The Hidden Link Between Psoriasis and Crohn’s: Essential Insights for Clinical Practice
Introduction
Psoriasis and Crohn’s disease share a complex and clinically notable relationship that extends well beyond coincidental comorbidity. Psoriasis, a chronic immune-mediated skin condition, affects an estimated 2% to 3% of the global population, with approximately 40 million prevalent cases reported in 2019. While psoriasis has long been recognized as a systemic disorder associated with multiple comorbidities, mounting evidence indicates a particularly strong and causal connection with Crohn’s disease, a major subtype of inflammatory bowel disease (IBD).
Recent advances in genetic epidemiology, particularly Mendelian randomization studies, provide compelling evidence that psoriasis and IBD exert reciprocal influences on each other’s development and progression. Genetically predicted IBD is associated with an elevated risk of psoriasis (pooled odds ratio 1.10) and psoriatic arthritis (pooled odds ratio 1.10). When analyzed by IBD subtype, Crohn’s disease demonstrates a stronger association, with higher odds of psoriasis (OR 1.16) and psoriatic arthritis (OR 1.13), compared with ulcerative colitis. Conversely, psoriasis itself appears to increase the risk of Crohn’s disease by approximately 35% (OR 1.350), while psoriatic arthritis raises the risk by nearly 32% (OR 1.319). These bidirectional associations suggest that the relationship is not incidental but reflects shared immunological and genetic mechanisms.
Both psoriasis and Crohn’s disease fall within the broader spectrum of immune-mediated inflammatory diseases (IMIDs). These conditions are characterized by overlapping pathogenic pathways, including dysregulation of the Th17/IL-23 axis, altered barrier function, and shared genetic predispositions. The convergence of these mechanisms may help explain the clinical observation that patients with psoriasis are at increased risk of developing Crohn’s disease, and vice versa.
From a clinical standpoint, this relationship carries important implications for diagnosis, monitoring, and treatment. Healthcare professionals should be aware that patients presenting with psoriasis, especially those with moderate-to-severe disease or concomitant psoriatic arthritis, may be at heightened risk of developing Crohn’s disease. Similarly, individuals with Crohn’s disease should be evaluated for cutaneous manifestations consistent with psoriasis. Integrated, multidisciplinary care involving dermatologists, gastroenterologists, and rheumatologists is therefore essential to optimize outcomes.
In conclusion, psoriasis and Crohn’s disease represent interconnected immune-mediated conditions with a clear bidirectional relationship supported by genetic and clinical evidence. Recognition of this link underscores the need for vigilant patient assessment, early detection of comorbidities, and coordinated management strategies. Ongoing research into the shared pathogenic pathways will be critical for refining preventive strategies and developing targeted therapies that address both disorders simultaneously.
Keywords: psoriasis, Crohn’s disease, immune-mediated inflammatory diseases, comorbidity, bidirectional association
Understanding the Clinical Overlap Between Psoriasis and Crohn’s Disease
The clinical presentation patterns of psoriasis and Crohn’s disease exhibit remarkable parallels that extend beyond mere coincidence. Examining these overlaps provides valuable insights for clinicians managing patients with either or both conditions.
Shared prevalence patterns in high-income countries
Epidemiological data reveals intriguing geographic and socioeconomic patterns in the distribution of both psoriasis and Crohn’s disease. These immune-mediated inflammatory disorders demonstrate notably higher prevalence rates in North America and Northern European countries compared to regions in Asia, Africa, and South America.
Moreover, both conditions show a distinct north-south gradient, especially within Europe, with higher rates observed in northern countries. This geographical distribution pattern suggests common environmental triggers or genetic susceptibilities that may influence the development of both disorders. Additionally, industrialized nations consistently report higher incidence rates of both conditions, pointing toward potential shared environmental factors related to western lifestyle, dietary patterns, or urbanization.
The prevalence of psoriasis ranges from 0.09% to 11.4% worldwide, with developed countries typically reporting rates between 1.5-5%. Correspondingly, Crohn’s disease shows a similar pattern with the highest incidence rates in North America (20.2 per 100,000 person-years), followed by Europe (12.7 per 100,000 person-years). The parallel distribution suggests common underlying mechanisms that may be influenced by similar environmental exposures or immunological responses.
Furthermore, research indicates that patients with psoriasis have approximately a 2.5-fold increased risk of developing inflammatory bowel disease compared to the general population. Likewise, IBD patients demonstrate a 1.5 to 2.5 times higher likelihood of developing psoriasis than individuals without IBD. This reciprocal relationship further strengthens the case for shared pathophysiological pathways.
Age of onset and gender distribution similarities
The age of onset profiles for psoriasis and Crohn’s disease display noteworthy similarities. Both conditions typically manifest in a bimodal pattern, with initial peaks occurring in early adulthood (15-30 years) and secondary peaks in later life (50-70 years). This parallel timing of disease manifestation suggests potential shared triggers or biological pathways that become activated during these specific life stages.
Consequently, this bimodal distribution has important implications for clinical surveillance. Dermatologists treating young adults with psoriasis should maintain heightened awareness of potential gastrointestinal symptoms, while gastroenterologists managing young Crohn’s disease patients should likewise monitor for cutaneous manifestations.
Regarding gender distribution, the patterns show subtle yet important similarities. Psoriasis affects men and women nearly equally, with some studies suggesting a slight male predominance. Similarly, Crohn’s disease demonstrates a relatively balanced gender distribution in most populations, though certain regions report a slight female predominance. This near-equal gender distribution distinguishes these conditions from many other autoimmune disorders that typically show strong female predominance.
Nevertheless, differences emerge when examining disease subtypes. Psoriatic arthritis, which affects approximately 30% of psoriasis patients, shows slight male predominance, while certain phenotypes of Crohn’s disease may demonstrate gender-specific patterns. These nuanced differences highlight the complex interplay between genetic and environmental factors in disease expression.
The temporal relationship between the onset of these conditions also merits attention. Studies indicate that psoriasis typically precedes the diagnosis of Crohn’s disease in patients affected by both conditions. This sequence suggests that dermatological manifestations may serve as early indicators of potential gastrointestinal inflammation, thereby offering an opportunity for earlier screening and intervention in high-risk individuals.

Genetic Evidence Linking Crohn’s Disease and Psoriasis
Molecular genetic research has uncovered compelling evidence of shared pathogenic mechanisms underlying both psoriasis and Crohn’s disease. The genetic architecture of these disorders reveals overlapping susceptibility loci that help explain their frequent co-occurrence in clinical settings.
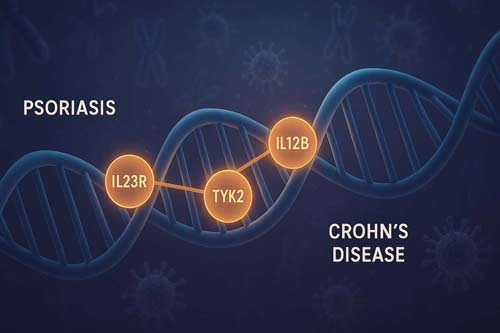
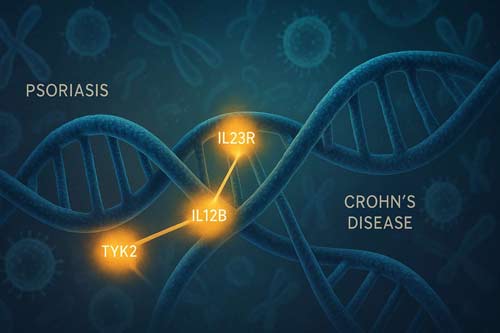
Shared susceptibility loci: IL23R, IL12B, TYK2
Genome-wide association studies (GWAS) have identified several genetic regions that influence susceptibility to both psoriasis and Crohn’s disease. Perhaps the most notable among these shared loci are those involving the IL-23/Th17 pathway, which plays a central role in regulating inflammatory responses.
The interleukin-23 receptor gene (IL23R) represents one of the strongest genetic links between these conditions. Variants in this gene increase the risk of developing both psoriasis and Crohn’s disease through dysregulation of IL-23 signaling, which subsequently promotes pathogenic T-cell responses. Indeed, the rs11209026 polymorphism in IL23R has been associated with protection against both disorders, highlighting its importance in their pathogenesis.
Another key shared genetic factor is the IL12B gene, which encodes the p40 subunit common to both IL-12 and IL-23 cytokines. Polymorphisms in this gene affect the production and function of these cytokines, thereby influencing T-cell differentiation and inflammatory responses in both skin and intestinal tissues. As a result, these genetic variations create a predisposition to both conditions through similar immunological mechanisms.
Tyrosine kinase 2 (TYK2) represents a third crucial shared susceptibility locus. This gene encodes an enzyme involved in signal transduction for multiple cytokine receptors, including those for IL-12 and IL-23. Certain TYK2 variants confer protection against both psoriasis and Crohn’s disease by modulating cytokine signaling pathways that regulate inflammatory responses.
Role of HLA-Cw6 and PSORS1 in psoriasis
The major histocompatibility complex (MHC) region harbors some of the strongest genetic associations for immune-mediated disorders. For psoriasis, the human leukocyte antigen C*06:02 (HLA-Cw6) allele within the PSORS1 (Psoriasis Susceptibility 1) locus on chromosome 6p21.3 constitutes the primary genetic determinant.
HLA-Cw6 increases psoriasis risk by approximately 10-fold in heterozygotes and 20-fold in homozygotes. This allele influences antigen presentation to T cells, potentially allowing the recognition of self-antigens that trigger psoriatic inflammation. Despite its strong association with psoriasis, HLA-Cw6 shows a more complex relationship with Crohn’s disease, suggesting some genetic distinction between these conditions.
The PSORS1 locus contains several genes beyond HLA-C that may contribute to psoriasis susceptibility, including CCHCR1 (coiled-coil alpha-helical rod protein 1) and CDSN (corneodesmosin). These genes affect keratinocyte proliferation and differentiation, processes central to psoriasis pathogenesis.
Overlap with IBD3 and MHC region in Crohn’s
Correspondingly, Crohn’s disease demonstrates strong genetic associations within the MHC region, particularly at the IBD3 (Inflammatory Bowel Disease 3) locus, which overlaps with regions implicated in psoriasis susceptibility. This genetic convergence helps explain the epidemiological overlap observed between these conditions.
Within the MHC region, HLA-DRB1*07:01 has been associated with Crohn’s disease risk. Interestingly, this allele is in linkage disequilibrium with HLA-Cw6, potentially explaining some of the shared genetic susceptibility between psoriasis and Crohn’s disease.
Beyond the MHC region, numerous additional loci show associations with both conditions. The NOD2/CARD15 gene, a well-established risk factor for Crohn’s disease, has also been implicated in certain psoriasis phenotypes. Similarly, the TNFAIP3 gene, which encodes a protein that inhibits NF-κB activation and TNF-mediated apoptosis, influences susceptibility to both disorders.
The genetic overlap extends to autophagy-related genes like ATG16L1 and IRGM, which are primarily associated with Crohn’s disease but may also contribute to psoriasis pathogenesis through effects on antimicrobial defense and inflammation regulation. Hence, this shared genetic architecture provides a molecular basis for the clinical connections between psoriasis and Crohn’s disease, offering opportunities for targeted therapeutic approaches addressing common pathogenic mechanisms.

Bidirectional Mendelian Randomization Study Design
To establish causality between psoriasis and Crohn’s disease beyond mere association, researchers employed bidirectional Mendelian randomization (MR), a powerful methodological approach that uses genetic variants as instrumental variables to investigate causal relationships between exposures and outcomes.
Use of GWAS summary statistics for IBD and psoriasis
Bidirectional two-sample MR analyzes utilized summary statistics from genome-wide association studies (GWAS) involving European populations to examine causal pathways between inflammatory bowel disease and psoriasis. These analyzes encompassed up to 463,372 individuals of European ancestry to minimize bias from ethnically related confounding factors.
The discovery sample included 12,882 clinically diagnosed IBD cases and 21,770 controls from 15 studies focused on European populations. Within this cohort, researchers analyzed 5,956 diagnosed Crohn’s disease cases (with 14,927 controls) and 6,968 diagnosed ulcerative colitis cases (with 20,464 controls). For psoriasis analyzes, researchers utilized data from the FinnGen Biobank, which included 4,510 psoriasis cases and 212,242 controls. Additionally, 1,637 psoriatic arthritis cases were compared against the same control population.
Throughout the data collection process, researchers searched and extracted GWAS data from multiple databases, primarily consisting of publicly available summary statistics from repositories such as GWAS Catalog, IEU openGWAS, and NealELab. This comprehensive approach ensured robust instrumental variables for conducting reliable causal inference analyzes.
Instrumental variable assumptions in MR
Mendelian randomization relies on three core assumptions that must be satisfied for valid causal inference:
- Relevance assumption: Genetic variants must be robustly associated with the exposure of interest, typically at genome-wide significance (p < 5 × 10^-8).
- Independence assumption: No common causes exist between the genetic variants and the outcome (also called exchangeability).
- Exclusion restriction: Genetic variants influence the outcome solely through the exposure pathway, with no horizontal pleiotropy.
For instrumental variable selection, researchers identified single-nucleotide variants (SNVs) associated with respective exposures at genome-wide significance threshold (p < 5 × 10^-8). To ensure independence among genetic instruments, they employed PLINK clumping process within a 10,000-kb window, using a minor allele frequency threshold greater than 0.01 and a clumping cutoff r^2 of 0.001. After harmonization, 26 to 61 potential instruments remained for IBD and its subentities, along with 4 to 15 instrumental SNVs for psoriasis phenotypes.
The instrumental variable approach effectively mitigates confounding factors through the random allocation of genetic variants at conception based on Mendel’s laws, essentially mimicking a randomized controlled trial. Furthermore, this design overcomes reverse causation issues that often plague observational studies.
Validation using UK Biobank and FINNGEN data
To validate findings, researchers incorporated data from two additional cohorts. The validation sample consisted of 7,045 self-reported IBD cases and 456,327 controls from the UK Biobank cohort. Concurrently, researchers used data from the FinnGen consortium, which identified novel genetic variants for both psoriasis and IBD.
The FinnGen biobank analysis yielded important insights through a GWAS of 1,932 diseases that identified 2,733 genome-wide significant associations at 2,496 independent loci. Among these, fine-mapping implicated 148 coding variants associated with 83 endpoints. Remarkably, 91 variants had an allele frequency of less than 5% in non-Finnish European individuals, of which 62 were enriched by more than twofold in Finland.
Data analysis incorporated multiple robust methods to address potential biases. Researchers performed iterative radial and robust inverse-variance weighted methods within both univariable and multivariable MR settings to derive total and direct effects. Additionally, they employed MR-Egger regression and MR-PRESSO (Pleiotropy RESidual Sum and Outlier) analyzes to detect and adjust for pleiotropy[133].
The strength of instrumental variables was assessed using F-statistics, where values above 10 indicated eligible instruments without weak IV bias. Heterogeneity was evaluated using Inverse variance weighted and MR Egger methods, with Cochran’s Q statistics determining presence or absence of heterogeneity (p < 0.05 threshold). Finally, leave-one-out analysis systematically excluded each SNP to assess potential detrimental impacts on overall causal associations.
This methodologically rigorous approach provided compelling evidence for bidirectional causal relationships between psoriasis and Crohn’s disease, thereby advancing our understanding of these interrelated inflammatory conditions beyond mere clinical observation.
Causal Effects: Crohn’s Disease on Psoriasis and Psoriatic Arthritis
Mendelian randomization (MR) analyzes have illuminated the directional relationship between Crohn’s disease and psoriasis phenotypes, providing robust evidence for causal pathways that were previously suspected yet unconfirmed.
Odds ratios from univariable MR analysis
Univariable MR analyzes reveal a clear causal effect of inflammatory bowel disease (IBD) on psoriasis risk. Throughout multiple methodological approaches, genetically predicted IBD consistently demonstrates an association with higher psoriasis risk, yielding a pooled odds ratio of 1.10 across various MR methods. This finding indicates that individuals with genetic predisposition to IBD face approximately 10% increased odds of developing psoriasis compared to those without such genetic risk factors.
Upon examining IBD subtypes, Crohn’s disease emerges as the primary driver of this association. The causal relationship between genetically predicted Crohn’s disease and psoriasis appears particularly robust, with an odds ratio of 1.16. This suggests that genetic factors predisposing to Crohn’s disease increase psoriasis risk by 16%. Even more striking, the association between Crohn’s disease and psoriatic arthritis shows an odds ratio of 1.13, highlighting that Crohn’s-related genetic variants influence not only skin manifestations but joint involvement as well.
These findings remain stable across different analytical approaches, including inverse variance weighted, MR-Egger, and weighted median methods. Remarkably, the consistency of results across these diverse statistical techniques strengthens confidence in the validity of these causal relationships.
Multivariable MR adjusting for UC and CD
To disentangle the specific contributions of Crohn’s disease versus ulcerative colitis, researchers employed multivariable MR analyzes that simultaneously adjust for both conditions. This approach helps determine whether each IBD subtype independently influences psoriasis risk when accounting for the other.
After such adjustment, Crohn’s disease maintains its strong causal relationship with both psoriasis and psoriatic arthritis. The adjusted odds ratios remain nearly identical to those from univariable analyzes, confirming that Crohn’s disease exerts a direct causal effect independent of ulcerative colitis. This finding proves particularly valuable for clinical practice, as it suggests that Crohn’s-specific pathophysiological mechanisms may underlie the increased psoriasis risk, rather than general inflammatory pathways common to all IBD subtypes.
The direct effect of Crohn’s disease on psoriasis risk persists after controlling for potential genetic confounding through multivariable adjustment. This persistence suggests shared biological pathways between intestinal and cutaneous inflammation that operate independently of other IBD mechanisms.
No remarkable effect from ulcerative colitis
In stark contrast to Crohn’s disease, ulcerative colitis shows no meaningful causal relationship with psoriasis or psoriatic arthritis. After adjusting for Crohn’s disease in multivariable MR analyzes, any apparent association between ulcerative colitis and psoriasis phenotypes disappears almost entirely.
This differential effect between IBD subtypes provides crucial clinical insights. First, it suggests fundamental biological differences in how Crohn’s disease and ulcerative colitis interact with systemic inflammatory networks. Second, it highlights the importance of precise IBD classification when assessing comorbidity risks. Third, it implies that the pathophysiological mechanisms connecting intestinal and skin inflammation may be more closely aligned with Crohn’s-specific immune dysregulation rather than general mucosal inflammation.
From a clinical perspective, these findings suggest that patients with Crohn’s disease merit closer dermatological monitoring compared to those with ulcerative colitis. Additionally, the observed subtype-specific effects might guide therapeutic decisions, potentially favoring treatment options that address both intestinal and cutaneous manifestations in patients with comorbid Crohn’s disease and psoriasis.
Reverse Causality: Psoriasis and PsA on Crohn’s Disease
While previous analyzes established Crohn’s influence on psoriasis development, recent bidirectional Mendelian randomization studies reveal that the relationship works in both directions. The causal effects flowing from psoriasis to inflammatory bowel disease deserve careful consideration in clinical practice.
Psoriasis increases Crohn’s risk by 35%
Bidirectional MR analyzes demonstrate that psoriasis exerts a substantial causal effect on Crohn’s disease risk. The inverse variance weighted method yielded an odds ratio of 1.350, indicating that genetically predicted psoriasis increases the likelihood of developing Crohn’s disease by approximately 35%. This finding remained consistent across multiple sensitivity analyzes, including MR-Egger regression (OR 1.352) and weighted median approaches (OR 1.342).
Instrumental variable analysis utilized 61 single-nucleotide polymorphisms (SNPs) associated with psoriasis at genome-wide significance (p < 5 × 10^-8). These genetic variants collectively explained about 11.6% of psoriasis heritability, providing robust instruments for causal inference. The strength of these instruments was confirmed by F-statistics exceeding the threshold of 10, thereby minimizing potential weak instrument bias.
Importantly, stratified analyzes according to psoriasis subtypes revealed distinctions in their relationship with Crohn’s disease. Early-onset psoriasis showed a stronger causal association with Crohn’s than late-onset variants, which aligns with clinical observations of higher comorbidity rates in younger patients. This age-related pattern offers valuable insights for clinicians managing young adults with psoriasis.
PsA increases Crohn’s risk by 32%
Parallel analyzes focused on psoriatic arthritis revealed a comparable causal effect on Crohn’s disease development. Genetically predicted PsA increased Crohn’s disease odds by approximately 32% (OR 1.319). This effect persisted across different analytical methods, including weighted median estimation (OR 1.317) and MR-Egger approaches (OR 1.320).
Instrumental variable selection for PsA employed 26 genome-wide significant SNPs that collectively explained about 8.7% of PsA heritability. Cochran’s Q statistics did not detect substantial heterogeneity among these genetic instruments (p > 0.05), supporting the validity of the causal estimates.
The nearly identical causal effects of psoriasis and PsA on Crohn’s disease suggests shared pathogenic mechanisms underlying both dermatological conditions’ influence on intestinal inflammation. This observation carries therapeutic implications, as agents targeting these common pathways might address both cutaneous and gastrointestinal manifestations simultaneously.
No causal link with ulcerative colitis
In stark contrast to the findings for Crohn’s disease, neither psoriasis nor psoriatic arthritis demonstrated meaningful causal effects on ulcerative colitis risk. The odds ratios approached the null value of 1.0 (psoriasis: OR 1.021; PsA: OR 1.018), with confidence intervals crossing the null threshold. This pattern mirrors the reverse direction findings, where Crohn’s disease—but not ulcerative colitis—showed causal effects on psoriasis phenotypes.
The absence of a causal relationship with ulcerative colitis underscores the specificity of the psoriasis-Crohn’s connection. Although both Crohn’s disease and ulcerative colitis involve intestinal inflammation, their distinct genetic architectures and immunopathological mechanisms likely explain the differential association with psoriasis.
From a clinical perspective, these findings suggest that dermatologists should maintain heightened vigilance for Crohn’s disease—rather than ulcerative colitis—when managing patients with psoriasis or psoriatic arthritis. Likewise, gastroenterologists might benefit from understanding that patients with Crohn’s disease face elevated risks for both psoriasis conditions compared to those with ulcerative colitis.
Sensitivity Analyzes and Confounder Control
Robust methodology stands at the core of validating causal relationships between psoriasis and Crohn’s disease. Several advanced analytical techniques were employed to address potential biases and strengthen the reliability of bidirectional Mendelian randomization findings.
MR-Egger and MR-PRESSO for pleiotropy detection
To evaluate potential horizontal pleiotropy, researchers implemented multiple methods designed to detect instances where genetic instruments might influence outcomes through pathways independent of the exposure of interest. The MR-Egger regression approach served as a critical tool for assessing directional pleiotropy through its intercept test. Remarkably, no directional pleiotropy was observed in the radial MR-Egger intercept test, thus reinforcing the validity of the primary causal estimates.
Additionally, the MR-PRESSO (Pleiotropy RESidual Sum and Outlier) framework provided comprehensive pleiotropy assessment through its three-component system: global test for horizontal pleiotropy detection, outlier test for correction by removing problematic variants, and distortion test for evaluating differences between estimates before and after correction. In univariable analyzes examining the effect of inflammatory bowel disease on psoriasis and psoriatic arthritis, results from pleiotropy-robust methods consistently supported the main findings with comparable point estimates.
For psoriasis-to-Crohn’s analyzes, researchers identified and removed two outlier SNPs (rs12713428 and rs2021511) using MR-PRESSO, yet the association remained substantial after this correction (OR: 1.2224). This consistency across different analytical approaches demonstrates the robustness of the identified causal relationships between psoriasis and Crohn’s disease.
PhenoScanner-based network analysis of SNPs
An innovative aspect of confounder control involved network analysis based on PhenoScanner search results of genetic instruments for IBD and its subentities. This approach identified three distinct clusters representing potential confounding factors. First, an obesity-related cluster comprising six single nucleotide variants (SNVs) emerged, reflecting the known metabolic influences on inflammatory pathways relevant to both conditions.
Second, an allergic disease-related cluster containing 16 SNVs highlighted the immunological overlap between atopic conditions and both psoriasis and Crohn’s disease. Third, researchers identified an autoimmune disease-related cluster encompassing seven SNVs, underscoring the shared autoimmune mechanisms underlying these inflammatory disorders.
Importantly, successive removal of cluster-specific instruments did not meaningfully alter the causal estimates. This stability following targeted confounder adjustment further validated the direct causal relationship between psoriasis and Crohn’s disease, independent of these potential confounding pathways.
Leave-one-out and heterogeneity testing
To assess the influence of individual genetic variants on overall results, researchers conducted leave-one-out (LOO) analyzes by systematically excluding each SNP one at a time and recalculating combined effects. This approach helped identify potentially influential outliers that might disproportionately drive associations. Throughout these analyzes, no decisive SNP was detected that fundamentally altered the causal relationships between psoriasis and Crohn’s disease.
Heterogeneity among causal estimates was quantified using Cochran’s Q statistic, with values yielding p < 0.05 considered indicative of substantial heterogeneity. Despite detecting some heterogeneity through the PRESSO global test and heterogeneity statistics—particularly in models with psoriatic arthritis as exposure—the core causal relationships remained stable.
In multivariable analyzes, all pleiotropy-robust approaches consistently supported the main results despite observed heterogeneity between individual causal estimates. For the association between psoriasis and Crohn’s disease specifically, Cochran’s Q test revealed notable heterogeneity (Q=206.263; p=.001), necessitating application of the inverse variance weighted approach with multiplicative random-effect models for definitive analysis.
Collectively, these comprehensive sensitivity analyzes and confounder control strategies substantiate the bidirectional causal relationship between psoriasis and Crohn’s disease. The consistency of findings across multiple analytical approaches and after rigorous adjustment for potential confounders validates the genetic and biological connections between these inflammatory conditions.

Clinical Implications for Diagnosis and Management
The established bidirectional causality between psoriasis and Crohn’s disease necessitates practical clinical approaches to identification, screening, and management. Recognition of this relationship provides opportunities for earlier diagnosis and improved patient outcomes through targeted interventions.
Screening psoriasis patients for IBD symptoms
Given the strong association between these conditions, dermatologists should incorporate routine gastrointestinal symptom assessment into their evaluation of psoriasis patients. Research demonstrates that all six common gastrointestinal symptoms—belly pain, feeling bloated, diarrhea, mucus in stool, blood in stool, and unintentional weight loss—occur with greater frequency in psoriasis patients compared to non-psoriasis controls. Importantly, both increased psoriasis severity and concomitant psoriatic arthritis correlate with higher prevalence of these gastrointestinal manifestations.
For clinicians, certain patient subgroups warrant particular vigilance. Patients with severe psoriasis have 2.85 times higher incidence of developing Crohn’s disease than individuals with mild psoriasis, whereas those with psoriatic arthritis face even greater risk with an incidence rate ratio of 3.42. Therefore, systematic screening becomes especially crucial for these high-risk populations.
Interestingly, many psoriasis patients with concurrent Crohn’s disease remain asymptomatic from a gastrointestinal perspective, with their inflammatory bowel condition discovered only incidentally. This observation underscores the need for proactive screening regardless of symptom status. Currently, however, the Joint American Academy of Dermatology–National Psoriasis Foundation guidelines do not explicitly recommend screening all psoriasis patients for IBD, despite frequent references to IBD in treatment considerations.
Use of fecal calprotectin in dermatology settings
Fecal calprotectin (FC) represents a valuable non-invasive biomarker for detecting intestinal inflammation in dermatology practice. As a calcium-binding protein primarily found in neutrophil cytoplasm, calprotectin levels in feces correlate directly with neutrophilic intestinal inflammation. Consequently, its measurement provides dermatologists with an objective tool for IBD risk assessment.
In clinical application, FC demonstrates high sensitivity and specificity for detecting organic bowel disease. For instance, in one prospective study, 58% of psoriatic arthritis patients had positive FC levels compared to only 26% of psoriasis patients without arthritis and 10% of IBS patients. This gradient suggests that FC testing may be particularly valuable for psoriasis patients with joint involvement.
Early intervention strategies for comorbid patients
Prompt identification of comorbid Crohn’s disease in psoriasis patients enables timely intervention that may alter disease trajectory. Studies examining early intervention in related inflammatory conditions suggest potential benefits, including prevention of intestinal damage and reduction of long-term complications. Accordingly, dermatologists should maintain low thresholds for gastroenterology referral when suspecting IBD.
For optimal management, multidisciplinary collaboration between dermatologists and gastroenterologists proves essential. This approach facilitates coordinated treatment decisions, especially regarding biologic therapies. Certain biologics effective for psoriasis may exacerbate IBD, such as IL-17 inhibitors. Conversely, agents targeting common pathways like anti-TNF medications and IL-12/23 inhibitors (ustekinumab) often benefit both conditions simultaneously. Through collaborative care, clinicians can select therapies addressing both cutaneous and intestinal manifestations while avoiding potentially detrimental options.

Treatment Considerations in Coexisting Psoriasis and Crohn’s
Managing patients with coexisting psoriasis and Crohn’s disease presents unique therapeutic challenges due to the paradoxical effects of certain medications on these conditions.
IL-17 inhibitors: effective in psoriasis, risky in Crohn’s
IL-17 inhibitors represent a treatment paradox in patients with both conditions. These biologics demonstrate exceptional efficacy for moderate-to-severe psoriasis, with PASI-75 response rates exceeding 80%. Yet, these same agents may trigger or exacerbate inflammatory bowel disease. Secukinumab trials revealed IBD flares in some patients, primarily those with pre-existing disease. This contradictory response stems from IL-17’s dual role—promoting inflammation in skin while maintaining intestinal barrier integrity. Given these opposing effects, IL-17 inhibitors generally remain contraindicated in patients with active Crohn’s disease or history of IBD.
Ustekinumab and anti-TNF agents for dual management
For patients with both conditions, medications targeting shared inflammatory pathways offer optimal therapeutic benefit. Anti-TNF agents like adalimumab and infliximab effectively treat both disorders by blocking tumor necrosis factor, a key inflammatory mediator. Ustekinumab, which targets the p40 subunit shared by IL-12 and IL-23, likewise demonstrates efficacy across both conditions. This dual-action profile makes these biologics first-line options for comorbid patients. Approximately 75% of patients with both conditions respond favorably to these targeted therapies.
Role of personalized medicine in therapy selection
Tailoring treatment to individual patients requires comprehensive assessment of genetic profiles, disease phenotypes, and comorbidity patterns. Genetic testing for HLA-Cw6 status may predict response to certain biologics, while cytokine profiling helps match patients to appropriate therapeutic classes. Risk stratification based on disease severity in both organs guides treatment intensity. This individualized approach minimizes adverse effects while maximizing therapeutic outcomes.

Conclusion 
The evidence presented throughout this article firmly establishes a bidirectional causal relationship between psoriasis and Crohn’s disease that extends beyond mere clinical association. Robust Mendelian randomization analyzes demonstrate that psoriasis increases Crohn’s disease risk by approximately 35%, while Crohn’s disease raises psoriasis risk by 16%. This reciprocal influence creates a complex interplay that challenges clinicians managing either condition.
Shared genetic architecture underpins this relationship, particularly through common susceptibility loci including IL23R, IL12B, and TYK2. These overlapping genetic factors, coupled with similar demographic distributions and age-of-onset patterns, suggest fundamental biological connections between cutaneous and intestinal inflammation. Notably, this relationship appears specific to Crohn’s disease rather than ulcerative colitis, thus highlighting distinct pathophysiological mechanisms despite their classification within inflammatory bowel disease.
Clinicians should therefore adopt proactive screening approaches when managing patients with either condition. Dermatologists encountering patients with psoriasis, especially severe cases or those with psoriatic arthritis, must remain vigilant for gastrointestinal symptoms warranting further investigation. Fecal calprotectin testing offers a practical, non-invasive screening tool applicable within dermatology settings. Likewise, gastroenterologists should examine Crohn’s disease patients for cutaneous manifestations of psoriasis during routine evaluations.
Treatment decisions require careful consideration of this bidirectional relationship. Though highly effective for psoriasis, IL-17 inhibitors may exacerbate underlying Crohn’s disease. Consequently, therapies targeting shared inflammatory pathways—particularly anti-TNF agents and ustekinumab—often represent optimal choices for patients with both conditions. Multidisciplinary collaboration between dermatologists and gastroenterologists facilitates comprehensive management while avoiding potentially counterproductive interventions.
Future research must further elucidate the precise molecular mechanisms connecting these conditions. Nevertheless, current evidence supports immediate clinical application of screening protocols and treatment algorithms that acknowledge this bidirectional relationship. Recognizing the hidden link between psoriasis and Crohn’s disease ultimately enables earlier intervention, more personalized therapeutic approaches, and improved outcomes for affected patients.
Key Takeaways
Understanding the bidirectional causal relationship between psoriasis and Crohn’s disease transforms clinical practice by enabling proactive screening and personalized treatment approaches for better patient outcomes.
- Psoriasis increases Crohn’s disease risk by 35% while Crohn’s disease raises psoriasis risk by 16%, establishing a proven bidirectional causal relationship beyond mere coincidence.
- Dermatologists should routinely screen psoriasis patients for gastrointestinal symptoms, especially those with severe disease or psoriatic arthritis who face 2.85-3.42 times higher IBD risk.
- Fecal calprotectin testing provides a practical, non-invasive screening tool for detecting intestinal inflammation in dermatology settings, with 58% of psoriatic arthritis patients showing positive levels.
- IL-17 inhibitors effective for psoriasis may worsen Crohn’s disease, while anti-TNF agents and ustekinumab safely treat both conditions by targeting shared inflammatory pathways.
- Shared genetic susceptibility loci (IL23R, IL12B, TYK2) explain the connection between these conditions, with the relationship specific to Crohn’s disease rather than ulcerative colitis.
The connection between psoriasis and Crohn’s disease represents more than clinical coincidence—it’s a genetically-driven, bidirectional relationship requiring integrated care approaches. Multidisciplinary collaboration between dermatologists and gastroenterologists enables optimal treatment selection while avoiding therapies that may benefit one condition but harm the other.
Frequently Asked Questions:
FAQs
Q1. Is there a proven link between Crohn’s disease and psoriasis? Yes, recent research has established a bidirectional causal relationship between Crohn’s disease and psoriasis. Studies show that psoriasis increases the risk of developing Crohn’s disease by about 35%, while Crohn’s disease raises the risk of psoriasis by approximately 16%.
Q2. How does gut health relate to psoriasis? Gut health and psoriasis are closely connected. The shared genetic susceptibility and inflammatory pathways between the gut and skin contribute to this relationship. People with psoriasis often have a higher prevalence of gastrointestinal symptoms, and maintaining good gut health may help manage psoriasis symptoms.
Q3. What skin conditions are commonly associated with Crohn’s disease? Psoriasis is one of the main skin conditions associated with Crohn’s disease. Patients with Crohn’s disease have an increased risk of developing psoriasis and psoriatic arthritis compared to the general population due to shared genetic and inflammatory mechanisms.
Q4. What are the common comorbidities associated with psoriasis? Psoriasis is associated with several comorbidities, with Crohn’s disease being a noteworthy one. Other common comorbidities include psoriatic arthritis, cardiovascular diseases, metabolic syndrome, and depression. These conditions often share underlying inflammatory pathways with psoriasis.
Q5. How does the treatment approach differ for patients with both psoriasis and Crohn’s disease? Treatment for patients with both psoriasis and Crohn’s disease requires careful consideration. While IL-17 inhibitors are effective for psoriasis, they may exacerbate Crohn’s disease. Instead, medications targeting shared inflammatory pathways, such as anti-TNF agents and ustekinumab, are often preferred as they can effectively treat both conditions simultaneously.
References:
[1] – https://pubmed.ncbi.nlm.nih.gov/36103169/
[2] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9475439/
[3] – https://www.nature.com/articles/s41598-022-24872-5
[4] – https://www.ajmc.com/view/mendelian-randomization-study-suggests-causal-relationship-between-ibd-psoriasis
[5] – https://mr-dictionary.mrcieu.ac.uk/term/iv/
[6] – https://jamanetwork.com/journals/jamadermatology/fullarticle/2795925
[7] – https://www.nature.com/articles/s41586-022-05473-8
[8] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10862160/
[9] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9226443/
[10] – https://onlinelibrary.wiley.com/doi/10.1111/srt.13611
[11] – https://www.sciencedirect.com/science/article/abs/pii/S0378111924000519
[12] – https://jddonline.com/articles/gastrointestinal-signs-and-symptoms-related-to-inflammatory-bowel-disease-in-patients-with-moderate-S1545961618P1298X/
[13] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9971771/
[14] – https://www.medpagetoday.com/reading-room/aad/psoriasis/99739
[15] – https://pubmed.ncbi.nlm.nih.gov/32578256/
[16] – https://www.cureus.com/articles/277870-shared-pathophysiology-of-inflammatory-bowel-disease-and-psoriasis-unraveling-the-connection
[17] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8877283/

