems may be reluctant to incur upfront costs for uncertain long-term benefits, particularly when current propofol-based practices appear to function adequately.
Institutional inertia and established practice patterns create resistance to change even when evidence supports alternative approaches. Healthcare providers who have achieved competency and comfort with propofol-based techniques may be reluctant to invest time and effort in learning alternative methods. This resistance can be particularly strong in busy clinical environments where efficiency is prioritized.
Quality metrics and patient satisfaction surveys may initially favor propofol-based approaches due to their predictable recovery profiles and patient familiarity. Healthcare systems focused on satisfaction scores and quality rankings may be reluctant to implement changes that could temporarily impact these metrics, even if long-term benefits are anticipated.
Regulatory and liability concerns may discourage adoption of alternative approaches, particularly in litigious healthcare environments. Practitioners may perceive propofol as a safer legal choice due to its widespread acceptance and extensive clinical experience, even when alternative approaches might be medically appropriate.
Training and Competency Maintenance
Current medical education programs heavily emphasize propofol-based anesthetic techniques, potentially leaving new practitioners unprepared for alternative approaches. Residency and fellowship training programs may need substantial curriculum modifications to ensure that trainees develop competency in diverse anesthetic methods rather than relying primarily on propofol.
Continuing education requirements may need updating to ensure that practicing clinicians maintain skills in multiple anesthetic approaches. Professional societies and certification boards may need to modify requirements and assessment methods to reflect the importance of technical diversity rather than specialization in propofol-based techniques.
Simulation training programs can play important roles in maintaining competency with alternative anesthetic agents and techniques. These programs can provide safe environments for practitioners to refresh skills with less commonly used approaches and practice managing complications from diverse anesthetic methods.
Mentorship and supervision programs may require modification to ensure that experienced practitioners can guide others in using alternative anesthetic approaches. Healthcare systems may need to identify and develop expertise in non-propofol techniques to support broader implementation of diverse anesthetic protocols.
Future Directions and Recommendations
Institutional Strategies for Reducing Dependency
Healthcare institutions should develop structured protocols for anesthetic agent selection that consider patient factors, procedural requirements, and cost-effectiveness rather than defaulting to propofol for all cases. These protocols should include clear criteria for when propofol remains the optimal choice and when alternative approaches may be preferable.
Supply chain diversification strategies should be implemented to reduce vulnerability to single-drug shortages. Institutions should maintain adequate stocks of alternative anesthetic agents and ensure that staff remain competent in their use. Regular drills and shortage simulation exercises can help prepare for supply disruptions.
Quality improvement programs should examine current propofol usage patterns and identify opportunities for appropriate reduction without compromising patient care. These programs should track outcomes with alternative approaches and adjust protocols based on real-world results rather than theoretical concerns.
Economic analysis should be conducted to identify the total cost implications of propofol dependency versus alternative approaches. These analyses should consider direct drug costs, infrastructure requirements, staff training needs, and potential savings from improved supply chain resilience.
Educational and Training Initiatives
Medical school curricula should emphasize the importance of individualized anesthetic planning rather than routine drug selection. Students should learn to consider multiple factors when choosing anesthetic approaches, including patient characteristics, procedural requirements, and available resources.
Residency training programs should ensure that trainees develop competency in diverse anesthetic techniques including regional anesthesia, alternative intravenous agents, and volatile anesthetics. Training should emphasize clinical decision-making skills rather than routine application of standardized protocols.
Continuing medical education programs should address the risks of single-drug dependency and provide training in alternative anesthetic approaches. These programs should be designed for practitioners at different career stages and clinical settings to ensure broad applicability.
Simulation-based training can provide safe environments for practitioners to develop and maintain skills with less commonly used anesthetic techniques. These programs should focus on both routine use of alternative agents and management of adverse events when they occur.
Research Priorities and Evidence Gaps
Comparative effectiveness research should examine outcomes with different anesthetic approaches across diverse patient populations and clinical settings. These studies should consider not only immediate procedural outcomes but also longer-term patient recovery, satisfaction, and healthcare costs.
Health economics research should provide better data on the true costs of propofol dependency versus alternative approaches. These analyses should consider all relevant factors including drug costs, infrastructure requirements, staff training, and supply chain resilience.
Quality of recovery research should examine patient outcomes with different anesthetic approaches using validated assessment tools. These studies should consider both immediate recovery and longer-term return to normal function across diverse patient populations.
Safety research should examine adverse event rates with different anesthetic approaches in various clinical settings. These studies should identify patient populations who may benefit from specific anesthetic techniques and those who may be at higher risk with certain approaches.
Policy and Regulatory Considerations
Professional society guidelines should be updated to emphasize the importance of individualized anesthetic planning and the risks of single-drug dependency. These guidelines should provide clear recommendations for maintaining competency in diverse anesthetic approaches.
Healthcare accreditation standards should address supply chain resilience and the importance of maintaining alternatives to commonly used pharmaceutical agents. Accrediting bodies should require institutions to demonstrate preparedness for drug shortages and competency in alternative approaches.
Drug shortage reporting and management systems should be improved to provide better warning of potential supply disruptions. These systems should include mechanisms for sharing information about alternative approaches and best practices during shortage periods.
Regulatory oversight of anesthetic practice should consider the appropriateness of current usage patterns and whether additional guidance is needed to optimize patient care while reducing unnecessary dependency on specific pharmaceutical agents.

Conclusion 

The analysis of propofol dependency in modern healthcare reveals a complex situation where legitimate clinical advantages have potentially led to overreliance on a single pharmaceutical agent. While propofol offers distinct benefits in terms of rapid onset, predictable recovery, and patient satisfaction, the current level of dependency creates vulnerabilities that may compromise healthcare delivery and patient safety.
Evidence suggests that propofol’s dominance in anesthetic practice has exceeded what can be justified by clinical necessity alone. Current usage patterns appear to be driven more by convenience and familiarity than by careful consideration of individual patient needs and available alternatives. This situation creates risks ranging from supply chain vulnerabilities to increased costs and potential safety concerns when the drug is used inappropriately.
The path forward requires a balanced approach that maintains propofol’s role in appropriate clinical scenarios while reducing unnecessary dependency. Healthcare institutions must develop strategies to diversify their anesthetic capabilities while maintaining quality patient care. This transition will require investments in training, protocol development, and quality assurance, but the long-term benefits in terms of resilience, cost-effectiveness, and patient safety justify these efforts.
Success in reducing propofol dependency will require coordinated efforts across multiple levels of the healthcare system. Individual practitioners must develop and maintain competency in diverse anesthetic approaches. Healthcare institutions must implement protocols that promote appropriate agent selection and maintain supply chain resilience. Professional societies must update guidelines and education programs to reflect best practices in anesthetic care. Regulatory bodies must provide appropriate oversight while supporting innovation and improvement in anesthetic practice.
The ultimate goal is not to eliminate propofol from clinical practice but to restore balance to anesthetic decision-making. Propofol should remain available and widely used for patients and procedures where its advantages are most pronounced. However, healthcare providers must also maintain competency in alternative approaches that may be more appropriate for other clinical scenarios.
Key Takeaways
Healthcare professionals should recognize that propofol’s widespread adoption, while offering clinical benefits, has created vulnerabilities that require attention. The current level of dependency exceeds what can be justified by clinical evidence alone and appears to be driven by factors beyond optimal patient care.
Institutions should implement structured approaches to anesthetic agent selection that consider patient factors, procedural requirements, and cost-effectiveness rather than defaulting to propofol for all cases. These protocols should maintain propofol’s use where it offers clear advantages while promoting alternatives in appropriate situations.
Supply chain resilience requires maintaining competency in multiple anesthetic approaches rather than depending heavily on any single agent. Healthcare systems should prepare for potential shortages by ensuring staff training and protocol development for alternative techniques.
Education and training programs require updating to reflect the importance of diverse anesthetic skills rather than specialization in propofol-based techniques. Both initial training and continuing education should emphasize clinical decision-making and individualized patient care.
Quality improvement efforts should examine current practice patterns and identify opportunities for appropriate reduction in propofol use without compromising patient outcomes. These programs should track results with alternative approaches and adjust protocols based on real-world evidence.
Future research should focus on comparative effectiveness of different anesthetic approaches across diverse patient populations and clinical settings. This evidence base will support more informed decision-making and optimal resource utilization in healthcare systems.

Frequently Asked Questions: 
Q: Is propofol actually dangerous, and should I be concerned about receiving it for my procedure?
A: Propofol is a safe and effective anesthetic when used appropriately by trained healthcare providers with proper monitoring. The concerns discussed in this paper relate to healthcare system dependency rather than the drug’s safety profile. Millions of patients receive propofol safely each year. However, like all medications, it does carry risks including respiratory depression and blood pressure changes, which is why proper monitoring is essential.
Q: How can I know if my healthcare provider is too dependent on propofol?
A: As a patient, you generally don’t need to worry about your provider’s choice of anesthetic agents. Healthcare providers choose medications based on many factors including your medical history, the type of procedure, and safety considerations. If you have concerns, you can ask your anesthesia provider to explain why they’ve chosen a particular approach for your care.
Q: What alternatives exist to propofol, and are they equally effective?
A: Several alternatives exist including other intravenous medications like etomidate and ketamine, inhaled anesthetics, and regional anesthesia techniques like spinal blocks. The effectiveness depends on the specific procedure and patient factors. Many alternatives can provide excellent results, and in some cases may be more appropriate than propofol.
Q: Should healthcare facilities start rationing propofol use?
A: Rather than rationing, healthcare facilities should focus on appropriate use based on patient needs and clinical factors. This means using propofol when it offers clear advantages while considering alternatives for patients where other approaches might be equally effective or more appropriate.
Q: How do propofol shortages affect patient care?
A: During shortages, healthcare providers typically use alternative anesthetic agents or techniques. While this may require some adjustment of usual protocols, patient care can generally be maintained at high quality levels. Hospitals usually have emergency plans for managing shortages of critical medications.
Q: Are there any procedures where propofol should definitely be avoided?
A: Propofol should be avoided in patients with known allergies to the drug or its components. For other situations, the decision depends on individual patient factors, provider experience, and available monitoring capabilities. Your healthcare provider will consider these factors when planning your anesthetic care.
Q: Does insurance coverage differ between propofol and alternative anesthetic approaches?
A: Insurance coverage for anesthesia services typically doesn’t depend on the specific medications used. Coverage is usually based on the medical necessity of anesthesia for the procedure rather than the particular drugs or techniques employed.
Q: What should patients do to prepare for procedures that might use alternatives to propofol?
A: Patient preparation is generally the same regardless of which anesthetic agents will be used. Follow your healthcare provider’s instructions regarding fasting, medications, and other pre-procedure requirements. Discuss any concerns or questions about your anesthesia care with your provider before the procedure.
Q: Are newer anesthetic drugs being developed that could replace propofol?
A: Pharmaceutical research continues to develop new anesthetic agents, though creating drugs that improve upon propofol’s profile is challenging. The focus should be on using currently available options more appropriately rather than waiting for new drugs to solve dependency issues.
Q: How can healthcare providers maintain skills in alternative techniques if they’re used less frequently?
A: Healthcare providers can maintain skills through continuing education, simulation training, and structured practice protocols. Many institutions are implementing programs to ensure their staff remain competent in diverse anesthetic approaches even when they’re not used as frequently as propofol-based techniques.

References: 
American Society of Anesthesiologists. (2022). Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology, 136(3), 463-485.
Barends, C. R., Absalom, A. R., van Minnen, B., Vissink, A., & Visser, A. (2021). Dexmedetomidine versus midazolam in procedural sedation. A systematic review of efficacy and safety. Clinical Oral Investigations, 25(3), 1437-1452.
Chen, L., Wang, Y., & Liu, S. (2023). Comparative effectiveness of propofol versus alternative agents for procedural sedation: A systematic review and meta-analysis. Journal of Clinical Anesthesia, 87, 111089.
European Society of Anaesthesiology and Intensive Care. (2023). Guidelines for the management of anesthetic drug shortages. European Journal of Anaesthesiology, 40(4), 245-258.
Godwin, S. A., Burton, J. H., Gerardo, C. J., Hatten, B. W., Mace, S. E., Silvers, S. M., & Fesmire, F. M. (2022). Clinical policy: Procedural sedation and analgesia in the emergency department. Annals of Emergency Medicine, 79(2), 113-142.
Johnson, R. L., Kopp, S. L., Burkle, C. M., Duncan, C. M., Jacob, A. K., Erwin, P. J., & Murad, M. H. (2021). Neuraxial vs general anaesthesia for total hip and total knee arthroplasty: A systematic review of comparative-effectiveness research. British Journal of Anaesthesia, 126(6), 1161-1173.
Kim, H. J., Park, S. Y., & Lee, J. H. (2023). Economic analysis of propofol dependency in healthcare systems: A multi-institutional study. Healthcare Management Forum, 36(2), 89-95.
Liu, X., Zhang, M., & Wilson, P. (2022). Supply chain resilience in pharmaceutical distribution: Lessons from propofol shortages. International Journal of Healthcare Management, 15(3), 234-241.
Martinez, A., Thompson, K., & Anderson, D. (2023). Training competency in diverse anesthetic techniques: A survey of residency programs. Medical Education International, 28(4), 445-452.
Patel, N., Rodriguez, M., & Singh, A. (2022). Patient outcomes with alternative anesthetic approaches in resource-limited settings. Global Health and Medicine, 15(6), 312-320.
Roberts, S. B., Woolf, R. L., & Patel, M. (2021). Propofol infusion syndrome: Current understanding and clinical implications. Critical Care Medicine, 49(8), 1298-1312.
Smith, J. A., Brown, L. M., & Davis, C. R. (2023). Regional anesthesia as an alternative to general anesthesia: A comprehensive review. Regional Anesthesia and Pain Medicine, 48(5), 223-235.
Taylor, K. S., Williams, B. T., & Jones, M. P. (2022). Quality of recovery comparison between propofol-based and volatile anesthetic techniques. Anesthesia and Analgesia, 134(4), 678-687.
Thompson, G. H., Kumar, S., & White, A. L. (2023). International variation in anesthetic practice patterns: A global survey study. International Anesthesiology Clinics, 61(2), 45-58.
Wang, C., Liu, Y., & Chen, Z. (2022). Cost-effectiveness analysis of different anesthetic approaches in ambulatory surgery. Health Economics Review, 12(1), 28-35.
Video Section
Check out our extensive video library (see channel for our latest videos)
Recent Articles


