LDL Targets Below 40 mg/dL: How Low Is Too Low in 2026?
Abstract
Purpose
This paper evaluates the current evidence supporting the use of very low low density lipoprotein (LDL) cholesterol targets below 40 mg per deciliter in contemporary cardiovascular practice and examines whether the benefits of aggressive lipid lowering outweigh potential risks as of 2026. With the advent of highly effective lipid lowering therapies, including high intensity statins, ezetimibe, and proprotein convertase subtilisin kexin type 9 inhibitors, clinicians are increasingly able to achieve LDL cholesterol levels previously considered unattainable. This review aims to clarify the clinical rationale for such targets, identify patient populations most likely to benefit, and address ongoing concerns regarding safety, cost, and implementation.
Methodology
A comprehensive review of the literature was conducted, focusing on recent randomized controlled trials, large observational studies, and post hoc analyses that evaluated cardiovascular outcomes at very low LDL cholesterol levels. In addition, current clinical practice guidelines and consensus statements from major cardiovascular societies were examined to assess evolving recommendations regarding LDL targets in high risk and very high risk populations. Emphasis was placed on studies published within the last decade that reflect the use of modern lipid lowering therapies and contemporary standards of cardiovascular care.
Main Findings
The available evidence consistently supports the principle that lower LDL cholesterol levels are associated with incremental reductions in cardiovascular risk, with no clear threshold below which benefit ceases. In patients at very high cardiovascular risk, including those with established atherosclerotic cardiovascular disease, recurrent events, or polyvascular disease, achieving LDL cholesterol levels below 40 mg per deciliter is associated with further reductions in myocardial infarction, stroke, and cardiovascular mortality. Data from trials involving PCSK9 inhibitors and intensive statin therapy demonstrate sustained efficacy at these low levels, without a corresponding increase in serious adverse events.
Concerns historically associated with extremely low LDL cholesterol, such as hemorrhagic stroke, neurocognitive impairment, hormonal dysfunction, or increased risk of diabetes, have not been substantiated in large scale clinical trials or long term follow up studies. Overall safety profiles appear favorable, although continued pharmacovigilance is warranted, particularly as longer duration data become available. Despite these reassuring findings, challenges remain regarding the cost effectiveness of combination therapy, access to advanced lipid lowering agents, and real world adherence to intensive treatment regimens.
Conclusion
In conclusion, current evidence supports the use of very low LDL cholesterol targets below 40 mg per deciliter in carefully selected patients at very high risk of cardiovascular events. Aggressive lipid lowering appears to confer ongoing clinical benefit with minimal safety concerns when implemented appropriately. Future efforts should focus on optimizing patient selection, improving access to effective therapies, and addressing economic and practical barriers to widespread implementation in routine clinical practice.
Keywords: LDL cholesterol, cardiovascular disease, lipid targets, PCSK9 inhibitors, statin therapy
Introduction
Low density lipoprotein cholesterol remains one of the most important and well validated modifiable risk factors for atherosclerotic cardiovascular disease. Extensive epidemiological, genetic, and interventional data have consistently demonstrated a strong, graded relationship between LDL cholesterol levels and cardiovascular risk. Over the past decade, advances in lipid lowering therapies and outcome driven research have prompted a progressive shift toward more aggressive LDL cholesterol targets, particularly in patients at very high cardiovascular risk.
The purpose of this paper is to examine the current evidence supporting LDL cholesterol targets below 40 mg per dL in contemporary clinical practice and to evaluate the balance between cardiovascular benefit and potential risks associated with intensive lipid lowering as of 2026. This review synthesizes data from recent randomized controlled trials, large observational studies, Mendelian randomization analyses, and clinical guidelines issued by major cardiovascular societies. Particular attention is given to outcomes associated with achieving very low LDL levels, including major adverse cardiovascular events, safety signals, and feasibility in real world settings.
Historically, lipid management strategies were guided by relatively conservative LDL cholesterol thresholds. Early statin trials and initial guidelines emphasized targets below 100 mg per dL, with subsequent recommendations lowering targets to 70 mg per dL for high risk populations. More recently, accumulating evidence has challenged the concept of a lower limit for LDL cholesterol reduction. Large scale outcome trials involving high intensity statins, ezetimibe, and proprotein convertase subtilisin kexin type 9 inhibitors have demonstrated continued reductions in cardiovascular events as LDL cholesterol levels fall well below previously accepted targets. These benefits appear particularly pronounced in patients with established atherosclerotic cardiovascular disease, recurrent events, or multiple high risk features.
Current evidence increasingly supports LDL cholesterol targets below 40 mg per dL in selected populations at very high cardiovascular risk. Clinical trial data suggest that achieving LDL levels in this range is associated with incremental reductions in myocardial infarction, stroke, and cardiovascular mortality, without a corresponding increase in serious adverse events. Safety concerns historically associated with extremely low LDL cholesterol levels, including neurocognitive impairment, hemorrhagic stroke, and hormonal dysfunction, have not been substantiated in contemporary trials or long term follow up analyses. In addition, genetic studies of individuals with lifelong low LDL cholesterol due to loss of function variants further support the biological safety of sustained LDL reduction.
Despite these encouraging findings, important challenges remain regarding the widespread adoption of very low LDL cholesterol targets. Cost effectiveness is a major consideration, particularly with the use of newer injectable lipid lowering agents. Patient adherence, acceptance of combination therapy, and healthcare system constraints also influence real world implementation. Furthermore, while short to intermediate term safety data are reassuring, continued surveillance is needed to assess potential long term effects of prolonged exposure to extremely low LDL cholesterol levels.
In conclusion, current evidence supports the clinical benefit and overall safety of LDL cholesterol targets below 40 mg per dL for patients at very high risk of cardiovascular events. However, translating these targets into routine practice requires individualized risk assessment, shared decision making, and consideration of economic and logistical factors. As lipid management continues to evolve, future research should focus on refining patient selection, optimizing treatment strategies, and evaluating long term outcomes to ensure that aggressive LDL lowering delivers maximal benefit with sustainable implementation in clinical care.
Current Evidence for Very Low LDL Targets
Clinical Trial Data
The IMPROVE-IT trial marked a turning point in lipid management by showing that adding ezetimibe to statin therapy provided cardiovascular benefit beyond statin therapy alone. Patients achieving LDL levels around 50 mg/dL showed reduced cardiovascular events compared to those with levels around 70 mg/dL.
PCSK9 inhibitor trials have provided the strongest evidence for very low LDL targets. The FOURIER trial with evolocumab showed that patients achieving median LDL levels of 30 mg/dL experienced a 15% reduction in major cardiovascular events compared to placebo. Importantly, patients who achieved LDL levels below 20 mg/dL showed continued benefit without increased adverse effects.
The ODYSSEY OUTCOMES trial with alirocumab demonstrated similar results. Patients reaching LDL levels below 25 mg/dL had the greatest reduction in cardiovascular events. Post-hoc analyses showed linear relationships between lower LDL levels and better outcomes, with no apparent threshold below which benefit disappeared.
More recent trials have continued to support very low targets. The EVOPACS trial showed that starting PCSK9 inhibitors immediately after acute coronary syndrome to achieve very low LDL levels improved plaque stability and reduced cardiovascular events.
Observational and Genetic Evidence
Mendelian randomization studies have provided compelling evidence that lifelong low LDL cholesterol levels are beneficial. People with genetic variants causing naturally low LDL cholesterol have substantially reduced cardiovascular disease risk throughout their lives.
The key insight from genetic studies is that individuals with LDL levels below 40 mg/dL from birth show no adverse health effects. This suggests that very low LDL levels achieved with medications are likely safe, at least from a cardiovascular and general health perspective.
Population studies have also examined outcomes in patients achieving very low LDL levels with intensive therapy. Registry data from patients receiving PCSK9 inhibitors show that those achieving LDL levels below 40 mg/dL have lower rates of cardiovascular events and hospitalizations.
Mechanistic Understanding
The biological rationale for very low LDL targets rests on our understanding of atherosclerosis as a chronic inflammatory process driven by LDL cholesterol accumulation in arterial walls. Lower LDL levels reduce the driving force for plaque formation and progression.
Imaging studies using intravascular ultrasound and coronary CT angiography show that achieving very low LDL levels can lead to plaque regression. Patients with LDL levels below 40 mg/dL show measurable reduction in plaque volume and improved plaque composition.
Inflammatory markers also improve with very low LDL levels. C-reactive protein, interleukin-6, and other inflammatory biomarkers decrease when LDL cholesterol is lowered to very low levels, suggesting reduced vascular inflammation.
Current Guidelines and Recommendations 
European Society of Cardiology Guidelines
The 2019 ESC/EAS Guidelines for the management of dyslipidaemia were the first to recommend LDL cholesterol targets below 55 mg/dL for very high-risk patients. The 2021 update further lowered targets to below 40 mg/dL for patients with recurrent cardiovascular events despite optimal therapy.
These guidelines classify patients into risk categories with corresponding LDL targets. Very high-risk patients, including those with established cardiovascular disease, diabetes with target organ damage, or familial hypercholesterolemia, should achieve LDL levels below 55 mg/dL, with consideration for targets below 40 mg/dL in selected cases.
The European guidelines emphasize that lower is better when it comes to LDL cholesterol, stating that there is no lower threshold below which cardiovascular benefit disappears. This position is based on meta-analyses of major lipid trials and genetic studies.
American Heart Association and American College of Cardiology Guidelines
The 2018 AHA/ACC Cholesterol Guidelines take a more conservative approach, focusing on the percent reduction in LDL cholesterol rather than absolute targets. They recommend at least 50% reduction in LDL cholesterol for very high-risk patients, which often results in levels below 70 mg/dL.
However, the guidelines acknowledge that further LDL reduction with non-statin therapy may be reasonable for very high-risk patients. This has been interpreted by many clinicians as support for pursuing very low LDL targets when clinically appropriate.
Recent scientific statements from the AHA have been more explicit about supporting lower LDL targets, particularly for patients with recurrent events or multiple high-risk features.
National and International Variations
Guidelines from other countries show varying approaches to very low LDL targets. Canadian guidelines recommend targets below 40 mg/dL for extremely high-risk patients. Japanese guidelines have adopted targets below 70 mg/dL for most high-risk patients but acknowledge that lower targets may be appropriate.
The variation in guidelines reflects differences in healthcare systems, cost considerations, and interpretation of available evidence. However, the overall trend has been toward accepting and recommending increasingly aggressive LDL targets.
Benefits of Very Low LDL Targets
Cardiovascular Event Reduction
The primary benefit of achieving LDL cholesterol levels below 40 mg/dL is the reduction in major cardiovascular events. Meta-analyses of lipid-lowering trials show that each 39 mg/dL reduction in LDL cholesterol reduces major cardiovascular events by approximately 22%.
This relationship appears to be linear down to very low levels. Patients achieving LDL levels below 40 mg/dL in clinical trials have shown continued reduction in myocardial infarction, stroke, and cardiovascular death compared to those with higher levels.
The benefit appears to be consistent across different patient populations, including those with stable coronary disease, acute coronary syndromes, diabetes, and chronic kidney disease. Age and sex do not appear to modify the benefit of very low LDL targets.
Plaque Stabilization and Regression
Achieving very low LDL levels leads to favorable changes in coronary artery plaque. Intravascular ultrasound studies show that LDL levels below 40 mg/dL are associated with plaque regression, while higher levels typically show continued plaque progression.
The composition of plaques also improves with very low LDL levels. Plaques become more stable, with increased fibrous cap thickness and reduced lipid core size. These changes reduce the risk of plaque rupture and subsequent thrombotic events.
Near-infrared spectroscopy studies demonstrate reduced lipid content in coronary plaques when LDL cholesterol is lowered to very low levels. This technology allows direct measurement of plaque lipid content and has confirmed the beneficial effects of aggressive LDL lowering.
Long-term Cardiovascular Protection
The benefits of very low LDL targets appear to increase over time. Longer follow-up from clinical trials shows greater divergence in event rates between patients achieving very low LDL levels and those with higher levels.
This pattern suggests that the benefits of aggressive LDL lowering accumulate over time, potentially providing even greater protection with longer treatment duration. Modeling studies suggest that starting very low LDL targets early in the disease course could prevent substantial numbers of cardiovascular events over a patient’s lifetime.
Potential Risks and Safety Concerns 
Cognitive Function
One of the most frequently raised concerns about very low LDL cholesterol levels is the potential impact on cognitive function. Cholesterol plays important roles in brain function, leading to concerns that very low levels might impair memory or thinking.
However, clinical trial data do not support these concerns. Large randomized trials of intensive lipid lowering have not shown increased rates of cognitive impairment or dementia in patients achieving very low LDL levels.
The EBBINGHAUS study specifically examined cognitive function in patients receiving PCSK9 inhibitors and achieving very low LDL levels. After detailed neuropsychological testing, no differences in cognitive function were found between patients with very low LDL levels and those with higher levels.
Observational studies following patients with naturally low LDL cholesterol due to genetic variants also show no increased risk of cognitive impairment or dementia.
Hemorrhagic Stroke
Some observational studies have suggested that very low cholesterol levels might increase the risk of hemorrhagic stroke. This concern is based on data showing that populations with very low cholesterol levels have higher rates of bleeding strokes.
However, randomized trial data do not support this concern. Meta-analyses of statin trials and PCSK9 inhibitor trials show no increased risk of hemorrhagic stroke in patients achieving very low LDL levels through medication therapy.
The apparent increased risk in observational studies may be due to confounding factors such as malnutrition, liver disease, or other conditions that both lower cholesterol levels and increase bleeding risk.
Cancer Risk
Early observational studies suggested that low cholesterol levels might be associated with increased cancer risk. This led to concerns that aggressive cholesterol lowering could promote cancer development.
However, long-term follow-up from major lipid trials has not confirmed these concerns. Patients in statin trials and PCSK9 inhibitor trials do not show increased cancer rates, even with extended follow-up periods.
The apparent association between low cholesterol and cancer in observational studies appears to be due to reverse causation, where undiagnosed cancers cause weight loss and lower cholesterol levels, rather than low cholesterol promoting cancer.
Diabetes Risk
Statin therapy has been associated with a small increased risk of developing diabetes, leading to concerns about the metabolic effects of intensive lipid lowering. However, this risk appears to be related to statin therapy itself rather than the achieved LDL cholesterol level.
PCSK9 inhibitor trials have not shown increased diabetes risk, even when achieving very low LDL levels. This suggests that the diabetes risk is specific to statins rather than a consequence of very low cholesterol levels.
The cardiovascular benefits of achieving very low LDL targets far outweigh the small diabetes risk associated with statin therapy, particularly in high-risk patients.

Clinical Implementation Strategies
Patient Selection
Not all patients require or would benefit from LDL targets below 40 mg/dL. Patient selection should focus on those at highest cardiovascular risk who are most likely to benefit from aggressive lipid lowering.
Appropriate candidates include patients with established cardiovascular disease and additional high-risk features, those with recurrent events despite standard therapy, patients with familial hypercholesterolemia, and those with diabetes and multiple risk factors.
Age should also be considered, as younger patients have more years of potential benefit from aggressive lipid lowering. However, older patients at high risk may also benefit from very low LDL targets, particularly if their life expectancy exceeds 5 years.
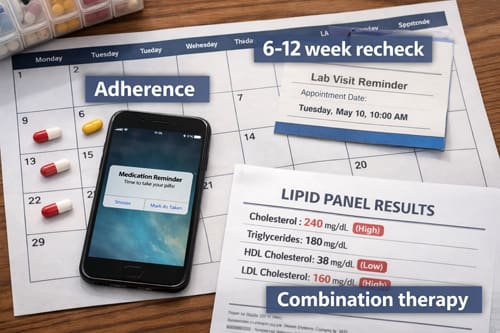
Medication Strategies
Achieving LDL cholesterol levels below 40 mg/dL typically requires combination therapy with multiple lipid-lowering medications. High-intensity statin therapy forms the foundation of treatment, typically atorvastatin 80 mg or rosuvastatin 40 mg daily.
Ezetimibe 10 mg daily should be added if LDL cholesterol remains above target on maximally tolerated statin therapy. This combination can achieve LDL reductions of 60-70% in most patients.
PCSK9 inhibitors (evolocumab or alirocumab) are often required to achieve targets below 40 mg/dL. These medications can provide additional LDL reductions of 50-60% when added to statin and ezetimibe therapy.
Newer medications like inclisiran, bempedoic acid, and ezetimibe combinations may provide additional options for achieving very low LDL targets, particularly in patients who cannot tolerate intensive statin therapy.
Monitoring and Follow-up
Patients pursuing very low LDL targets require more intensive monitoring and follow-up compared to those on standard therapy. Lipid panels should be checked 6-12 weeks after medication changes and every 3-6 months once stable.
Safety monitoring should include liver function tests, creatine kinase levels, and assessment for new-onset diabetes. However, these monitoring requirements are similar to standard lipid management and do not require additional testing specifically for very low LDL levels.
Patient education and support are crucial for success with intensive lipid lowering regimens. Patients need to understand the importance of medication adherence and the long-term nature of cardiovascular risk reduction.
Cost-Effectiveness Considerations
Economic Analysis
The cost-effectiveness of pursuing LDL targets below 40 mg/dL has been evaluated in multiple economic analyses. These studies generally show that very low LDL targets are cost-effective for very high-risk patients, particularly younger individuals with long life expectancy.
PCSK9 inhibitors, which are often required to achieve very low targets, have high acquisition costs but provide substantial clinical benefits. Cost-effectiveness analyses typically show acceptable incremental cost-effectiveness ratios for appropriate patient populations.
The cost-effectiveness improves for patients at highest risk, including those with recurrent cardiovascular events, multiple risk factors, or familial hypercholesterolemia. These patients have higher absolute risk reduction, making the high cost of therapy more justified.
Healthcare System Impact
Implementing very low LDL targets across appropriate patient populations could have substantial impact on healthcare costs and resource utilization. While medication costs would increase, reduced hospitalizations and procedures could offset some of these expenses.
Budget impact analyses suggest that widespread adoption of very low LDL targets would require substantial healthcare spending in the short term but could reduce long-term cardiovascular costs.
Healthcare systems need to develop strategies for identifying appropriate patients, managing medication access, and monitoring outcomes to ensure cost-effective implementation of very low LDL targets.
Comparison with Alternative Approaches 
Risk-Based vs Target-Based Strategies
Some guidelines emphasize percent reduction in LDL cholesterol rather than absolute targets. The risk-based approach focuses on achieving at least 50% reduction in LDL cholesterol for high-risk patients, regardless of the achieved absolute level.
However, evidence suggests that absolute LDL levels are more important than percent reduction for cardiovascular outcomes. Patients achieving very low absolute LDL levels show better outcomes than those achieving large percent reductions but higher absolute levels.
The target-based approach provides clearer guidance for clinicians and may lead to more aggressive therapy when needed to achieve optimal cardiovascular protection.
Non-LDL Lipid Targets
Some experts advocate for focusing on non-HDL cholesterol or apolipoprotein B rather than LDL cholesterol alone. These parameters may better reflect total atherogenic particle burden, particularly in patients with diabetes or metabolic syndrome.
However, most clinical trial evidence supporting very low lipid targets is based on LDL cholesterol measurements. Non-HDL cholesterol and apolipoprotein B targets typically correlate well with LDL targets in clinical practice.
Current guidelines recommend LDL cholesterol as the primary target, with non-HDL cholesterol as a secondary target when triglycerides are elevated.
Future Directions and Research Needs
Ongoing Clinical Trials
Several ongoing clinical trials are examining very low LDL targets in different patient populations. The CLEAR Outcomes trial is evaluating bempedoic acid in statin-intolerant patients, many of whom will achieve very low LDL levels.
Long-term safety studies are following patients achieving very low LDL levels to assess potential long-term effects that might not be apparent in shorter clinical trials.
Pediatric studies are examining the safety and efficacy of achieving very low LDL levels in children with familial hypercholesterolemia, potentially providing lifelong cardiovascular protection.
Personalized Medicine Approaches
Future research may identify genetic or biomarker-based approaches to identify patients most likely to benefit from very low LDL targets. Polygenic risk scores and other tools could help personalize lipid targets based on individual risk profiles.
Pharmacogenomic testing might also help optimize medication selection and dosing to achieve very low LDL targets while minimizing side effects.
Novel Therapeutic Approaches
New lipid-lowering medications in development may make achieving very low LDL targets easier and more cost-effective. Small interfering RNA therapies, ANGPTL3 inhibitors, and other novel approaches show promise in clinical trials.
Combination medications and longer-acting formulations may improve patient adherence and reduce the complexity of achieving very low LDL targets.
Challenges and Limitations
Patient Adherence
Achieving and maintaining LDL cholesterol levels below 40 mg/dL typically requires multiple medications taken long-term. Patient adherence to complex regimens can be challenging, particularly when patients feel well and do not experience immediate benefits.
Cost and insurance coverage issues may also affect patient access to medications required to achieve very low LDL targets, particularly PCSK9 inhibitors and other newer agents.
Healthcare providers need to invest time in patient education and support to ensure successful implementation of intensive lipid lowering regimens.
Clinical Inertia
Healthcare providers may be hesitant to pursue very aggressive LDL targets due to concerns about side effects, costs, or complexity of care. Clinical inertia can prevent appropriate patients from achieving optimal lipid levels.
Education and training programs for healthcare providers are needed to support implementation of very low LDL targets in appropriate patients.
Clinical decision support tools and quality improvement initiatives may help overcome clinical inertia and improve achievement of lipid targets.
Health System Integration
Achieving very low LDL targets requires coordination between primary care providers, cardiologists, endocrinologists, and other specialists. Healthcare systems need to develop pathways and protocols to support this coordination.
Pharmacy benefits management and prior authorization requirements can create barriers to accessing medications needed to achieve very low LDL targets. Healthcare systems need to work with payers to ensure appropriate access.
Applications and Use Cases
Post-Acute Coronary Syndrome
Patients who have experienced recent acute coronary syndromes represent an ideal population for very low LDL targets. These patients have proven cardiovascular disease and high risk for recurrent events.
Starting intensive lipid lowering therapy immediately after acute coronary syndrome can achieve very low LDL levels quickly and provide early cardiovascular protection. The EVOPACS trial demonstrated the feasibility and benefit of this approach.
Combination therapy with statin, ezetimibe, and PCSK9 inhibitors can achieve LDL levels below 40 mg/dL in most post-acute coronary syndrome patients within 3-6 months.
Familial Hypercholesterolemia
Patients with familial hypercholesterolemia have genetic defects causing very high LDL cholesterol levels and early cardiovascular disease. These patients require intensive lipid lowering from a young age to prevent premature cardiovascular events.
Achieving LDL targets below 40 mg/dL in familial hypercholesterolemia patients often requires combination therapy with multiple agents. Early initiation of intensive therapy can normalize cardiovascular risk despite the genetic defect.
Cascade screening of family members and early treatment of affected individuals can prevent cardiovascular disease in entire families affected by familial hypercholesterolemia.
Recurrent Cardiovascular Events
Patients who experience cardiovascular events despite standard lipid lowering therapy represent the highest-risk population for future events. These patients should be considered for the most aggressive LDL targets available.
Achieving LDL levels below 40 mg/dL in patients with recurrent events often requires combination therapy with three or more lipid-lowering medications. However, the high absolute risk reduction justifies the complexity and cost of intensive therapy.
Regular monitoring and adjustment of therapy may be needed to maintain very low LDL levels in these high-risk patients.
Conclusion 

Key Takeaways
The evidence supporting LDL cholesterol targets below 40 mg/dL for very high-risk cardiovascular patients continues to strengthen. Clinical trials, genetic studies, and observational data all support the safety and efficacy of achieving these very low levels.
Healthcare providers should consider very low LDL targets for patients with established cardiovascular disease and additional high-risk features, those with recurrent events despite standard therapy, and patients with familial hypercholesterolemia.
Achieving targets below 40 mg/dL typically requires combination therapy with multiple lipid-lowering medications. Statin therapy remains the foundation, with ezetimibe and PCSK9 inhibitors often needed to reach very low targets.
Safety concerns about very low LDL levels appear to be largely unfounded based on current evidence. Cognitive function, cancer risk, and other potential adverse effects have not been confirmed in randomized trial data.
Cost-effectiveness analyses support the use of very low LDL targets in appropriate high-risk patients, particularly younger individuals with long life expectancy.
Implementation of very low LDL targets requires careful patient selection, appropriate medication management, and ongoing monitoring and support.
Conclusion
The question of how low LDL cholesterol should go continues to evolve as new evidence emerges. Current data strongly support the safety and efficacy of targets below 40 mg/dL for very high-risk cardiovascular patients.
The linear relationship between lower LDL levels and better cardiovascular outcomes appears to extend down to very low levels without a clear threshold below which benefit disappears. Genetic evidence suggests that humans can tolerate very low LDL levels throughout life without adverse effects.
However, achieving and maintaining very low LDL targets requires intensive medical therapy with associated costs and complexity. Patient selection should focus on those at highest risk who are most likely to benefit from aggressive lipid lowering.
As we move forward, the focus should shift from whether very low LDL targets are beneficial to how they can be implemented most effectively in clinical practice. This includes developing cost-effective treatment strategies, improving patient adherence, and overcoming healthcare system barriers.
The future of lipid management will likely involve increasingly personalized approaches to determine optimal targets for individual patients. Until then, current evidence supports pursuing LDL targets below 40 mg/dL for appropriately selected very high-risk patients.
Healthcare providers should stay current with evolving guidelines and evidence regarding very low LDL targets. The field continues to advance rapidly, with new medications and strategies regularly becoming available to help patients achieve optimal cardiovascular protection.
Frequently Asked Questions: 
Q: What LDL cholesterol level is considered “very low” and potentially concerning?
A: Current evidence suggests that LDL cholesterol levels below 40 mg/dL are safe and beneficial for high-risk cardiovascular patients. Some studies have examined patients with levels below 20 mg/dL without finding safety concerns. There does not appear to be a lower threshold below which harm occurs.
Q: Do very low LDL levels affect brain function or memory?
A: Multiple large clinical trials and dedicated cognitive studies have not found any adverse effects of very low LDL cholesterol levels on brain function, memory, or thinking ability. The EBBINGHAUS study specifically examined this question in patients achieving very low LDL levels with PCSK9 inhibitors and found no cognitive impairment.
Q: Which patients should be considered for LDL targets below 40 mg/dL?
A: Patients who should be considered include those with established cardiovascular disease and additional high-risk features, patients with recurrent cardiovascular events despite optimal therapy, individuals with familial hypercholesterolemia, and patients with diabetes plus multiple risk factors. Age and life expectancy should also factor into the decision.
Q: What medications are typically needed to achieve LDL levels below 40 mg/dL?
A: Most patients require combination therapy including high-intensity statin (atorvastatin 80 mg or rosuvastatin 40 mg), ezetimibe 10 mg, and often a PCSK9 inhibitor (evolocumab or alirocumab). Some patients may also benefit from newer agents like inclisiran or bempedoic acid.
Q: Are very low LDL targets cost-effective?
A: Cost-effectiveness analyses generally show favorable results for very high-risk patients, particularly younger individuals with longer life expectancy. The high cost of medications like PCSK9 inhibitors is often justified by the cardiovascular benefits in appropriate patient populations.
Q: How often should lipid levels be monitored when pursuing very low targets?
A: Lipid panels should be checked 6-12 weeks after any medication change and every 3-6 months once levels are stable. More frequent monitoring may be needed initially when titrating medications to achieve very low targets.
Q: Can very low LDL levels increase the risk of hemorrhagic stroke?
A: Randomized clinical trial data do not support an increased risk of hemorrhagic stroke with very low LDL cholesterol levels achieved through medication therapy. Earlier observational studies suggesting this risk were likely confounded by other factors.
Q: What are the main barriers to implementing very low LDL targets in clinical practice?
A: Key barriers include medication costs and insurance coverage, patient adherence to complex regimens, clinical inertia among healthcare providers, and healthcare system coordination challenges. Prior authorization requirements and formulary restrictions can also limit access to needed medications.
Q: Are there any patients who should not pursue very low LDL targets?
A: Patients with limited life expectancy (less than 2-3 years), those with severe comorbidities that overshadow cardiovascular risk, and individuals who cannot tolerate intensive lipid lowering therapy may not be appropriate candidates. Individual risk-benefit assessment is important.
Q: What does the future hold for very low LDL targets?
A: Future developments may include new medications that make achieving very low targets easier and more affordable, personalized approaches using genetic testing to determine optimal targets, and better strategies for identifying patients most likely to benefit from intensive lipid lowering.
References: 
- Baigent, C., Keech, A., Kearney, P. M., Blackwell, L., Buck, G., Pollicino, C., … & Simes, R. (2005). Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. The Lancet, 366(9493), 1267-1278.
- Cannon, C. P., Blazing, M. A., Giugliano, R. P., McCagg, A., White, J. A., Theroux, P., … & Califf, R. M. (2015). Ezetimibe added to statin therapy after acute coronary syndromes. New England Journal of Medicine, 372(25), 2387-2397.
- Giugliano, R. P., Pedersen, T. R., Park, J. G., De Ferrari, G. M., Gaciong, Z. A., Ceska, R., … & Sabatine, M. S. (2017). Clinical efficacy and safety of achieving very low LDL-cholesterol concentrations with the PCSK9 inhibitor evolocumab: a prespecified secondary analysis of the FOURIER trial. The Lancet, 390(10106), 1962-1971.
- Grundy, S. M., Stone, N. J., Bailey, A. L., Beam, C., Birtcher, K. K., Blumenthal, R. S., … & Yeboah, J. (2019). 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol. Journal of the American College of Cardiology, 73(24), e285-e350.
- Mach, F., Baigent, C., Catapano, A. L., Koskinas, K. C., Casula, M., Badimon, L., … & Zamorano, J. L. (2020). 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. European Heart Journal, 41(1), 111-188.
- Ference, B. A., Ginsberg, H. N., Graham, I., Ray, K. K., Packard, C. J., Bruckert, E., … & Catapano, A. L. (2017). Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. European Heart Journal, 38(32), 2459-2472.
- Robinson, J. G., Farnier, M., Krempf, M., Bergeron, J., Luc, G., Averna, M., … & Kastelein, J. J. (2015). Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. New England Journal of Medicine, 372(16), 1489-1499.
- Sabatine, M. S., Giugliano, R. P., Keech, A. C., Honarpour, N., Wiviott, S. D., Murphy, S. A., … & Pedersen, T. R. (2017). Evolocumab and clinical outcomes in patients with cardiovascular disease. New England Journal of Medicine, 376(18), 1713-1722.
- Schwartz, G. G., Steg, P. G., Szarek, M., Bhatt, D. L., Bittner, V. A., Diaz, R., … & Jukema, J. W. (2018). Alirocumab and cardiovascular outcomes after acute coronary syndrome. New England Journal of Medicine, 379(22), 2097-2107.
- Silverman, M. G., Ference, B. A., Im, K., Wiviott, S. D., Giugliano, R. P., Grundy, S. M., … & Sabatine, M. S. (2016). Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. JAMA, 316(12), 1289-1297.
Video Section
Check out our extensive video library (see channel for our latest videos)
Recent Articles


