Ketogenic Diets in Neurology and Endocrinology: Friend or Fad?

Abstract
The ketogenic diet (KD), defined by a high fat, moderate protein, and very low carbohydrate composition, has undergone a notable resurgence in both clinical practice and popular health discourse. Initially introduced in the 1920s as a therapeutic approach for refractory pediatric epilepsy, its clinical utility has since broadened considerably. Today, ketogenic diets are being investigated not only for weight management and type 2 diabetes but also for their potential in addressing neurological and endocrinological disorders, including neurodegenerative diseases and hormonal imbalances.
This review critically evaluates the current body of evidence supporting ketogenic diets across these domains, with particular attention to therapeutic mechanisms, efficacy, safety, and implementation challenges. In neurology, systematic reviews and clinical trials consistently demonstrate that ketogenic diets reduce seizure frequency and, in some cases, improve cognitive and behavioral outcomes. However, evidence on their impact on quality of life, psychosocial well-being, and growth parameters in pediatric populations remains inconclusive, highlighting the need for long-term follow-up studies [1] [2]. Emerging research also suggests potential neuroprotective effects in conditions such as Alzheimer’s disease, Parkinson’s disease, and traumatic brain injury, although these findings are still preliminary and require validation in large-scale randomized controlled trials.
In endocrinology, a substantial body of meta-analyses and randomized studies supports the role of ketogenic diets in improving glycemic control. Reported benefits include marked reductions in fasting blood glucose and glycated hemoglobin (HbA1c), along with favorable effects on insulin resistance and weight regulation [3]. Beyond diabetes, there is growing evidence that ketogenic diets may influence reproductive endocrinology by modulating sex hormones, improving polycystic ovary syndrome (PCOS) outcomes, and impacting thyroid and adrenal function [4] [5]. Despite these promising findings, questions persist regarding long-term adherence, sustainability, and the potential for adverse effects such as dyslipidemia, micronutrient deficiencies, and gastrointestinal complications.
A key point of contention is whether ketogenic diets provide superior clinical outcomes compared to established dietary interventions such as the Mediterranean or DASH diets, which are supported by robust long-term safety and efficacy data. Conflicting results from clinical studies contribute to ongoing uncertainty among healthcare providers, making it difficult to establish standardized guidelines for ketogenic diet use outside specific indications such as refractory epilepsy [6] [7].
This review synthesizes available evidence to present a balanced perspective on the therapeutic potential of ketogenic diets within neurological and endocrinological practice. By examining mechanisms of action, clinical efficacy, safety considerations, and barriers to implementation, it aims to clarify whether ketogenic diets should be viewed as legitimate metabolic therapies or as transient dietary trends. Ongoing large-scale, long-term studies will be critical in determining their place within evidence-based medicine.
Keywords: ketogenic diet, epilepsy, diabetes, neurological disorders, endocrine function, metabolic therapy
Introduction
The ketogenic diet stands at a fascinating crossroads between established medical therapy and contemporary dietary phenomenon. Having been used to treat epilepsy for 100 years, the ketogenic diet is a high-fat, low-carbohydrate, sufficient-protein diet that mimics metabolic changes occurring during starvation [8]. Previously seen as an “alternative” treatment of last resort, ketogenic diets have emerged as important therapeutic options for children with intractable epilepsy and have become more frequently used worldwide [9] [10].
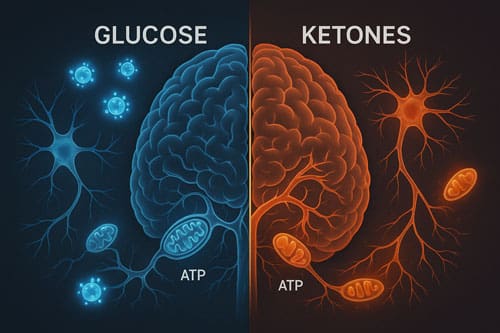
The fundamental premise of ketogenic diets lies in their ability to induce ketosis, a metabolic state where ketone bodies partly replace glucose as fuel during marked alterations in brain energy metabolism [11]. Under normal physiological conditions, the brain primarily utilizes glucose for ATP generation, but during glucose scarcity, ketone bodies become an important energy source [12] [13]. This metabolic shift has profound implications for both neurological and endocrinological function.
Recent decades have witnessed an explosion of interest in ketogenic diets beyond epilepsy treatment. Such low-carbohydrate, ketogenic diets were employed to treat obesity and diabetes in the 19th and early 20th centuries, with recent clinical research reinvigorating their use for individuals with obesity and diabetes [14] [15]. Simultaneously, enthusiasm has increased in the scientific community due to evidence that ketogenic diets reduce pathology and improve outcomes in animal models of neurodegenerative disorders, including multiple sclerosis, stroke, Parkinson’s disease, and Alzheimer’s disease [16].
However, this renewed interest has generated interesting debate. Diets have been at the center of animated debates for decades with many claims made by supporters of opposite camps, often with limited evidence, with the ketogenic diet generating particular interest with many taking pro and con positions [17] [18] [19]. The most appropriate type of diets to maintain or lose body weight over medium to long term has been a matter of controversy and debates for more than half a century [20].
This analytical review seeks to examine whether ketogenic diets represent evidence-based therapeutic interventions or merely reflect contemporary dietary trends. By critically evaluating current evidence across neurological and endocrinological applications, we aim to provide clinicians, researchers, and patients with a balanced perspective on the legitimate therapeutic potential and limitations of ketogenic dietary interventions.
Research Questions
This review addresses several key questions:
- What is the current evidence for ketogenic diet efficacy in neurological conditions beyond epilepsy?
- How do ketogenic diets affect endocrine function and metabolic parameters in clinical populations?
- What are the established mechanisms of action underlying ketogenic diet effects?
- What safety considerations and contraindications must be weighed in clinical implementation?
- How do short-term benefits translate to long-term outcomes and sustainability?
Background and Historical Context
Origins in Clinical Medicine
The ketogenic diet was first developed in the 1920s, created to mimic the biochemical environment that would ensue during periods of limited food availability [21]. Although the ketogenic diet has been used in therapy for epilepsy for more than 50 years, there are few studies concerned with the effects of this diet on the central nervous system [22]. The initial clinical application emerged from observations that fasting could reduce seizure frequency, leading clinicians to develop a sustainable dietary approach that could maintain the metabolic benefits of starvation.
The ketogenic diet has been in use since the 1920s as therapy for epilepsy, and since the 1960s has also become widely known as one of the methods for obesity treatment [23]. However, with the advent of effective antiepileptic medications in the mid-20th century, ketogenic diet use declined notably until its resurgence in recent decades.
Defining Ketogenic Diets
Ketogenic diet therapies are high-fat, low-carbohydrate diets designed to mimic a fasting state [24] [25]. The ketogenic diet is a high-fat, low-carbohydrate diet used to treat drug-resistant seizures, especially in children [26] [27]. Classical formulations typically consist of a 4:1 or 3:1 ratio of fats to carbohydrates and proteins combined, with about 90% of calories in a 4:1 ketogenic diet coming from fat [28].
Several variations have been developed:
- Classical Ketogenic Diet (CKD): The traditional high-fat, very low-carbohydrate approach
- Medium-Chain Triglyceride (MCT) Diet: Incorporates MCT oils to enhance ketone production
- Modified Atkins Diet (MAD): A modified counterpart that has gained ground to increase palatability and adherence [29]
- Low Glycemic Index Treatment (LGIT): Based on maintaining stable blood sugar levels with low-carbohydrate composition designed to minimize blood sugar spikes, proven effective as an antiepileptic intervention in children with intractable epilepsy [30]
Mechanisms of Action
Neurological Mechanisms
The precise mechanisms underlying ketogenic diet effects in neurological conditions remain incompletely understood, with multiple pathways likely contributing to therapeutic benefits.
Ketone Body Utilization
A key mechanism is the generation of ketones, which provide brain cells (neurons and astrocytes) with an energy source that is more efficient than glucose, resulting in beneficial downstream metabolic changes such as increasing adenosine levels [31]. Once blood concentration of ketone bodies reaches 2-4 mM, these metabolic substrates can provide as much as 70% of brain energy demand [32].
The brain’s utilization of ketones depends mainly on blood concentration, with many dietary approaches such as ketogenic diets, ketogenic medium-chain fatty acids, or exogenous ketones facilitating notable changes in brain metabolism [33] [34]. Glucose functions span beyond its role as energy substrate, and in most functions glucose is irreplaceable, with ketone bodies acting as supplementary fuel that may free up glucose for other crucial functions [35].
Neurotransmitter Effects
The ketogenic diet may alter brain handling of glutamate, the major excitatory neurotransmitter, with ketone body metabolism furnishing as much as 30% of glutamate and glutamine carbon and relatively more glutamate becoming available to glutamate decarboxylase reaction, which increases brain GABA [36] [37]. Ketosis also increases brain GABA by increasing brain metabolism of acetate, which glia convert to glutamine that GABA-ergic neurons readily take up and use as a precursor to GABA [38].
Mitochondrial and Metabolic Effects
Studies have shown that medium-chain fatty acids directly inhibit AMPA receptors (glutamate receptors) and change cell energetics through mitochondrial biogenesis, with medium-chain fatty acids rather than ketones likely blocking seizure onset and raising seizure threshold [39]. Ketosis alters crucial aspects of brain biochemistry, including a positive effect on energy charge [40].
Endocrinological Mechanisms
Hormonal Alterations
The ketogenic diet causes a decrease in insulin (more consistent finding) and may increase serum leptin levels, with the finding that ketogenic diets can concurrently increase leptin and decrease insulin being unique, and also affects other peripherally released hormones including ghrelin and cortisol [41] [42] [43].
Changes in caloric composition and metabolism alter neurohormones participating in energy homeostasis regulation, with observed changes including increased serum leptin and decreased serum insulin, opposing changes unique compared to other metabolic stimuli that may modify activity of several cell signaling cascades including PI3K, AMPK, and mTOR [44].
Metabolic Pathway Modifications
Reducing carbohydrate intake to typically below 50g per day leads to increased ketogenesis to provide body fuel, with such low-carbohydrate, ketogenic diets employed to treat obesity and diabetes in the 19th and early 20th centuries [45]. The ketogenic diet decreases liver glycogen content and promotes gluconeogenesis while increasing lipid oxidation and reducing de novo lipogenesis, though hepatic lipid content still inevitably increases [46] [47].
Clinical Applications in Neurology
Epilepsy: The Established Application
Pediatric Epilepsy
Approximately 30% of patients with epilepsy have drug-resistant epilepsy (DRE), with the ketogenic diet considered an effective alternative treatment for epileptic patients [48]. Overall, positive effects of ketogenic diet therapy for epilepsy on seizure frequency reduction, as well as cognition and behavior were observed [49] [50].
Depending on patient compliance and comorbidities, all variations of the ketogenic diet were found helpful for seizure treatment, whether as additive or alternative treatment option, for children and adolescents with epilepsy [51]. In correctly qualified patients, seizure activity may be reduced by over 90% or even abolished for long periods after the diet is stopped [52].
Adult Epilepsy
Most clinical trials for drug-resistant epilepsy management in children and adults have been conducted over the last 3 decades, with ketogenic diets offering promising new adjunctive strategies in critical care settings for acute status epilepticus resolution when traditional antiseizure drugs and anesthetic agents fail [53].
Emerging Neurological Applications
Neurodegenerative Diseases
Ketogenic approaches may ameliorate the energy crisis in neurodegenerative diseases characterized by deterioration of brain glucose metabolism, providing therapeutic advantage, with most clinical studies examining neuroprotective roles conducted in patients with Alzheimer’s disease where brain imaging studies support enhancing brain energy metabolism with ketones [54].
Evidence shows ketogenic diets reduce pathology and improve outcome measures in animal models of multiple sclerosis, stroke, glaucoma, spinal cord injury, retinal degenerations, Parkinson’s disease and Alzheimer’s disease, with clinical trials suggesting improved quality of life in patients with multiple sclerosis and Alzheimer’s disease [55].
Cognitive Function
Higher cognitive functions require large-scale interactions across prefrontal cortical and hippocampal networks, with reduced ability to utilize glucose for energy metabolism shared by prefrontal cortex and hippocampus, suggesting therapeutic strategies bypassing neuronal glycolysis need may be beneficial for treating cognitive aging, with ketogenic diet used as global metabolic strategy for improving brain function [56].
Data suggest ketogenic diets could be optimal for enhancing large-scale network function critical for higher cognition [57].
Clinical Applications in Endocrinology
Type 2 Diabetes Management
Glycemic Control
Meta-analytic findings show remarkable effect of ketogenic diet compared to controls in terms of weight reduction, glycemic control, and improved lipid profile, with noticeable improvement in glycated hemoglobin (HbA1c) and high-density lipoprotein (HDL), concluding that ketogenic diet is superior to controls and results significant enough to recommend as adjunctive treatment for type 2 diabetes [58].
After ketogenic diet intervention, fasting blood glucose decreased by 1.29 mmol/L on average and glycated hemoglobin A1c by 1.07 [59]. Ketogenic diets result in improved HbA1c after 3 weeks, with effects persisting for at least 1 year, associated with reduction in glucose-lowering medications [60].
Weight Management
In overweight or obese patients newly diagnosed as type 2 diabetes mellitus, periodic ketogenic diet can control body weight and blood glucose and lipid, though long-term persistence is difficult [61] [62]. Evidence suggests very-low-calorie ketogenic diets effective in achieving rapid and noteworthy weight loss through easily reversible intervention, with muscle mass and strength preserved and preliminary studies suggesting potential as game-changer in type 2 diabetes management [63] [64].
Type 1 Diabetes Considerations
The jury remains out on whether low-carbohydrate, ketosis-inducing diet is effective and safe adjunctive therapy to insulin in type 1 diabetes, with limited published literature reporting association with weight loss and improved glycemic control but attendant increased risk of dyslipidemia, diabetic ketoacidosis, and hypoglycemia warranting caution and close monitoring [65] [66].
Case studies show diabetes-related biomarkers saw massive improvements ending up in official non-diabetic range, with total daily insulin requirements dropping by 70%, and diabetes-related biomarkers such as HbA1c being main risk factors for developing complications in diabetics [67] [68].
Hormonal and Reproductive Effects
Polycystic Ovary Syndrome (PCOS)
Short-term ketogenic diet potentially improved hormonal imbalances commonly associated with PCOS [69]. Research suggests ketogenic interventions may benefit reproductive hormone profiles in women with metabolic dysfunction.
Stress Hormones
Adipose tissue is considered an endocrine organ with excess compromising immune response and hormone metabolism, with visceral fat accumulation helping increase cortisol synthesis, involving hypothalamus-pituitary-adrenal (HPA) axis as neuroendocrine system maintaining homeostasis, with caloric restriction being valid strategy to reduce visceral adipose tissue in obesity [70] [71].
Low-carbohydrate diets may have endocrine effects on men’s testosterone and cortisol, though individual studies are conflicting [72]. Evidence suggests ketogenic diets could decrease total testosterone levels, with combination of ketogenic diet and physical activity markedly reducing body weight and increasing levels of LDL-C and cortisol [73].
Safety Profile and Contraindications
Short-term Side Effects
During ketogenic diet initiation phase, common side effects include vomiting, hypoglycemia, metabolic acidosis and diet refusal, with side effects while on diet involving gastrointestinal, hepatic, cardiovascular, renal, dermatological, hematologic and bone systems [74].
The most common early-onset complication was dehydration, especially in patients who started with initial fasting, with gastrointestinal disturbances such as nausea/vomiting, diarrhea, and constipation frequently noted, sometimes associated with gastritis and fat intolerance, and other early-onset complications including hypertriglyceridemia, transient hyperuricemia, hypercholesterolemia, infectious diseases, symptomatic hypoglycemia, hypoproteinemia, hypomagnesemia, repetitive hyponatremia [75].
Long-term Considerations
Some rare and serious side effects reported include pancreatitis, protein-losing enteropathy, prolonged QT interval, cardiomyopathy and changes in basal ganglia, with these serious complications potentially needing advanced work-up and immediate diet cessation [76].
Due to unbalanced ratio of lipids, carbohydrates and proteins, clinical evaluation of possible side effects with strict evaluation of growth and nutritional status is essential in patients following long-term restrictive diet, with possible long-term impact on growth and nutritional status not yet fully understood, especially when started in pediatric age [77] [78].
Cardiovascular Considerations
The ketogenic diet is not better for long-term effects compared to other dietary patterns, with low-carb pattern seeming more beneficial than very low-carbohydrate in terms of cardiovascular mortality, and other safety concerns should be taken into consideration when conducting future research [79] [80].
Intense debate surrounds use of low-carbohydrate, ketogenic diets for weight loss and cardiovascular disease avoidance, with case made that ketone bodies are more potent than glucose in bringing about protein modifications to which harmful effects of glucose have been attributed, suggesting attempts to minimize such modifications through nutritional ketosis are futile and may lead to adverse health outcomes [81] [82] [83].
Quality of Life and Adherence
Ketogenic diet was practiced mostly for one to six months, making it short-term solution to weight loss, with different symptoms and side effects occurring with varying intensities especially in first few days, though overall ketogenic diet did not affect quality of life and yielded very positive overall experience [84].
Significant weight loss was observed without adverse metabolic changes, reducing body fat without affecting muscle or bone mass, with quality of life improved and fatigue symptoms in subjects with overweight decreased [85].
Current Controversies and Debates
Evidence Quality and Study Limitations
Very few randomized clinical trials involving diets have addressed the combined question of weight loss and cardiovascular outcomes, with the ketogenic diet generating flurry of interest with many taking pro position and as many taking cons position [86].
Rates of obesity and diabetes rose markedly during periods of dietary guidelines focusing on reducing saturated and total fat, with ketogenic diets receiving substantial attention from general public and nutrition research community, though these very-low-carbohydrate diets with fat comprising >70% of calories have been dismissed as fads despite having long history in clinical medicine and human evolution [87] [88].
Clinical Practice Integration
Recommendations regarding ketogenic diet in clinical practice are often hindered by lack of established definition preventing capacity to be most appropriately prescribed as therapeutic option for diabetes, with conflicted evidence leading to uncertainty amongst clinicians on how best to support and advise patients [89].
The ketogenic diet might not be appropriate intervention for every individual, with number of contraindications proposed and deeply rooted into clinical practice, excluding many patients that could benefit from use, though many concerns were expressed due to absence of clinical studies conducted on fragile populations, with assessment of emerged evidence relative to safety currently lacking and much needed, requiring patient-to-patient basis assessment by adequately skilled medical doctors [90].
Long-term Sustainability
The most appropriate type of diets to maintain or lose body weight over medium to long term has been matter of controversy and debates for more than half a century, with both voluntary and coercive food restriction resulting in negative energy and macronutrient balance not designed to be maintained long term, contrasted with classical traditional alimentation consumed ad lib providing appropriate nutritional density and being appropriate for long-term use [91].
It is hard to imagine debate more animated and scientifically weaker than any debate centered around diets, with ketogenic diet possibly having some merits but excessive fervor with which it is often defended making it appear as another fad, with paucity of scientifically rigorous trials rendering debate over diets tentative, confusing, very opinionated and at times bitter [92].

Comparative Effectiveness
Versus Other Dietary Approaches
Based on evidence reviewed, low-carbohydrate and very-low-carbohydrate diets are not superior to other dietary approaches for weight loss, though these diets may have advantages related to appetite control, triglyceride reduction, and reduction in use of medication in T2D management [93].
Ketogenic diets appear to be more effective than low-fat diets for treatment of obesity and diabetes, with chronic ketosis potentially conferring unique metabolic benefits of relevance to cancer, neurodegenerative conditions, and other diseases associated with insulin resistance [94].
Mediterranean Diet Comparison
HbA1c values were not different between diet phases after 12 weeks, but improved from baseline on both diets, likely due to several shared dietary aspects [95]. There is still scarce evidence comparing ketogenic to Mediterranean diet, with other safety concerns in cardiovascular patients such as adverse events related to ketosis, fat-free mass loss, or potential pharmacological interactions needing consideration in future research [96].
Implementation Considerations
Clinical Monitoring
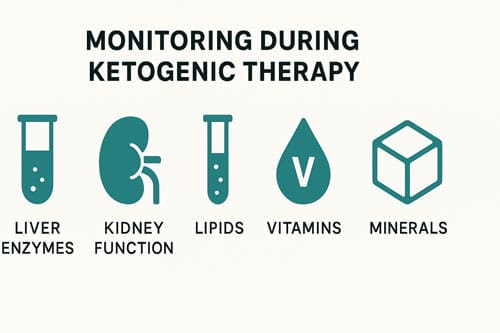
Many common side effects can be tackled easily with careful monitoring including blood counts, liver enzymes, renal function tests, urinalysis, vitamin levels, mineral levels, lipid profiles, and serum carnitine levels, with appropriate monitoring and close follow-up to minimize adverse effects allowing ketogenic diets to be effective for patients with intractable conditions [97] [98].
The prophylactic use of micronutrients supplementation should be considered before starting any ketogenic diet [99].
Patient Selection
This metabolic therapy is increasingly considered due to unique mechanisms and turns out to be powerful tool in hands of skillful team, though despite decades of extensive research to explain mechanism of efficacy, precise mechanism of action is still largely unknown, with fundamental change occurring regarding method of energy production that causes alterations in numerous biochemical pathways, thus restoring energetic and metabolic homeostasis of brain [100] [101].
Based on available evidence, a well-formulated ketogenic diet does not appear to have major safety concerns for the general public and can be considered a first-line approach for obesity and diabetes [102].
Future Directions and Research Needs
Mechanistic Understanding
A number of possible mechanisms of action have been proposed to explain anticonvulsant effects of the diet, with four hypothetical mechanisms discussed: the pH hypothesis, the metabolic hypotheses, the amino acid hypothesis, and the ketone hypothesis [103].
The microbes and metabolites identified may contribute to therapeutic effect of ketogenic diet in children with drug-resistant epilepsy, with several metabolites (e.g., plasmalogens) playing important roles in neurobiology and potentially influencing seizures, suggesting anti-seizure therapeutic strategies could be developed involving targeted manipulation of gut microbiota and/or its metabolites [104].
Long-term Outcome Studies
It would be useful to determine whether diet produces any neurophysiological effects that could account for some or all of its antiseizure properties, with efficacy of diet being impressive, and continued study of therapy which seems to work so well potentially giving valuable clues as to mechanism of seizures and their control, with further investigations into mechanism of action being encouraged [105] [106].
Personalized Medicine Approaches
Ketogenic dietary strategies may play role in short-term improvement of important metabolic parameters with potential for long-term benefit, however response may vary due to inter-individual ability to maintain long-term carbohydrate restriction [107].
Discussion
The evidence regarding ketogenic diets in neurology and endocrinology presents a complex picture that defies simple categorization as either “friend” or “fad.” The analysis reveals substantial therapeutic potential alongside limitations and ongoing controversies.
Neurological Applications: Established Benefits with Expanding Horizons
In neurology, the evidence base is most robust for pediatric epilepsy management. Systematic reviews consistently demonstrate positive effects on seizure frequency reduction, cognition, and behavior, with evidence indicating ketogenic diet therapy is safe [108] [109] [110]. The expansion beyond epilepsy into neurodegenerative conditions shows promise, though clinical evidence remains preliminary compared to the extensive preclinical data.
The mechanistic understanding, while incomplete, provides plausible explanations for therapeutic effects. Evidence suggests ketogenic diets cause effects on intermediary metabolism that influence dynamics of major inhibitory and excitatory neurotransmitter systems in brain, with the pattern of protection in animal models being distinct from other anticonvulsants, suggesting unique mechanism of action [111].
Endocrinological Applications: Promising but Complex
In endocrinology, ketogenic diets demonstrate clear short-term benefits for glycemic control and weight management. Meta-analyses conclude ketogenic diets are superior to controls in terms of glycemic control and lipid profile improvements, with results significant enough to recommend as adjunctive treatment for type 2 diabetes [112] [113]. However, concerns remain about safety in type 1 diabetes, with increased risks of dyslipidemia, diabetic ketoacidosis, and hypoglycemia warranting caution [114].
The hormonal effects of ketogenic diets reveal complexity that extends beyond simple glucose control. The unique finding that ketogenic diets can concurrently increase leptin and decrease insulin, opposing changes compared to other metabolic stimuli, may modify activity of several cell signaling cascades and could have important implications for metabolic health [115] [116].
Safety Considerations: Risk-Benefit Balance
The safety profile of ketogenic diets requires careful consideration. While common side effects during initiation are manageable, rare but serious complications including pancreatitis, cardiomyopathy, and changes in basal ganglia require advanced monitoring and potential diet cessation [117] [118]. The unbalanced macronutrient ratio necessitates clinical evaluation of side effects with strict monitoring of growth and nutritional status, particularly given incomplete understanding of long-term impacts when started in pediatric age [119] [120].
Clinical Implementation Challenges
The lack of established definition hinders appropriate prescription as therapeutic option, while conflicted evidence creates uncertainty among clinicians regarding patient support and guidance [121]. Barriers exist during use of this special and individualized therapy in many clinical settings worldwide [122], highlighting implementation challenges that extend beyond purely medical considerations.
Evidence Quality and Research Limitations
Very few randomized clinical trials involving diets have addressed the combined question of weight loss and cardiovascular outcomes [123], representing a significant limitation in the evidence base. Many safety concerns were expressed due to absence of clinical studies conducted on fragile populations, with assessment of lately emerged evidence relative to safety currently lacking and much needed [124].
Sustainability and Long-term Outcomes
Ketogenic diet was practiced mostly for one to six months, making it a short-term solution to weight loss [125] [126], raising questions about long-term sustainability. Both voluntary and coercive food restriction resulting in negative energy and macronutrient balance have not been designed to be maintained long term, contrasting with traditional alimentation that provides appropriate nutritional density for long-term use [127].
Comparative Effectiveness
Evidence indicates low-carbohydrate and very-low-carbohydrate diets are not superior to other dietary approaches for weight loss, though they may have advantages related to appetite control, triglyceride reduction, and medication reduction in T2D management [128]. This finding challenges claims of categorical superiority while acknowledging specific therapeutic niches.
Future Research Priorities
Several critical research priorities emerge from this analysis:
- Long-term safety and efficacy studies across diverse populations and conditions
- Mechanistic research to better understand ketogenic diet effects at cellular and systems levels
- Comparative effectiveness research against established therapeutic approaches
- Implementation science studies to optimize clinical delivery and patient adherence
- Personalized medicine approaches to identify optimal candidates for ketogenic interventions
.

Conclusion 
The evidence suggests that ketogenic diets occupy a legitimate place in the therapeutic armamentarium for specific neurological and endocrinological conditions, though they do not represent a universal panacea or categorical improvement over all alternative approaches. The characterization of ketogenic diets as either “friend” or “fad” represents a false dichotomy that fails to capture the nuanced reality of their clinical applications.
In neurology, ketogenic diets demonstrate established efficacy for drug-resistant pediatric epilepsy and emerging potential for neurodegenerative conditions. Evidence indicates ketogenic diet therapy is safe when implemented with appropriate monitoring and close follow-up to minimize adverse effects [129] [130]. The expansion of applications beyond epilepsy shows promise but requires additional rigorous clinical investigation.
In endocrinology, ketogenic diets offer demonstrable benefits for short-term glycemic control and weight management, particularly in type 2 diabetes. Results show improved HbA1c after 3 weeks with effects persisting at least 1 year, associated with reduction in glucose-lowering medications, with weight loss observed after short time period maintained with long-term diet [131]. However, long-term persistence remains difficult [132], and cardiovascular safety requires ongoing evaluation.
The characterization of ketogenic diets as “fad” fails to acknowledge their century-long clinical history and robust evidence base in specific applications. Conversely, uncritical promotion as universal therapy ignores important limitations, contraindications, and the need for individualized implementation. The possible use of this diet as therapeutic intervention should be assessed on patient-to-patient basis by adequately skilled medical doctors, keeping in mind current recommendations but reading them through knowledge of current state of the art [133].
Based on available evidence, a well-formulated ketogenic diet does not appear to have major safety concerns for the general public and can be considered a first-line approach for obesity and diabetes [134], though this must be balanced against evidence that ketogenic diets are not better for long-term effects compared to other dietary patterns, with safety concerns requiring consideration in future research [135] [136].
The future of ketogenic diets in clinical practice depends on continued rigorous research, improved clinical implementation protocols, and realistic expectations regarding their therapeutic scope. Rather than representing either revolutionary breakthrough or dietary fad, ketogenic diets exemplify the complexity of nutritional medicine, where therapeutic potential must be carefully balanced against risks, limitations, and individual patient factors.
Clinicians should approach ketogenic diets as legitimate therapeutic tools for specific indications while maintaining critical evaluation of evidence quality, patient selection criteria, and long-term outcomes. This review provides comprehensive summary of current evidence for effectiveness in humans and preclinical models of various neurological disorders, describes molecular mechanisms that may contribute to beneficial effects, and highlights key controversies and current gaps in knowledge [137].
The question of whether ketogenic diets represent “friend or fad” ultimately depends on context, application, and implementation. When appropriately prescribed, carefully monitored, and realistically expectations are set, ketogenic diets can serve as valuable therapeutic interventions. When promoted indiscriminately or implemented without proper medical supervision, they risk becoming another transient dietary trend with potential for harm.
The evidence supports a nuanced position: ketogenic diets represent neither universal panacea nor mere fad, but rather specialized therapeutic tools with specific applications, established benefits, important limitations, and ongoing research needs. Their place in clinical practice should be determined by evidence-based evaluation rather than categorical enthusiasm or dismissal.
Author Note: This analytical review synthesizes current evidence regarding ketogenic diets in neurological and endocrinological applications. The authors declare no conflicts of interest. Correspondence regarding this article should be addressed to the corresponding author
References:
[1] Ketogenic diet for epilepsy: an overview of systematic review and meta-analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35027683/
[2] Ketogenic Diet in the Treatment of Epilepsy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/38732505/
[3] Effect of the ketogenic diet on glycemic control, insulin resistance, and lipid metabolism in patients with T2DM: a systematic review and meta-analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33257645/
[4] Ketogenic Diet: an Endocrinologist Perspective – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31705484/
[5] Ketogenic Diet: an Endocrinologist Perspective – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31705484/
[6] Does a Ketogenic Diet Have a Place Within Diabetes Clinical Practice? Review of Current Evidence and Controversies – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/37966583/
[7] Does a Ketogenic Diet Have a Place Within Diabetes Clinical Practice? Review of Current Evidence and Controversies – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/37966583/
[8] Therapeutic Use of the Ketogenic Diet in Refractory Epilepsy: What We Know and What Still Needs to Be Learned – PubMed – pubmed.ncbi.nlm.nih.govhttps://pubmed.ncbi.nlm.nih.gov/32867258/
[9] Ketogenic diets: an update for child neurologists – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/19535814/?dopt=Abstract
[10] Ketogenic diets: an update for child neurologists – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/19535814/?dopt=Abstract
[11] Ketogenic diet, brain glutamate metabolism and seizure control – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S0952327803002187
[12] Effects of Ketone Bodies on Brain Metabolism and Function in Neurodegenerative Diseases – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33233502/
[13] Effects of Ketone Bodies on Brain Metabolism and Function in Neurodegenerative Diseases – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33233502/
[14] Implementing a low-carbohydrate, ketogenic diet to manage type 2 diabetes mellitus – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/30289048/
[15] Implementing a low-carbohydrate, ketogenic diet to manage type 2 diabetes mellitus – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/30289048/
[16] Neuroprotection by the Ketogenic Diet: Evidence and Controversies – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34888340/
[17] The ketogenic diet: Pros and cons – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31805451/
[18] The ketogenic diet: Pros and cons – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31805451/
[19] The ketogenic diet: Pros and cons – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31805451/
[20] Low-carbohydrate ketogenic diets in body weight control: A recurrent plaguing issue of fad diets? – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33471427/
[21] Role of the ketogenic diet in acute neurological diseases – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S0303846720300706
[22] The ketogenic diet: mechanism of anticonvulsant action – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/6990715/
[23] Ketogenic Diets: Side Effects, Attitude, and Quality of Life – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35036220/
[24] Ketogenic Diet Therapies for Seizures and Status Epilepticus – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33155184/
[25] Ketogenic Diet Therapies for Seizures and Status Epilepticus – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33155184/
[26] The Ketogenic Diet: Proposed Mechanisms of Action – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S1878747923003902
[27] The Ketogenic Diet: Proposed Mechanisms of Action – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S1878747923003902
[28] Hypothalamic hormones and metabolism – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S0920121111002105
[29] Therapeutic Use of the Ketogenic Diet in Refractory Epilepsy: What We Know and What Still Needs to Be Learned – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32867258/
[30] Therapeutic potential of the ketogenic diet: A metabolic switch with implications for neurological disorders, the gut-brain axis, and cardiovascular diseases – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S0955286324001268
[31] Mechanisms of action for the medium-chain triglyceride ketogenic diet in neurological and metabolic disorders – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/29263011/
[32] Ketogenic diet, brain glutamate metabolism and seizure control – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S0952327803002187
[33] Effects of Ketone Bodies on Brain Metabolism and Function in Neurodegenerative Diseases – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33233502/
[34] Effects of Ketone Bodies on Brain Metabolism and Function in Neurodegenerative Diseases – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33233502/
[35] Glucose-Sparing Action of Ketones Boosts Functions Exclusive to Glucose in the Brain – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33168619/
[36] Ketogenic diet, brain glutamate metabolism and seizure control – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S0952327803002187
[37] Ketogenic diet, brain glutamate metabolism and seizure control – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S0952327803002187
[38] Ketogenic diet, brain glutamate metabolism and seizure control – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S0952327803002187
[39] Mechanisms of action for the medium-chain triglyceride ketogenic diet in neurological and metabolic disorders – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/29263011/
[40] Ketogenic diet, brain glutamate metabolism and seizure control – ScienceDirect –https://www.sciencedirect.com/science/article/abs/pii/S0952327803002187
[41] Hypothalamic hormones and metabolism – ScienceDirect –https://www.sciencedirect.com/science/article/abs/pii/S0920121111002105
[42] Hypothalamic hormones and metabolism – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S0920121111002105
[43] Hypothalamic hormones and metabolism – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S0920121111002105
[44] Hypothalamic hormones and metabolism – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/21856125/
[45] Implementing a low-carbohydrate, ketogenic diet to manage type 2 diabetes mellitus – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/30289048/
[46] An overlooked danger of ketogenic diets: Making the case that ketone bodies induce vascular damage by the same mechanisms as glucose – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S0899900720300460
[47] An overlooked danger of ketogenic diets: Making the case that ketone bodies induce vascular damage by the same mechanisms as glucose – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S0899900720300460
[48] The Metabolic Role of Ketogenic Diets in Treating Epilepsy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36501104/
[49] Ketogenic diet for epilepsy: an overview of systematic review and meta-analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35027683/
[50] Ketogenic diet for epilepsy: an overview of systematic review and meta-analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35027683/
[51] Advances in Ketogenic Diet Therapies in Pediatric Epilepsy: A Systematic Review – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/38954792/
[52] Ketogenic Diet in the Treatment of Epilepsy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/38732505/
[53] Ketogenic Diet Therapies for Seizures and Status Epilepticus – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33155184/
[54] Effects of Ketone Bodies on Brain Metabolism and Function in Neurodegenerative Diseases – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33233502/
[55] Neuroprotection by the Ketogenic Diet: Evidence and Controversies – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34888340/
[56] A Ketogenic Diet Improves Cognition and Has Biochemical Effects in Prefrontal Cortex That Are Dissociable From Hippocampus – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/30559660/
[57] A Ketogenic Diet Improves Cognition and Has Biochemical Effects in Prefrontal Cortex That Are Dissociable From Hippocampus – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/30559660/
[58] Effects of the Ketogenic Diet on Glycemic Control in Diabetic Patients: Meta-Analysis of Clinical Trials – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33163300/
[59] Effect of the ketogenic diet on glycemic control, insulin resistance, and lipid metabolism in patients with T2DM: a systematic review and meta-analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33257645/
[60] Efficacy of Ketogenic Diets on Type 2 Diabetes: a Systematic Review – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34448957/
[61] The effect of periodic ketogenic diet on newly diagnosed overweight or obese patients with type 2 diabetes – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35115003/
[62] The effect of periodic ketogenic diet on newly diagnosed overweight or obese patients with type 2 diabetes – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35115003/
[63] Ketogenic diets as treatment of obesity and type 2 diabetes mellitus – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32803691/
[64] Ketogenic diets as treatment of obesity and type 2 diabetes mellitus – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32803691/
[65] Ketogenic diets in the management of type 1 diabetes: Safe or safety concern? – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34598919/
[66] Ketogenic diets in the management of type 1 diabetes: Safe or safety concern? – PubMed – pubmed.ncbi.nlm.nih.govhttps://pubmed.ncbi.nlm.nih.gov/34598919/
[67] Managing type 1 diabetes mellitus with a ketogenic diet – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/37584373/
[68] Managing type 1 diabetes mellitus with a ketogenic diet – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/37584373/
[69] Effects of Ketogenic Diet on Reproductive Hormones in Women With Polycystic Ovary Syndrome – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/37693687/
[70] The Role of Very Low Calorie Ketogenic Diet in Sympathetic Activation through Cortisol Secretion in Male Obese Population – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34575351/
[71] The Role of Very Low Calorie Ketogenic Diet in Sympathetic Activation through Cortisol Secretion in Male Obese Population – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34575351/
[72] Low-carbohydrate diets and men’s cortisol and testosterone: Systematic review and meta-analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35254136/
[73] Ketogenic Diet and Multiple Health Outcomes: An Umbrella Review of Meta-Analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/37836444/
[74] A Review of the Multi-Systemic Complications of a Ketogenic Diet in Children and Infants with Epilepsy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36138681/
[75] Early- and late-onset complications of the ketogenic diet for intractable epilepsy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/15329077/
[76] A Review of the Multi-Systemic Complications of a Ketogenic Diet in Children and Infants with Epilepsy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36138681/
[77] Ketogenic diet in children and adolescents: The effects on growth and nutritional status – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S1043661823001366
[78] Ketogenic diet in children and adolescents: The effects on growth and nutritional status – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S1043661823001366
[79] Ketogenic diet and cardiovascular risk – state of the art review – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0146280624000410
[80] Ketogenic diet and cardiovascular risk – state of the art review – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0146280624000410
[81] An overlooked danger of ketogenic diets: Making the case that ketone bodies induce vascular damage by the same mechanisms as glucose – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32248054/
[82] An overlooked danger of ketogenic diets: Making the case that ketone bodies induce vascular damage by the same mechanisms as glucose – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32248054/
[83] An overlooked danger of ketogenic diets: Making the case that ketone bodies induce vascular damage by the same mechanisms as glucose – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32248054/
[84] Ketogenic Diets: Side Effects, Attitude, and Quality of Life – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35036220/
[85] The impact of a ketogenic diet on weight loss, metabolism, body composition and quality of life – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S2589004224025161
[86] The ketogenic diet: Pros and cons – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31805451/
[87] The Ketogenic Diet: Evidence for Optimism but High-Quality Research Needed – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31825066/
[88] The Ketogenic Diet: Evidence for Optimism but High-Quality Research Needed – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31825066/
[89] Does a Ketogenic Diet Have a Place Within Diabetes Clinical Practice? Review of Current Evidence and Controversies – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/37966583/
[90] Scientific evidence underlying contraindications to the ketogenic diet: An update – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32648647/
[91] Low-carbohydrate ketogenic diets in body weight control: A recurrent plaguing issue of fad diets? – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33471427/
[92] The ketogenic diet: Pros and cons – ScienceDirect –https://www.sciencedirect.com/
science/article/abs/pii/S0021915019315898
[93] Review of current evidence and clinical recommendations on the effects of low-carbohydrate and very-low-carbohydrate (including ketogenic) diets for the management of body weight and other cardiometabolic risk factors: A scientific statement from the National Lipid Association Nutrition and Lifestyle Task Force – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S1933287419302673
[94] The Ketogenic Diet: Evidence for Optimism but High-Quality Research Needed – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31825066/
[95] Effect of a ketogenic diet versus Mediterranean diet on glycated hemoglobin in individuals with prediabetes and type 2 diabetes mellitus: The interventional Keto-Med randomized crossover trial – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35641199/
[96] Ketogenic diet and cardiovascular risk – state of the art review – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/38232923/
[97] A Review of the Multi-Systemic Complications of a Ketogenic Diet in Children and Infants with Epilepsy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36138681/
[98] A Review of the Multi-Systemic Complications of a Ketogenic Diet in Children and Infants with Epilepsy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36138681/
[99] Ketogenic diet in children and adolescents: The effects on growth and nutritional status – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S1043661823001366
[100] Therapeutic Use of the Ketogenic Diet in Refractory Epilepsy: What We Know and What Still Needs to Be Learned – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32867258/
[101] Therapeutic Use of the Ketogenic Diet in Refractory Epilepsy: What We Know and What Still Needs to Be Learned – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32867258/
[102] The Ketogenic Diet: Evidence for Optimism but High-Quality Research Needed – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31825066/
[103] The Ketogenic Diet: Proposed Mechanisms of Action – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S1878747923003902
[104] Association between seizure reduction during ketogenic diet treatment of epilepsy and changes in circulatory metabolites and gut microbiota composition – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/39500011/
[105] The ketogenic diet: mechanism of anticonvulsant action – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/6990715/
[106] The ketogenic diet: mechanism of anticonvulsant action – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/6990715/
[107] Ketogenic Diet: an Endocrinologist Perspective – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31705484/
[108] Ketogenic diet for epilepsy: an overview of systematic review and meta-analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35027683/
[109] Ketogenic diet for epilepsy: an overview of systematic review and meta-analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35027683/
[110] Ketogenic diet for epilepsy: an overview of systematic review and meta-analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35027683/
[111] Ketogenic diet, brain glutamate metabolism and seizure control – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S0952327803002187
[112] Effects of the Ketogenic Diet on Glycemic Control in Diabetic Patients: Meta-Analysis of Clinical Trials – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33163300/
[113] Effects of the Ketogenic Diet on Glycemic Control in Diabetic Patients: Meta-Analysis of Clinical Trials – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33163300/
[114] Ketogenic diets in the management of type 1 diabetes: Safe or safety concern? – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34598919/
[115] Hypothalamic hormones and metabolism – ScienceDirect –https://www.sciencedirect.com/science/article/abs/pii/S0920121111002105
[116] Hypothalamic hormones and metabolism – ScienceDirect – https://www.sciencedirect.com/science/article/abs/pii/S0920121111002105
[117] A Review of the Multi-Systemic Complications of a Ketogenic Diet in Children and Infants with Epilepsy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36138681/
[118] A Review of the Multi-Systemic Complications of a Ketogenic Diet in Children and Infants with Epilepsy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36138681/
[119] Ketogenic diet in children and adolescents: The effects on growth and nutritional status – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S1043661823001366
[120] Ketogenic diet in children and adolescents: The effects on growth and nutritional status – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S1043661823001366
[121] Does a Ketogenic Diet Have a Place Within Diabetes Clinical Practice? Review of Current Evidence and Controversies – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/37966583/
[122] Therapeutic Use of the Ketogenic Diet in Refractory Epilepsy: What We Know and What Still Needs to Be Learned – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32867258/
[123] The ketogenic diet: Pros and cons – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31805451/
[124] Scientific evidence underlying contraindications to the ketogenic diet: An update – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32648647/
[125] Ketogenic Diets: Side Effects, Attitude, and Quality of Life – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35036220/
[126] Ketogenic Diets: Side Effects, Attitude, and Quality of Life – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35036220/
[127] Low-carbohydrate ketogenic diets in body weight control: A recurrent plaguing issue of fad diets? – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33471427/
[128] Review of current evidence and clinical recommendations on the effects of low-carbohydrate and very-low-carbohydrate (including ketogenic) diets for the management of body weight and other cardiometabolic risk factors: A scientific statement from the National Lipid Association Nutrition and Lifestyle Task Force – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S1933287419302673
[129] Ketogenic diet for epilepsy: an overview of systematic review and meta-analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35027683/
[130] A Review of the Multi-Systemic Complications of a Ketogenic Diet in Children and Infants with Epilepsy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36138681/
[131] Efficacy of Ketogenic Diets on Type 2 Diabetes: a Systematic Review – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34448957/
[132] The effect of periodic ketogenic diet on newly diagnosed overweight or obese patients with type 2 diabetes – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35115003/
[133] Scientific evidence underlying contraindications to the ketogenic diet: An update – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32648647/
[134] The Ketogenic Diet: Evidence for Optimism but High-Quality Research Needed – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31825066/
[135] Ketogenic diet and cardiovascular risk – state of the art review – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0146280624000410
[136] Ketogenic diet and cardiovascular risk – state of the art review – ScienceDirect – https://www.sciencedirect.com/science/article/pii/S0146280624000410
[137] Neuroprotection by the Ketogenic Diet: Evidence and Controversies – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34888340/

