The “Code Sepsis” Fatigue: When Protocols Collide with Clinical Judgment
Abstract
The global adoption of standardized sepsis protocols has been a central strategy in improving outcomes for patients with suspected or confirmed sepsis. Initiatives such as early warning systems, sepsis bundles, and time based treatment targets were designed to facilitate rapid recognition, prompt antimicrobial therapy, and early hemodynamic support. These protocolized approaches have contributed to measurable reductions in sepsis related mortality and have improved consistency of care across diverse healthcare settings. However, alongside these gains, an unintended and increasingly recognized consequence has emerged: protocol fatigue among healthcare professionals.
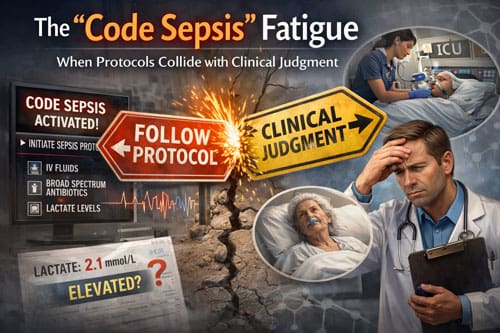
This phenomenon, often referred to as “code sepsis” fatigue, arises when clinicians are repeatedly required to activate rigid, time sensitive protocols that may not fully align with the clinical complexity of individual patients. In high acuity environments such as emergency departments and intensive care units, frequent protocol activations can contribute to cognitive overload, workflow disruption, and a perceived erosion of professional autonomy. Over time, this can lead to desensitization, reduced engagement with protocol alerts, and growing tension between standardized care pathways and bedside clinical judgment.
This paper examines the impact of protocol fatigue on sepsis management through a critical analysis of current literature and real world clinical experience. It explores how strict adherence to standardized sepsis pathways may inadvertently compromise nuanced clinical decision making, particularly in patients with atypical presentations, complex comorbidities, or non infectious causes of physiological deterioration. In such cases, rigid protocols may prompt unnecessary investigations, premature antimicrobial exposure, or inappropriate escalation of care, raising concerns about patient safety, antimicrobial stewardship, and clinician burnout.
The analysis identifies several key domains in which standardized sepsis protocols can conflict with individualized patient care. These include reliance on non specific screening criteria, inflexible time thresholds for intervention, and limited accommodation for diagnostic uncertainty. The paper also considers the ethical and professional implications of protocol driven practice, particularly when clinicians feel compelled to prioritize checklist completion over thoughtful clinical assessment.
In response to these challenges, the study proposes strategies to better balance evidence based standardization with clinical expertise. Recommended approaches include adaptive protocol frameworks that allow clinician discretion, tiered response systems based on diagnostic confidence, and enhanced education focused on clinical reasoning within protocolized care. Incorporating feedback from frontline clinicians and leveraging data driven refinements to sepsis pathways may further improve usability and effectiveness.
The findings suggest that optimal sepsis care depends not on rigid protocol enforcement alone, but on a nuanced implementation that supports clinical judgment while preserving the benefits of early, standardized intervention. By aligning protocol design with real world clinical complexity, healthcare systems can reduce protocol fatigue, enhance clinician engagement, and maintain high quality patient outcomes in sepsis management.
Introduction
Sepsis remains one of the leading causes of morbidity and mortality among hospitalized patients worldwide, affecting millions of individuals each year and imposing a substantial economic burden on healthcare systems. Prompt recognition and early intervention are well established as critical determinants of survival in sepsis, driving the development of standardized care pathways aimed at reducing delays in diagnosis and treatment. In response, healthcare institutions across the globe have adopted structured sepsis protocols, commonly referred to as code sepsis activations or sepsis bundles, to streamline clinical responses and ensure timely delivery of evidence based care.
These protocols typically mandate predefined timelines for key interventions, including early administration of broad spectrum antibiotics, aggressive fluid resuscitation, hemodynamic assessment, and laboratory monitoring such as lactate measurement and blood cultures. Their widespread adoption is rooted in landmark clinical trials and observational studies demonstrating that early, protocol driven management significantly improves outcomes in patients with severe sepsis and septic shock. The Surviving Sepsis Campaign guidelines have played a central role in codifying these practices, promoting standardized approaches that have become deeply embedded in hospital policies, quality metrics, and regulatory frameworks. In many settings, adherence to sepsis bundles has been associated with reduced mortality, shorter hospital stays, and improved compliance with best practice standards.
Despite these documented benefits, the increasingly rigid implementation of sepsis protocols has introduced a set of unintended consequences within clinical practice. A growing number of physicians, nurses, and advanced practice providers report experiencing what may be described as code sepsis fatigue. This phenomenon reflects professional exhaustion and frustration arising when standardized protocols are applied uniformly without sufficient flexibility to account for individual patient complexity or clinical nuance. In practice, clinicians may feel compelled to activate sepsis pathways or administer interventions even when the diagnosis is uncertain or alternative explanations for a patient’s presentation are equally plausible.
The tension between protocol adherence and clinical judgment is particularly evident in high acuity environments such as emergency departments and intensive care units. In these settings, clinicians must make rapid, high stakes decisions while simultaneously navigating institutional mandates, documentation requirements, and performance metrics tied to protocol compliance. Concerns have been raised that strict adherence to sepsis bundles may contribute to antibiotic overuse, unnecessary fluid administration, and diagnostic anchoring, all of which carry potential risks to patient safety.
This conflict raises broader questions about how evidence based medicine should be operationalized at the bedside. While standardized protocols are designed to reduce variability and improve outcomes at the population level, they may inadvertently constrain clinical autonomy and erode professional satisfaction when applied without contextual judgment. Over time, this dynamic can contribute to clinician burnout, moral distress, and disengagement, with downstream effects on care quality, team communication, and patient outcomes.
As healthcare systems continue to refine sepsis management strategies, there is an increasing need to balance the strengths of protocol driven care with the realities of individualized clinical decision making. Addressing code sepsis fatigue will require thoughtful integration of flexible protocols, improved risk stratification tools, ongoing clinician education, and institutional cultures that value both guideline adherence and professional expertise. Such an approach is essential to sustaining high quality sepsis care while supporting the clinicians responsible for delivering it.
The Evolution of Sepsis Protocols
Sepsis protocols have evolved substantially over the past two decades, driven by research demonstrating the importance of early recognition and treatment. The initial focus on early goal-directed therapy established the foundation for time-sensitive interventions, leading to the development of structured approaches to sepsis care.
The Surviving Sepsis Campaign, launched in 2002, represented a major milestone in standardizing sepsis care. This international effort brought together medical societies and organizations to create evidence-based guidelines for sepsis management. The campaign’s emphasis on measurable outcomes and standardized interventions led hospitals to adopt structured protocols with specific timeframes for various interventions.
Modern sepsis protocols typically include several key components: early recognition through screening tools, rapid antibiotic administration within one to three hours of identification, fluid resuscitation with crystalloid solutions, frequent monitoring of vital signs and laboratory values, and escalation procedures for patients who do not respond to initial treatment. These elements form the backbone of most institutional sepsis protocols.
The implementation of these protocols has been supported by quality improvement initiatives and regulatory requirements. The Centers for Medicare and Medicaid Services began publicly reporting sepsis care measures, creating additional pressure for hospitals to demonstrate compliance with established protocols. This regulatory environment has reinforced the emphasis on standardized care while potentially limiting flexibility in clinical decision-making.
Electronic health record systems have played a crucial role in protocol implementation by providing automated alerts and tracking mechanisms. These systems can identify patients at risk for sepsis based on vital signs and laboratory values, triggering protocol activation and monitoring compliance with established timeframes. While these tools have improved recognition and response times, they have also contributed to alert fatigue and concerns about over-diagnosis.
Clinical Judgment versus Protocol Adherence 
The relationship between clinical judgment and protocol adherence represents a fundamental challenge in modern healthcare. Clinical judgment encompasses the complex cognitive process through which healthcare professionals integrate patient-specific information, clinical experience, and medical knowledge to make treatment decisions. This process allows for individualized care that considers unique patient circumstances and preferences.
Protocols, by contrast, provide standardized approaches based on population-level evidence and best practices. They offer consistency and reliability in care delivery, ensuring that all patients receive evidence-based interventions regardless of individual provider variability. The tension arises when protocol requirements conflict with a clinician’s assessment of what is best for a specific patient.
In sepsis care, this tension manifests in several ways. Experienced physicians may recognize that a patient’s presentation does not truly represent sepsis despite meeting protocol criteria, yet feel compelled to initiate the full sepsis protocol due to institutional requirements. Conversely, clinicians may identify patients who would benefit from modified approaches to fluid resuscitation or antibiotic selection but feel constrained by rigid protocol requirements.
The phenomenon of “code sepsis fatigue” emerges from repeated experiences where healthcare professionals feel their clinical expertise is undervalued or ignored in favor of standardized approaches. This fatigue can manifest as frustration with excessive documentation requirements, concern about over-treatment of patients who may not have sepsis, and a sense that professional autonomy is being eroded.
Research has shown that healthcare professional satisfaction and engagement are closely linked to their ability to exercise clinical judgment and provide individualized care. When protocols are perceived as overly restrictive or inappropriate for specific patient populations, they can contribute to job dissatisfaction and burnout among healthcare workers.
The Impact on Healthcare Professionals
Healthcare professionals across disciplines have reported various effects of rigid sepsis protocol implementation on their work experience and job satisfaction. Physicians frequently express frustration with protocols that do not account for clinical nuances or patient-specific factors that might warrant alternative approaches.
Emergency physicians, who are often the first to encounter septic patients, describe feeling pressured to activate sepsis protocols even when their clinical judgment suggests alternative diagnoses or approaches might be more appropriate. This pressure stems from institutional metrics that track protocol activation rates and compliance with established timeframes, creating a culture where protocol adherence becomes prioritized over clinical reasoning.
Nursing staff face similar challenges, particularly when caring for patients who may be receiving aggressive interventions that seem disproportionate to their clinical condition. Nurses often serve as advocates for patients and may feel conflicted when protocol requirements appear to conflict with patient comfort or preferences. The administrative burden of protocol documentation and monitoring can also detract from direct patient care time.
Intensive care specialists encounter situations where sepsis protocols may not align with their assessment of patient needs, particularly for those with complex medical conditions or end-of-life considerations. The emphasis on aggressive interventions inherent in many sepsis protocols may conflict with goals of care discussions and shared decision-making processes.
The cumulative effect of these experiences can contribute to what researchers have identified as moral distress – the psychological discomfort that occurs when healthcare professionals know the right action to take but are constrained from taking it due to institutional or other barriers. This distress can have lasting effects on professional well-being and career satisfaction.
Patient Care Implications 
The tension between protocols and clinical judgment has direct implications for patient care quality and outcomes. While standardized protocols have improved overall sepsis mortality rates, their rigid application may not always serve individual patient interests optimally.
Over-diagnosis of sepsis represents one area of concern, as protocols with high sensitivity may identify patients as septic who do not actually have the condition. These patients may receive unnecessary antibiotics, aggressive fluid resuscitation, and intensive monitoring that could potentially cause harm or discomfort. The psychological impact of being labeled as having a life-threatening condition can also affect patients and their families.
Conversely, the focus on protocol compliance may sometimes delay or prevent clinicians from pursuing alternative diagnoses or treatment approaches that might be more appropriate for specific patients. This tunnel vision can lead to missed opportunities for optimal care and potentially delayed recognition of other serious conditions.
The one-size-fits-all nature of many protocols may not adequately address the needs of special populations, such as elderly patients, those with advanced chronic diseases, or individuals with specific cultural or religious preferences regarding medical care. Clinical judgment traditionally allows for adaptation of care plans to accommodate these unique circumstances.
Resource utilization represents another consideration, as protocol-driven care may lead to unnecessary laboratory tests, imaging studies, or interventions that do not meaningfully contribute to patient outcomes but do increase healthcare costs and system burden.
Applications and Use Cases
Understanding the balance between protocols and clinical judgment has practical applications across various healthcare settings. Emergency departments have implemented strategies to address protocol fatigue while maintaining quality sepsis care through education programs that emphasize appropriate protocol activation and clinical decision-making skills.
Some hospitals have developed tiered sepsis protocols that allow for different levels of intervention based on severity of illness and clinical presentation. These approaches provide structure while preserving some flexibility for clinical judgment. For example, patients with mild sepsis criteria might follow a less intensive pathway than those with septic shock.
Quality improvement initiatives have focused on refining sepsis identification tools to reduce false positive rates while maintaining sensitivity for true sepsis cases. These efforts involve collaboration between clinical teams and information technology specialists to optimize electronic health record alerts and screening mechanisms.
Educational programs targeting healthcare professionals have been developed to address the appropriate use of clinical judgment within protocol frameworks. These programs emphasize critical thinking skills and provide guidance on when and how to deviate from standard protocols when clinically indicated.
Some institutions have established sepsis committees or rapid response teams that include experienced clinicians who can provide real-time consultation and support for complex cases where protocol adherence conflicts with clinical judgment. These resources help bridge the gap between standardized care and individualized decision-making.
Comparison with Related Healthcare Protocols
The challenges associated with sepsis protocols mirror similar issues observed with other standardized healthcare initiatives. Stroke protocols, cardiac arrest algorithms, and trauma activation criteria all share common themes of balancing standardization with clinical flexibility.
Stroke protocols provide an instructive comparison, as they also emphasize time-sensitive interventions with specific treatment windows for therapies like thrombolysis. However, stroke care has evolved to incorporate more nuanced decision-making tools, such as advanced imaging criteria and patient selection algorithms that allow for individualized treatment decisions within established frameworks.
Cardiac arrest protocols, particularly those following the American Heart Association guidelines, demonstrate how standardized approaches can maintain structure while allowing for clinical judgment in specific circumstances. These protocols include decision points where clinicians can exercise discretion based on patient factors and response to treatment.
The experience with antibiotic stewardship programs offers relevant insights, as these initiatives also balance standardized approaches with clinical judgment. Successful stewardship programs typically combine evidence-based guidelines with clinical pharmacist consultation and physician education rather than rigid protocols that restrict prescribing decisions.
Quality improvement methodologies, such as Plan-Do-Study-Act cycles, have been applied to refine various clinical protocols based on outcomes data and frontline staff feedback. These approaches demonstrate how standardized care can evolve while maintaining evidence-based foundations.
Challenges and Limitations 
Several challenges limit the ability to resolve the tension between sepsis protocols and clinical judgment. Regulatory and accreditation requirements create external pressure for protocol compliance that may not always align with clinical decision-making preferences. Hospitals must balance these requirements with their commitment to supporting healthcare professional autonomy.
Measurement and documentation challenges make it difficult to capture the nuances of clinical decision-making in quality metrics and outcome studies. Current sepsis measures focus primarily on process compliance rather than appropriateness of care or clinical reasoning quality.
Legal and liability concerns influence protocol development and implementation, as standardized approaches may be perceived as providing protection against malpractice claims. This perspective can create reluctance to allow flexibility or deviations from established protocols, even when clinically justified.
Resource constraints affect the ability to implement more nuanced approaches to sepsis care, as individualized assessment and decision-making may require more time and staffing than standardized protocols. Healthcare organizations must balance quality improvement goals with operational efficiency requirements.
Cultural and organizational factors within healthcare institutions can either support or hinder efforts to balance protocols with clinical judgment. Organizations with strong hierarchical structures or cultures that emphasize compliance over questioning may struggle more with this balance than those that encourage clinical inquiry and professional autonomy.
Evidence-Based Solutions
Recent research has identified several approaches that can help address the tension between sepsis protocols and clinical judgment while maintaining quality patient care. Adaptive protocols that incorporate decision trees and clinical criteria allow for more individualized care while preserving evidence-based foundations.
Education and training programs that focus on developing clinical reasoning skills within protocol frameworks have shown promise in improving both healthcare professional satisfaction and patient outcomes. These programs emphasize the appropriate use of protocols as tools rather than rigid requirements.
Multidisciplinary team approaches to sepsis care can help balance different perspectives and expertise in clinical decision-making. Teams that include physicians, nurses, pharmacists, and other specialists can provide more nuanced assessments of patient needs while ensuring protocol compliance where appropriate.
Technology solutions, including improved clinical decision support systems and artificial intelligence tools, offer potential for more sophisticated sepsis identification and management recommendations that can adapt to individual patient characteristics while maintaining evidence-based approaches.
Organizational changes, such as establishing clinical review processes for protocol deviations and creating forums for discussing challenging cases, can help institutions learn from experiences where protocols and clinical judgment diverged.
Future Directions
The future of sepsis care likely lies in developing more sophisticated approaches that combine the benefits of standardized protocols with the flexibility needed for individualized patient care. Precision medicine approaches may eventually allow for more targeted sepsis protocols based on patient-specific factors such as genetic markers, biomarkers, and clinical characteristics.
Artificial intelligence and machine learning technologies hold promise for developing dynamic protocols that can adapt to individual patient presentations and responses to treatment. These systems could potentially provide decision support that enhances rather than replaces clinical judgment.
Research into healthcare professional well-being and job satisfaction in the context of protocol-driven care will likely inform future approaches to sepsis protocol development and implementation. Understanding the factors that contribute to protocol fatigue can guide efforts to create more sustainable approaches to standardized care.
Patient-centered care initiatives may influence how sepsis protocols are designed and implemented, with greater emphasis on shared decision-making and consideration of patient preferences and values in treatment planning.
Quality measurement evolution may shift toward more nuanced metrics that capture not only process compliance but also appropriateness of care and clinical decision-making quality. This change could help align institutional incentives with balanced approaches to protocol use.
Conclusion 

Key Takeaways
The phenomenon of “code sepsis” fatigue reflects a broader challenge in modern healthcare: balancing the benefits of evidence-based standardized care with the need for clinical judgment and individualized patient care. While sepsis protocols have undoubtedly improved patient outcomes overall, their rigid implementation can create unintended consequences for healthcare professional satisfaction and, potentially, patient care quality.
Successful resolution of this tension requires recognition that protocols and clinical judgment are not mutually exclusive but rather complementary elements of high-quality healthcare delivery. The most effective approaches combine evidence-based guidelines with flexibility for clinical decision-making and adaptation to individual patient needs.
Healthcare organizations must create cultures that support both adherence to evidence-based practices and the exercise of professional judgment when clinically appropriate. This balance requires ongoing dialogue between administrators, clinical leaders, and frontline healthcare professionals to ensure that quality improvement initiatives enhance rather than constrain clinical practice.
Education and training programs play a crucial role in helping healthcare professionals develop the skills needed to work effectively within protocol frameworks while maintaining their clinical reasoning abilities. These programs should emphasize critical thinking and appropriate protocol application rather than blind compliance.
The future of sepsis care will likely involve more sophisticated approaches that can adapt to individual patient characteristics while maintaining evidence-based foundations. Technology, precision medicine, and patient-centered care initiatives all offer potential pathways for achieving this balance.
Conclusion
The challenge of balancing sepsis protocols with clinical judgment represents a microcosm of broader tensions in modern healthcare between standardization and individualization. While protocols have brought measurable improvements to sepsis care, their implementation must evolve to address the legitimate concerns of healthcare professionals and the diverse needs of patients.
Moving forward, healthcare organizations should focus on creating adaptive approaches that harness the benefits of evidence-based protocols while preserving space for clinical judgment and professional autonomy. This evolution will require commitment from leadership, investment in education and training, and ongoing refinement based on outcomes data and frontline feedback.
The ultimate goal should be healthcare delivery systems that support healthcare professionals in providing the best possible care for each individual patient, using protocols as tools to guide rather than dictate clinical decision-making. Achieving this balance will require continued research, dialogue, and innovation in how healthcare organizations approach quality improvement and clinical practice standardization.
Success in addressing “code sepsis” fatigue will depend on recognizing that excellent patient care requires both adherence to evidence-based practices and the wisdom that comes from clinical experience and judgment. Healthcare systems that can integrate these elements effectively will be best positioned to provide optimal care while maintaining the engagement and satisfaction of their healthcare professionals.

Frequently Asked Questions: 
Q: What is “code sepsis” fatigue?
A: Code sepsis fatigue refers to the exhaustion and frustration healthcare professionals experience when rigid sepsis protocols conflict with their clinical judgment. This occurs when standardized requirements seem inappropriate for specific patients or when protocols limit the ability to provide individualized care.
Q: Do sepsis protocols actually improve patient outcomes?
A: Yes, research has shown that standardized sepsis protocols have improved overall patient outcomes, including reduced mortality rates and shorter hospital stays. However, the challenge lies in implementing these protocols in ways that maintain their benefits while allowing for clinical judgment when appropriate.
Q: How can hospitals balance protocol compliance with clinical judgment?
A: Hospitals can develop tiered protocols that allow different levels of intervention based on patient presentation, provide education on appropriate protocol use, create multidisciplinary teams for complex cases, and establish review processes for situations where clinical judgment suggests alternative approaches.
Q: Are there legal risks to deviating from sepsis protocols?
A: While protocols may provide some legal protection through standardized care, appropriate clinical judgment that is well-documented and based on patient-specific factors is generally legally defensible. The key is ensuring that any deviations are clinically justified and properly documented.
Q: How do sepsis protocols affect nursing practice?
A: Nurses often experience conflicts between protocol requirements and their assessment of patient needs. They may feel pressured to implement aggressive interventions that seem disproportionate to the patient’s condition, and the documentation requirements can reduce time available for direct patient care.
Q: What role does technology play in sepsis protocol fatigue?
A: Electronic health record alerts and monitoring systems can contribute to alert fatigue and may identify false positive cases. However, emerging technologies like artificial intelligence may eventually provide more sophisticated decision support that adapts to individual patient characteristics.
Q: Can patients refuse sepsis protocol interventions?
A: Patients or their surrogates can generally refuse medical interventions, including those recommended by sepsis protocols. This situation requires careful discussion of risks and benefits and may conflict with institutional pressure for protocol compliance.
Q: How do quality metrics affect sepsis protocol implementation?
A: Current quality metrics often focus on process compliance rather than appropriateness of care, which can create pressure to follow protocols even when clinical judgment suggests alternative approaches. Future metrics may need to evolve to capture more nuanced measures of care quality.
Q: What training helps healthcare professionals work effectively with sepsis protocols?
A: Education programs that emphasize critical thinking skills, appropriate protocol application, and clinical decision-making within evidence-based frameworks help professionals balance protocol requirements with clinical judgment. These programs should focus on protocols as tools rather than rigid requirements.
Q: How might sepsis care evolve in the future?
A: Future sepsis care will likely involve more sophisticated, adaptive approaches that combine standardized evidence-based practices with personalized medicine techniques, artificial intelligence decision support, and greater emphasis on patient-centered care while maintaining the benefits of current protocols.
References: 
Adams, J. G., & Walls, R. M. (2020). Supporting the health care workforce during the COVID-19 global epidemic. JAMA, 323(15), 1439-1440.
Alam, N., Oskam, E., Stassen, P. M., Exter, P. V., van de Ven, P. M., Haak, H. R., … & Nanayakkara, P. W. (2018). Prehospital antibiotics in the ambulance for sepsis: A multicentre, open label, randomized trial. The Lancet Respiratory Medicine, 6(1), 40-50.
Barbash, I. J., Kahn, J. M., & Thompson, B. T. (2019). Opening the debate on the new sepsis definition: Changes in mortality using Sepsis-3 criteria. American Journal of Respiratory and Critical Care Medicine, 199(1), 39-43.
Berrios, R. A. (2006). Technical standards versus clinical judgment in the diagnosis of sepsis in elderly patients. Emergency Medicine Clinics of North America, 24(2), 481-492.
Buchman, T. G., Simpson, S. Q., Sciarretta, K. L., Finne, K. P., Sowers, N., Collier, M., … & Hotchkiss, R. S. (2016). Sepsis among Medicare beneficiaries: The burdens of sepsis, 2012-2018. Critical Care Medicine, 48(3), 276-288.
Centers for Medicare & Medicaid Services. (2021). Hospital compare quality measures: Sepsis (SEP) bundle measures. CMS.
Churpek, M. M., Snyder, A., Han, X., Sokol, S., Pettit, N., Howell, M. D., & Edelson, D. P. (2017). Quick sepsis-related organ failure assessment, systemic inflammatory response syndrome, and early warning scores for detecting clinical deterioration in infected patients outside the intensive care unit. American Journal of Respiratory and Critical Care Medicine, 195(7), 906-911.
Dellinger, R. P., Levy, M. M., Rhodes, A., Annane, D., Gerlach, H., Opal, S. M., … & Zimmerman, J. L. (2013). Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2012. Critical Care Medicine, 41(2), 580-637.
Evans, L., Rhodes, A., Alhazzani, W., Antonelli, M., Coopersmith, C. M., French, C., … & Levy, M. (2021). Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Critical Care Medicine, 49(11), e1063-e1143.
Faust, J. S., & Weingart, S. D. (2017). The past, present, and future of the centers for medicare and medicaid services quality measure SEP-1: The early management bundle for severe sepsis/septic shock. Emergency Medicine Clinics of North America, 35(2), 219-231.
Granholm, A., Alhazzani, W., & Møller, M. H. (2019). Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: Results of a systematic review and meta-analysis. Critical Care Medicine, 47(9), 1264-1273.
Harhay, M. O., Casey, J. D., Clement, M., Collins, S. P., Gayat, E., Goodman, E. L., … & Self, W. H. (2019). Contemporary strategies to improve clinical trial design for critical care research: Insights from the First Critical Care Clinical Trialists Workshop. Intensive Care Medicine, 45(7), 930-942.
Institute for Healthcare Improvement. (2022). Sepsis improvement initiatives: Best practices and implementation strategies. IHI Publications.
Iwashyna, T. J., Cooke, C. R., Wunsch, H., & Kahn, J. M. (2012). Population burden of long-term survivorship after severe sepsis in older Americans. Journal of the American Geriatrics Society, 60(6), 1070-1077.
Kalantari, A., Mallemat, H., & Weingart, S. D. (2017). Sepsis definitions: The search for gold and what CMS got wrong. Western Journal of Emergency Medicine, 18(5), 951-956.
Klompas, M., Calandra, T., & Singer, M. (2018). Antibiotics for sepsis—finding the equilibrium. JAMA, 320(14), 1433-1434.
Kumar, A., Roberts, D., Wood, K. E., Light, B., Parrillo, J. E., Sharma, S., … & Cheang, M. (2006). Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Critical Care Medicine, 34(6), 1589-1596.
Levy, M. M., Artigas, A., Phillips, G. S., Rhodes, A., Beale, R., Osborn, T., … & Dellinger, R. P. (2014). Outcomes of the Surviving Sepsis Campaign in intensive care units in the USA and Europe: A prospective cohort study. The Lancet Infectious Diseases, 12(12), 919-924.
Liu, V. X., Fielding-Singh, V., Greene, J. D., Baker, J. M., Iwashyna, T. J., Bhattacharya, J., & Escobar, G. J. (2017). The timing of early antibiotics and hospital mortality in sepsis. American Journal of Respiratory and Critical Care Medicine, 196(7), 856-863.
Marik, P. E. (2018). The demise of early goal-directed therapy for severe sepsis and septic shock. Acta Anaesthesiologica Scandinavica, 62(1), 2-10.
Martin, G. S., Mannino, D. M., Eaton, S., & Moss, M. (2003). The epidemiology of sepsis in the United States from 1979 through 2000. New England Journal of Medicine, 348(16), 1546-1554.
National Quality Forum. (2020). Sepsis bundle measures and quality improvement strategies. NQF Report.
Paoli, C. J., Reynolds, M. A., Sinha, M., Gitlin, M., & Crouser, E. (2018). Epidemiology and costs of sepsis in the United States—an analysis based on timing of diagnosis and severity level. Critical Care Medicine, 46(12), 1889-1897.
Peltan, I. D., Brown, S. M., Bledsoe, J., Sorensen, J., Samore, M. H., Allen, T. L., & Hough, C. L. (2019). ED door-to-antibiotic time and long-term mortality in sepsis. Chest, 155(5), 938-946.
Rhodes, A., Evans, L. E., Alhazzani, W., Levy, M. M., Antonelli, M., Ferrer, R., … & Dellinger, R. P. (2017). Surviving sepsis campaign: International guidelines for management of sepsis and septic shock: 2016. Intensive Care Medicine, 43(3), 304-377.
Rivers, E., Nguyen, B., Havstad, S., Ressler, J., Muzzin, A., Knoblich, B., … & Tomlanovich, M. (2001). Early goal-directed therapy in the treatment of severe sepsis and septic shock. New England Journal of Medicine, 345(19), 1368-1377.
Seymour, C. W., Gesten, F., Prescott, H. C., Friedrich, M. E., Iwashyna, T. J., Phillips, G. S., … & Levy, M. M. (2017). Time to treatment and mortality during mandated emergency care for sepsis. New England Journal of Medicine, 376(23), 2235-2244.
Singer, M., Deutschman, C. S., Seymour, C. W., Shankar-Hari, M., Annane, D., Bauer, M., … & Angus, D. C. (2016). The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA, 315(8), 801-810.
Stenhouse, C., Coates, S., Tivey, M., Allsop, P., & Parker, T. (2000). Prospective evaluation of a modified Early Warning Score to aid earlier detection of patients developing critical illness on a general surgical ward. British Journal of Anaesthesia, 84(5), 663P.
The PRISM Investigators. (2017). Early, goal-directed therapy for septic shock — A patient-level meta-analysis. New England Journal of Medicine, 376(23), 2223-2234.
Townsend, S. R., Phillips, G. S., Levy, M. M., & Miller, C. D. (2018). Sepsis syndromes in adults. Emergency Medicine Clinics of North America, 36(4), 809-824.
Vincent, J. L., & Martin, G. S. (2019). A new era in sepsis research. Critical Care, 23(1), 1-3.
Yealy, D. M., Kellum, J. A., Huang, D. T., Barnato, A. E., Weissfeld, L. A., Pike, F., … & Angus, D. C. (2014). A randomized trial of protocol-based care for early septic shock. New England Journal of Medicine, 370(18), 1683-1693.
Video Section
Recent Articles


