Uterine Transplant Success Rates Breakthrough Data from 2025 Clinical Trials
Introduction
Uterine transplantation has emerged as a transformative therapeutic option for women with uterine factor infertility, a condition that affects approximately five percent of women of reproductive age worldwide. Uterine factor infertility is defined by the absence of a functional uterus and represents one of the few forms of infertility in which pregnancy has historically been impossible despite normal ovarian function. Advances in surgical technique, immunosuppression, and assisted reproductive technologies have positioned uterine transplantation as a viable solution that enables gestation and childbirth in carefully selected patients.
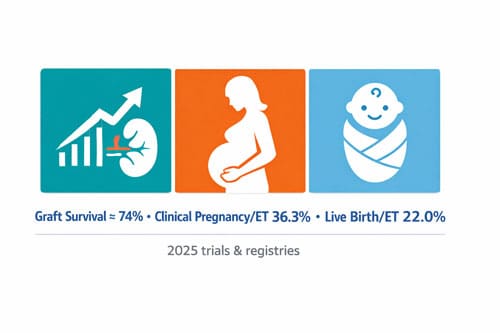
Recent clinical trials and international registry data demonstrate encouraging outcomes that mark a significant milestone in reproductive medicine. Contemporary studies report an overall uterine transplant success rate of approximately 74 percent, with a clinical pregnancy rate of 36.3 percent and a live birth rate per embryo transfer of 22.0 percent. These outcomes represent unprecedented progress in the management of uterine factor infertility and compare favorably with early results from other complex transplant procedures. Notably, outcomes continue to improve as surgical teams gain experience and protocols are refined.
Uterine factor infertility arises from a range of congenital and acquired conditions. Congenital absence or malformation of the uterus accounts for a substantial proportion of cases, with congenital uterine anomalies affecting up to 6.7 percent of the female population. Among these, Mayer Rokitansky Küster Hauser syndrome is the most well recognized etiology, occurring in approximately one in 4,500 to 5,000 women and characterized by uterine agenesis in the presence of normal secondary sexual development and ovarian function. Acquired uterine factor infertility most commonly results from hysterectomy performed for benign or malignant indications. In the United States alone, more than 150,000 hysterectomies are performed annually in women of reproductive age, creating a large population for whom traditional fertility treatments offer no pathway to pregnancy.
For individuals affected by uterine factor infertility, uterine transplantation provides an opportunity for biological motherhood that was previously unattainable. The procedure involves transplantation of a donor uterus, followed by in vitro fertilization and embryo transfer once graft function is established. Over the past decade, uterine transplant protocols have evolved substantially, incorporating advances in donor selection, surgical techniques for vascular anastomosis, perioperative management, and immunosuppressive regimens.
Data from centers with established uterine transplant programs report graft survival rates of approximately 74 percent at one year following transplantation. Among recipients with viable grafts, some programs have achieved live birth rates as high as 83 percent, underscoring the importance of careful patient selection and multidisciplinary expertise. Importantly, reported pregnancies following uterine transplantation have generally resulted in favorable obstetric outcomes. Median gestational ages approach 37 weeks, and available data indicate no increased incidence of congenital malformations among infants born following uterine transplant pregnancies.
This review examines the most recent evidence from clinical trials and observational studies published through 2025, with a detailed analysis of outcomes stratified by donor type, including living and deceased donors. It further explores pregnancy and delivery outcomes, maternal surgical and immunologic complications, neonatal health, and the psychological and quality of life impacts experienced by transplant recipients. As uterine transplantation continues to evolve from experimental innovation toward clinical application, ongoing evaluation of safety, efficacy, and ethical considerations will be essential to define its role in future reproductive care.
Clinical Trial Landscape in 2025: Scope and Methodology
The 2025 landscape of uterine transplant clinical trials reflects a methodical evolution of this experimental procedure into an increasingly standardized treatment. Research protocols now adhere to rigorous scientific frameworks, including the IDEAL criteria for surgical innovation and the Moore Criteria for translational research [1].
Study inclusion criteria and data sources
Recent systematic reviews of uterine transplant outcomes have employed meticulous methodological approaches. One comprehensive analysis registered on the PROSPERO platform (ID: CRD420250604888) followed PRISMA 2020 guidelines to ensure methodological transparency and prevent research bias [1]. This review examined literature from three major databases:
- PubMed (Medline)
- Web of Science
- Scopus
The search parameters covered publications from January 2002 through December 2024, with analyzes focusing on peer-reviewed clinical studies including observational research, retrospective and prospective studies, clinical trials, and cohort studies [1]. Conversely, preclinical or animal studies, isolated case reports, editorials, and opinion pieces were excluded from most analyzes [1].
For recipients, common inclusion criteria across trials encompass:
- Reproductive-aged females (18-45 years) with sufficient embryos
- Absence of hypertension, diabetes, or significant systemic illness
- Body mass index ≤30 kg/m²
- Non-smoker status
- Adequate vaginal canal (minimum 7 cm length) [2]
Donor criteria vary between living and deceased donor protocols, though all donors must be blood-type compatible with recipients [2]. Living donors typically need to be medically healthy, parous, have favorable obstetric histories, and be free of conditions that might impact reproductive outcomes [2].
Geographic distribution of trials: Sweden, US, Czech Republic
The geographical distribution of uterine transplant research reveals concentrated centers of excellence. According to citation analysis, Sweden leads with the highest total citations (TC=4274), followed by the United States (TC=3251), Spain (TC=1972), and England (TC=1741) [3]. However, the most active clinical programs are in:
- Sweden – Pioneer in the field with the first successful trial and births
- United States – Through the United States Uterus Transplant Consortium (USUTC), formed in 2019 by centers at Baylor University Medical Center, Cleveland Clinic, and University of Pennsylvania [4]
- Czech Republic – Among the top ten countries in uterine transplant research (TC=284) [3]
International collaboration has been crucial to advancing the field, with the most substantial collaborative relationships occurring between Sweden and Spain (18 collaborations), Sweden and the USA (14), and the USA and Spain (8) [3]. The International Society of Uterus Transplantation (ISUTx) serves as a vital network for sharing protocols and outcomes [5].
Definition of success: menstruation, pregnancy, live birth
Success in uterine transplant follows a progressive framework. In 2020, the United States Uterus Transplant Consortium established guidelines identifying seven sequential stages of success [4]:
- Technical success (surgical)
- Menstruation
- Embryo implantation
- Pregnancy
- Delivery
- Graft removal
- Long-term follow-up
Menstruation represents the first clinical indication of graft function, requiring regeneration of the endometrium, a patent uterine cavity, and functional outflow tract. The mean time to first menstrual cycle is 30 days (range: 10-59 days) [4]. Nevertheless, a UTx procedure is considered fully successful only when a healthy baby has been delivered from the transplanted uterus [1].
Pregnancy after uterine transplant necessitates assisted reproductive technology since fallopian tubes are not transplanted [4]. The time to first embryo transfer ranges from 64 to 551 days post-transplant [1]. Current data show a clinical pregnancy rate of 36.3% per embryo transfer and a live birth rate of 22.0% per embryo transfer [1].
Primary efficacy outcomes in most trials measure the proportion of recipients achieving at least one live birth [4]. According to recent data, this proportion reaches 83% among recipients with viable grafts—comparable or superior to the estimated cumulative live birth rates for patients under 35 years after six cycles of IVF without uterus transplant (65% to 86%) [4].
Uterine Transplant Success Rates by Donor Type 
Analysis of recent clinical trials reveals distinct patterns in uterine transplant outcomes based on donor source. These findings offer crucial insights for refining surgical techniques and improving success rates in this evolving field.
Living donor vs deceased donor outcomes
Recent data from multiple transplant centers shows that among 33 uterine transplants performed between 2016 and 2021, 64% utilized living donors while 36% came from deceased donors [1]. Initially, researchers debated which source would yield better outcomes, but current evidence suggests both approaches can achieve success with proper patient selection and surgical technique.
Living donor uterine transplant (LD UTx) offers several advantages:
- Complete clinical and radiological assessment of donors
- More accurate recipient evaluation
- Preventable procedure with controlled timing [6]
Deceased donor uterine transplant (DD UTx), meanwhile, eliminates risk to living donors and potentially simplifies procurement techniques [1]. As one transplant center concluded, “outcomes are the same in deceased donor as with living donor uterus transplantation” [1].
Yet systematic reviews present a more nuanced picture, with surgical success rates of 78% for LD UTx versus 64% for DD UTx [2]. Essentially, both approaches remain viable, with centers increasingly developing expertise in their preferred technique rather than abandoning either method.
Graft survival rate: 74% overall
The critical benchmark for technical success in uterine transplant surgery is graft survival, particularly at the one-year mark. Data from U.S. transplant centers demonstrates an overall one-year graft survival rate of 74% (23 of 31 recipients) [1]. Notably, this rate holds relatively steady regardless of donor type, with 74% (14 of 19) survival after living donor transplant and 75% (9 of 12) after deceased donor transplant [1].
The Cleveland Clinic, which performed the first U.S. uterine transplant, reports similar figures with one-year graft survival at 74% [5]. Importantly, among recipients who reach this milestone, 83% subsequently achieve at least one live birth [5]. This clearly indicates that once the critical one-year threshold is passed, prospects for successful pregnancy become considerably favorable.
From a global perspective, 76% of uterine transplants (25 of 33) are technically successful when defined as having a viable graft at postoperative day 30 [1]. Currently, some centers report even higher early graft survival rates of 80% in both living and deceased donor cohorts [2].
Graft failure causes: thrombosis, infection, rejection
Despite advances in surgical technique, approximately one-quarter of uterine transplants experience graft failure. The primary causes remain consistent across transplant centers worldwide.
Vascular complications, particularly thrombosis, represent the leading cause of graft loss [1]. These typically manifest in the immediate postoperative period and necessitate graft hysterectomy [7]. Many recipients with thrombosis develop graft failure within one month of surgery [8]. Overall, vascular complications occur in approximately 20% of cases [7].
Infection poses another significant challenge. Among 33 recipients, 30% experienced infection, with urinary tract infections being most common (12%) [1]. Occasionally, severe infections resistant to treatment necessitate graft removal [9].
Rejection remains a concern, with 43% of recipients experiencing at least one episode of acute cellular rejection (ACR) requiring treatment [1]. The ACR rate varies by donor type—57% among living donors compared to 22% among deceased donors [1]. Fortunately, most rejection episodes respond well to corticosteroid treatment, with all documented cases successfully controlled using intravenous and oral steroid therapy [6].
In examining graft failure patterns globally, data suggests a slightly higher failure rate among deceased donor transplants (28%) compared to living donor procedures (16.9%) [2]. This difference may inform future refinements in surgical techniques and postoperative management.
Pregnancy Outcomes Following Successful UTx
Following graft survival, pregnancy becomes the next crucial milestone in the uterine transplant journey. Data from multiple transplant centers reveals distinct patterns in timing, success rates, and pregnancy outcomes that inform clinical practice.
Time to first embryo transfer: 64–551 days
The interval between transplantation and the first embryo transfer varies considerably across centers and individual cases. The median time from uterus transplant to first embryo transfer is 4.1 months (approximately 123 days), with a range of 2.1-7.7 months [3]. In other studies, the first embryo transfer was performed after a mean of 178 days (range: 106-335 days) [10].
This timeline represents a notable shift from initial protocols:
- Early uterine transplant programs recommended waiting 12 months before embryo transfer
- Current protocols typically aim for 3-6 months post-transplant [11]
- Some centers report successful transfers as early as 64 days post-transplant
The rationale for earlier embryo transfers is straightforward—to minimize the total duration of immunosuppression exposure [11]. Nevertheless, each center must balance this goal against ensuring adequate healing and stable graft function. Regular menstruation, typically beginning around 30 days post-surgery, serves as the primary indicator of graft readiness for embryo transfer [4].
Clinical pregnancy rate (CPR) per ET: 36.3%
Analysis of pooled data from ten major studies—including four from Sweden, three from the DUETS group, two from the Czech Republic, and one multi-institutional American study—established a clinical pregnancy rate (CPR) per embryo transfer of 36.3% [8].
In fact, individual centers occasionally report even higher success rates. For instance, among 23 recipients who underwent a total of 59 embryo transfers, 19 eventually had at least one live-born child [10]. Most recipients who achieved pregnancy did so relatively quickly—89% of those who had a live birth achieved pregnancy after their first or second embryo transfer, whereas only 11% required three or more embryo transfers [12].
Live birth rate (LBR) per ET: 22.0%
The overall live birth rate per embryo transfer across recent studies stands at 22.0% [8]. This figure increases substantially to 43% in some specialized centers with more established protocols [3]. Certain programs report that 50% of recipients experienced a live birth after their first embryo transfer [3].
Obviously, cumulative success rates increase with multiple transfer attempts. The Dallas Uterus Transplant Study (DUETS) found that among recipients with successful grafts, all 14 eventually gave birth to at least one live-born infant [13]. Likewise, other centers report that 83% of recipients with viable grafts ultimately had at least one live birth [12].
These results suggest that a successfully transplanted uterus functions comparably to a native uterus in terms of supporting pregnancy [11]. Indeed, the national U.S. data for infertility treatment in women under 35 using their own ova suggests a live birth rate of 68.9% following any number of cycles—a benchmark that uterine transplant outcomes are approaching [11].
Pregnancy loss and recurrent miscarriage rates
Pregnancy loss remains an important consideration in uterine transplant pregnancies. Among recipients who achieved pregnancy, approximately 19% experienced miscarriage [12]. The majority of these losses (60%) occurred during the first trimester [12].
More complex cases of recurrent pregnancy loss have also been documented:
- Some recipients experienced multiple consecutive losses
- Second-trimester losses occurred at gestational weeks 17-19 [4]
- Cervical insufficiency emerged as a notable cause for second-trimester losses [3]
In one documented case, a recipient experienced two second-trimester miscarriages at 17 and 19 weeks, followed by multiple failed transfers or biochemical pregnancies, before finally achieving a successful live birth with her seventh embryo transfer, nearly four years after transplantation [4]. Indeed, this underscores both the challenges and the ultimate potential for success.
Generally, early pregnancy losses in uterine transplant recipients appear comparable to those in the general population undergoing IVF. Moreover, with appropriate interventions such as cervical cerclage for identified insufficiency, many recipients go on to achieve successful pregnancies in subsequent attempts [4].
Obstetric and Maternal Complications in UTx Pregnancies 
Pregnancies following uterine transplant present unique clinical challenges, requiring specialized monitoring and management. Maternal and obstetrical complications occur in approximately 50% of successful pregnancies after uterine transplant surgery [3], highlighting the complex nature of these gestations.
Preeclampsia and gestational hypertension incidence
Hypertensive disorders represent a primary concern for recipients with transplanted uteri. Gestational hypertension affects 14-24% of uterine transplant pregnancies [3][10], making it the most common maternal complication. Preeclampsia occurs in 7.5-15% of cases [1][6], notably higher than the 3-5% rate observed in the general population but consistent with rates in other solid organ transplant recipients.
Risk factors for preeclampsia in uterine transplant recipients include:
- Calcineurin inhibitor-based immunosuppression
- Abnormal renal function (lower eGFR at embryo transfer)
- Single kidney anatomy (common in MRKH syndrome)
Immunosuppressive medications, particularly tacrolimus, contribute to this elevated risk through their vasoconstrictive properties [14]. Consequently, close monitoring of blood pressure, proteinuria, and renal function becomes essential throughout gestation. Early administration of low-dose aspirin (81 mg daily) serves as standard prophylaxis, initiated during early gestation [5].
Preterm labor and cesarean delivery rates
Premature birth occurs frequently following uterine transplantation. Accordingly, 75% of births following UTx occur before 37 weeks gestation [5], with a median gestational age at delivery of 36 weeks and 1 day [15]. Preterm labor complicates 14% of uterine transplant pregnancies [3], while cervical insufficiency affects another 14% [3].
Unplanned preterm deliveries result from several factors:
- Spontaneous preterm labor
- Severe rejection episodes
- Placental complications (placenta previa occurs in 10% of cases [1])
- Subchorionic hematoma
Although initial protocols recommended delivery at 35 weeks, current guidelines suggest aiming for 37 weeks when possible to reduce neonatal respiratory morbidity [5]. Among elective cesarean sections, 52.4% still occur before 37 weeks [1], often due to maternal complications requiring early delivery.
All deliveries following uterine transplant occur via cesarean section due to concerns about vaginal anastomosis dehiscence and potential damage to surrounding structures [14]. Furthermore, emergency cesarean deliveries account for 47.5% of all deliveries [1], underscoring the unpredictable course of these pregnancies.
Renal toxicity and vaginal stenosis prevalence
Renal function requires careful monitoring throughout the transplant and pregnancy journey. The median serum creatinine in nonpregnant and pregnant recipients reaches 1.0 mg/dL, with ranges of 0.75-1.89 mg/dL and 0.66-1.47 mg/dL respectively [3]. Calcineurin inhibitor-induced kidney toxicity occasionally necessitates early delivery [3].
Grade 1 acute kidney injury (AKI) by AKIN criteria affects 50% of recipients during pregnancy [6]. Thereafter, renal dysfunction contributes substantially to pregnancy complications, including hypertensive disorders and fetal growth restriction [6]. Unlike other solid organ transplants, renal toxicity typically resolves after graft hysterectomy and cessation of immunosuppression [14].
Vaginal stenosis emerges as a remarkably common surgical complication, affecting 66.7-72% of recipients [7][10]. The median time to stenosis development is just 33 days post-transplant [7]. Severity grading correlates with treatment responsiveness – grade 1 stenosis typically responds to self-dilation, whereas all grade 3 cases require surgical repair or dilation under anesthesia [7]. Risk factors include short preoperative vaginal length and history of müllerian agenesis [7].
Neonatal and Infant Outcomes up to 3 Years
Examining children born after uterine transplant provides crucial insights into the long-term viability of this procedure. Throughout 2025, expanded follow-up data has enhanced understanding of outcomes from infancy through early childhood.
Preterm vs full-term birth distribution
Children born from transplanted uteri demonstrate distinctive gestational patterns. Approximately 60.7% of newborns arrive preterm, with the remaining 39.3% reaching full-term gestation [8]. The median gestational age at delivery typically falls between 35 weeks 3 days and 37 weeks, with the earliest recorded birth at 30 weeks 6 days and the latest at 38 weeks 1 day [8]. Recent analysis from 33 uterine transplant births reveals a median delivery time of 36 weeks 4 days [2].
Planned vs unplanned deliveries show meaningful differences:
- Planned term deliveries comprise 44% of live births
- Among preterm births, 30% are planned versus 70% unplanned [9]
The cause for preterm births remains multifactorial, with spontaneous preterm labor, rejection episodes, subchorionic hematomas, and placenta previa contributing to early delivery decisions [9]. Importantly, all deliveries occur via cesarean section [8].
Congenital anomalies and Apgar scores
Most children born after uterine transplant show no major congenital issues. Within studied cohorts, 78.6% exhibit no apparent congenital anomalies [8]. Of the 21.4% with anomalies, cases include patent foramen ovale, clitoromegaly with anterior urethral displacement (surgically corrected at 11 months), and helical ear deformity [8]. In other centers, no congenital malformations were detected among 16 live-born infants [10].
Apgar scores typically indicate healthy neonatal adaptation. The mean scores reach 8 at one minute and 9 at five minutes, with ranges from 4-10 at first minute and 8-10 at fifth minute [8]. In one study, the lowest recorded Apgar score at 5 minutes was 8 [16]. Neonatal complications primarily involve respiratory distress syndrome, neutrophilia, hypoglycemia, and fetal lung fluid retention [8].
Neurodevelopmental milestones at 6, 12, 24, and 36 months
Longitudinal assessment shows predominantly favorable developmental trajectories. At 2 months, 100% of evaluated infants demonstrate normal anthropometric data (weight, height, head circumference) and neurodevelopment [8]. This pattern continues at 6 months with all infants maintaining normal anthropometric parameters [8].
By 12 months, subtle deviations emerge—one child exhibited abnormal anthropometric data, while another showed delayed language development, unable to use “mother” or “father” meaningfully [8]. At 18 months, three of nine evaluated children had anthropometric abnormalities, with three showing mild cognitive deficits, primarily in language [8].
At 24 months, four of five children reached expected milestones, with only one child showing persistent communication delays requiring speech therapy [8]. Concurrent studies affirm these findings, noting physical and neurological milestones were age-appropriate for all children within the first two years [17].
For the longest follow-up to date, by 36 months, 100% of evaluated children achieved expected anthropometric parameters [8]. One case of idiopathic thelarche emerged at 21 months, and one child exhibited mild expressive communication deficits [8]. From a broader dataset, only one child among 33 had been diagnosed with autism at 3-year follow-up [2].

Psychological Impact and Quality of Life in Recipients
Beyond physical outcomes, the psychological dimension of uterine transplant reveals crucial insights into recipients’ lived experiences. Throughout the recovery journey, most recipients maintain resilient mental health despite facing numerous challenges.
SF-36 and HADS scores over 4 years
Five years post-transplantation, the majority of recipients scored above predicted general population values on quality-of-life measures [18]. Physical component summary (PCS) scores remained relatively stable across follow-up periods, with only two recipients showing significant declines [11]. Most recipients maintained mental component summary (MCS) scores above population norms (50) at year five, with decreases observed in only two women [11].
HADS measurements revealed:
- Depression scores consistently remained below clinical thresholds (8) at five-year follow-up [18]
- Only one recipient exhibited anxiety scores requiring further clinical assessment [11]
- Year two evaluations showed temporary decreases in physical components among several recipients [19]
Impact of failed pregnancies on mental health
Failed pregnancy outcomes distinctly influenced psychological wellbeing. A recipient experiencing six miscarriages showed continuous decline in both physical and mental component scores throughout the study period [11]. Primarily, recipients who experienced multiple pregnancy failures demonstrated higher anxiety and depression scores at 4-year follow-up [20].
Childlessness appeared directly linked to elevated anxiety scores [21]. Even with baseline psychological characteristics equal to or better than norm populations, graft failure and unsuccessful pregnancy attempts created substantial psychological strain [19].
Marital adjustment and FertilQol trends
Marital satisfaction assessments revealed a complex picture. Recipients showed declining satisfaction with marital relationships over time, yet maintained scores above the “at risk for divorce” threshold [18]. In the first uterine transplant cohort, two recipients and one living donor divorced during the study period [11].
FertilQol assessments identified the emotional dimension as the most distressing aspect of infertility for recipients [22]. Interestingly, couples undergoing uterine transplant showed better infertility-related quality of life compared to those attempting first-time IVF [8], possibly reflecting their longer-term adjustment to infertility diagnoses.
Conclusion 

Uterine transplantation has emerged as a viable solution for women with uterine factor infertility, offering new paths to biological motherhood. The remarkable 74% overall graft survival rate demonstrates the procedure’s technical feasibility, while clinical pregnancy rates of 36.3% and live birth rates of 22.0% per embryo transfer highlight its reproductive functionality. These outcomes rival those of conventional assisted reproductive technologies for certain patient populations.
Data from multiple transplant centers reveals several crucial insights:
- Both living and deceased donor transplants achieve comparable success rates, though living donor procedures show slightly higher graft survival (78% vs 64%) • Most recipients with viable grafts (83%) eventually achieve at least one live birth • Pregnancy typically begins relatively quickly, with most successful recipients achieving pregnancy within their first or second embryo transfer
The journey from transplant to motherhood follows a predictable timeline. First menstruation occurs approximately 30 days post-transplant, while embryo transfers begin between 64-551 days after surgery. This progressive path underscores the remarkable resilience of the transplanted organ and its ability to support normal reproductive functions.
Obstetric challenges certainly exist. Preterm birth affects nearly 75% of pregnancies following uterine transplant, with a median gestational age of 36 weeks. Hypertensive disorders represent another concern, affecting 14-24% of recipients during pregnancy. Nevertheless, these complications appear manageable with appropriate monitoring and intervention.
Perhaps most encouraging, children born through this procedure show overwhelmingly normal development. The absence of major congenital anomalies in most infants and their appropriate developmental progression through 36 months of follow-up provides reassurance about long-term outcomes. Though some children experience minor developmental delays, particularly in language acquisition, these issues appear largely comparable to general population rates.
The psychological dimension of uterine transplantation deserves equal consideration. Recipients generally maintain quality-of-life scores above population norms throughout their journey, though failed pregnancies and graft failures predictably impact mental wellbeing. Marital relationships face challenges during this intensive process, yet most couples demonstrate remarkable resilience.
Uterine transplantation stands as a testament to medical innovation, offering hope where none previously existed. The procedure has evolved from experimental to increasingly standardized, with protocols refined through methodical research across multiple international centers. While complications and challenges persist, the overall trajectory points toward continued improvement in outcomes.
For practitioners considering this option for patients with uterine factor infertility, several factors warrant consideration:
- Patient selection remains paramount, with strict medical criteria for both recipients and donors • Comprehensive pre-transplant counseling must address both physical and psychological aspects • Long-term immunosuppression management requires careful monitoring • Multidisciplinary care teams provide optimal support throughout the transplant and pregnancy journey
Uterine transplantation represents more than a surgical technique—it embodies the intersection of reproductive medicine, transplant surgery, maternal-fetal medicine, and psychological support. This groundbreaking procedure continues to evolve, offering renewed hope for biological motherhood among women previously limited to adoption or gestational surrogacy options.
Key Takeaways
Recent 2025 clinical trials reveal groundbreaking success rates for uterine transplantation, offering new hope for women with uterine factor infertility who previously had limited options for biological motherhood.
- Uterine transplant achieves 74% overall graft survival rate with 36.3% clinical pregnancy rate and 22.0% live birth rate per embryo transfer
- Both living and deceased donor transplants show comparable outcomes, with 83% of recipients with viable grafts eventually achieving live birth
- Most successful pregnancies occur within first two embryo transfers, typically beginning 64-551 days post-transplant
- Children born from transplanted uteri show normal development with 78.6% having no congenital anomalies and appropriate milestones through age 3
- Recipients maintain quality of life scores above population norms despite facing preterm birth in 75% of pregnancies and hypertensive complications
While uterine transplantation requires careful patient selection and comprehensive multidisciplinary care, these breakthrough results demonstrate that the procedure has evolved from experimental to increasingly standardized treatment. The success rates now rival conventional assisted reproductive technologies, making biological motherhood possible for women with conditions like MRKH syndrome or those who’ve undergone hysterectomy.
Frequently Asked Questions: 
FAQs
Q1. What is the current success rate of uterine transplants? Recent clinical trials show an overall uterine transplant success rate of 74%, with a clinical pregnancy rate of 36.3% and a live birth rate of 22.0% per embryo transfer. Among recipients with viable grafts, 83% eventually achieve at least one live birth.
Q2. Are there differences in outcomes between living and deceased donor uterine transplants? Both living and deceased donor transplants show comparable success rates. However, living donor procedures have a slightly higher graft survival rate of 78% compared to 64% for deceased donor transplants. The choice between living and deceased donors often depends on the transplant center’s expertise and protocol.
Q3. How long after a uterine transplant can a recipient attempt pregnancy? The time from transplant to first embryo transfer varies, ranging from 64 to 551 days. Most centers aim for 3-6 months post-transplant, with the median time being about 4 months. Regular menstruation, typically beginning around 30 days post-surgery, is a key indicator of graft readiness for embryo transfer.
Q4. What are the main complications in pregnancies following uterine transplant? The most common complications include preterm birth (affecting nearly 75% of pregnancies) and hypertensive disorders (affecting 14-24% of recipients). All deliveries are performed via cesarean section. Despite these challenges, most recipients maintain quality-of-life scores above population norms throughout their journey.
Q5. How do children born from transplanted uteri develop in the long term? Follow-up studies show that most children born after uterine transplant develop normally. About 78.6% have no congenital anomalies, and the majority reach appropriate developmental milestones through age 3. While some children may experience minor developmental delays, particularly in language acquisition, these issues appear largely comparable to general population rates.
References: 
[1] – https://obgyn.onlinelibrary.wiley.com/doi/10.1111/aogs.15003
[2] – https://www.fertstert.org/article/S0015-0282(24)00791-X/fulltext
[3] – https://jamanetwork.com/journals/jama/fullarticle/2822479
[4] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10607750/
[5] – https://obgyn.onlinelibrary.wiley.com/doi/full/10.1002/uog.26134
[6] – https://www.amjtransplant.org/article/S1600-6135(23)00062-X/fulltext
[7] – https://www.sciencedirect.com/science/article/pii/S0015028224002474
[8] – https://www.mdpi.com/2079-9721/13/5/152
[9] – https://pubmed.ncbi.nlm.nih.gov/37994646/
[10] – https://jamanetwork.com/journals/jamasurgery/fullarticle/2793976
[11] – https://academic.oup.com/humrep/article/39/2/374/7444825
[12] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9260640/
[13] – https://www.healio.com/news/womens-health-ob-gyn/20240815/feasible-uterus-transplant-associated-with-high-live-birth-rate-surgical-risks
[14] – https://www.eujtransplantation.com/article/view/533
[15] – https://www.contemporaryobgyn.net/view/uterus-transplants-high-live-birth-rate-longterm-safety
[16] – https://utsouthwestern.elsevierpure.com/en/publications/neonatal-outcomes-after-uterus-transplantation-dallas-uterus-tran/
[17] – https://obgyn.onlinelibrary.wiley.com/doi/10.1111/1471-0528.17270
[18] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10833084/
[19] – https://www.sciencedirect.com/science/article/pii/S0015028220303319
[20] – https://www.fertstert.org/article/S0015-0282(22)00462-9/pdf
[21] – https://pubmed.ncbi.nlm.nih.gov/32709381/
[22] – https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/aogs.15004
Video Section
Recent Articles


