Biomarkers for Alzheimer’s Disease: PET to Plasma

Abstract
Background:
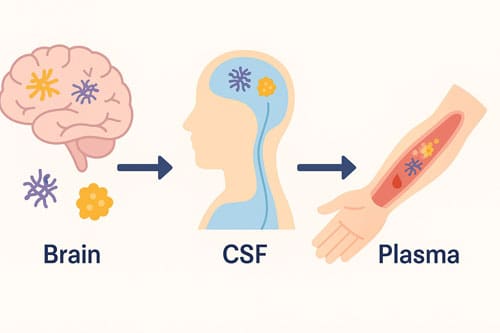
The diagnostic landscape of Alzheimer’s disease (AD) has shifted considerably in recent years. Traditional diagnosis relied heavily on clinical assessments supported by neuropsychological testing and structural imaging. These approaches, while valuable, often lacked the sensitivity and specificity needed to detect AD pathology in its earliest stages. The introduction of biomarker-based diagnostics has transformed the field, enabling more accurate and earlier detection. Positron emission tomography (PET) imaging initially established itself as a highly reliable method for visualizing amyloid and tau pathology in vivo, closely correlating with neuropathological findings at autopsy. More recently, advances in fluid biomarkers, particularly those derived from plasma, have created opportunities for scalable, less invasive, and more cost-effective diagnostic strategies. This review examines the evolution of AD diagnostics from PET imaging to plasma-based assays, focusing on their comparative clinical utility, analytical performance, and barriers to implementation in routine practice.
Methods:
A comprehensive synthesis of literature published between 2023 and 2025 was conducted. Studies were selected based on their evaluation of analytical validity, clinical performance, and implementation feasibility of AD biomarkers across different modalities. Key platforms included single molecule arrays (Simoa), Mesoscale Discovery (MSD), and mass spectrometry for plasma assays, as well as amyloid and tau PET imaging. Attention was given to studies that compared plasma biomarker performance with PET and cerebrospinal fluid (CSF) reference standards, with emphasis on diagnostic accuracy, reproducibility, and practical applicability in clinical settings.
Results:
PET imaging continues to demonstrate excellent accuracy in identifying amyloid and tau pathology, particularly when validated against autopsy-confirmed diagnoses. Plasma biomarkers, however, have shown remarkable progress. Plasma Aβ42/40 ratios and phosphorylated tau isoforms, especially p-tau181 and p-tau217, display strong concordance with PET findings [1]. Plasma p-tau217 has consistently shown the highest accuracy for distinguishing between amyloid-positive and amyloid-negative individuals, including those who remain cognitively unimpaired. Moreover, diagnostic accuracy improves further when plasma biomarkers are combined with demographic and genetic risk factors, such as age and APOE ε4 status. Several commercially available PET, CSF, and plasma assays now reliably detect AD-related amyloid and tau pathology, indicating readiness for broader clinical application [2].
Conclusions:
While PET imaging remains the gold standard for detecting Alzheimer’s pathology, plasma biomarkers represent a major advancement toward more accessible and scalable diagnostic approaches. The transition to plasma-based testing holds promise for early detection, large-scale screening, and improved patient access, particularly in primary care and resource-limited settings. Nevertheless, important challenges remain. These include variability across assay platforms, the need for standardized protocols, and the establishment of clear clinical interpretation guidelines. Addressing these issues will be essential to ensure reliable adoption and integration of plasma biomarkers into everyday clinical practice.
Keywords: Alzheimer’s disease, diagnostic biomarkers, PET imaging, plasma p-tau, amyloid-beta, clinical validation, diagnostic performance, implementation challenges
Introduction
Alzheimer’s disease (AD) represents the most prevalent neurodegenerative disorder globally, with profound implications for healthcare systems worldwide. The World Health Organization reported in 2019 that 50 million people are affected by dementia worldwide and projected that 82 million people will have dementia in 2030, with AD being the most common form comprising 60%-70% of the cases [3]. The advent of disease-modifying therapies has fundamentally altered the therapeutic landscape, necessitating accurate and timely diagnostic approaches that can identify AD pathology in its earliest stages.
The diagnostic evolution of AD has progressed through distinct phases: from purely clinical assessments based on cognitive symptoms to biomarker-driven approaches that enable detection of pathological changes decades before symptom onset. Amyloid and tau biomarkers for Alzheimer’s disease are widely recognized diagnostic tools for the identification of Alzheimer’s disease pathology antemortem and are recommended by the most recent clinical and research guidelines [4] [5]. This progression reflects a deeper understanding of AD as a biological continuum rather than a discrete clinical syndrome.
The introduction of recently approved anti-amyloid immunotherapies for Alzheimer’s disease requiring evidence of amyloid-β pathology from positron emission tomography (PET) or cerebrospinal fluid (CSF) before initiating treatment [6] [7] has intensified the need for accessible and accurate biomarker testing. However, the invasive nature and limited accessibility of traditional biomarker modalities have created notable barriers to widespread implementation.
A growing class of radiotracers targeting specific protein aggregates for amyloid-β (Aβ) and tau are changing the way AD is diagnosed, as these radiotracers directly label the underlying disease pathology [8]. Simultaneously, recently, low-sensitive plasma assays have been replaced by new ultra-sensitive assays such as single molecule enzyme-linked immunosorbent assay (Simoa), the Mesoscale Discovery (MSD) platform, and immunoprecipitation-mass spectrometry (IP-MS) with higher accuracy in the determination of plasma biomarkers of Alzheimer’s disease [9].
This analytical review examines the comparative advantages and limitations of PET and plasma biomarker approaches, evaluating their diagnostic performance, clinical utility, and implementation feasibility. The central research question addresses how the transition from PET to plasma biomarkers represents not merely a technological advancement, but a fundamental shift in AD diagnostic paradigms that could democratize access to accurate AD diagnosis while maintaining clinical precision.
The analysis encompasses three critical dimensions: analytical performance characteristics of different biomarker modalities, clinical validation evidence supporting their diagnostic utility, and practical implementation considerations that will determine their real-world impact. Understanding these interconnected aspects is essential for clinical decision-makers, researchers, and healthcare policy planners navigating the evolving landscape of AD diagnostics.
PET Imaging Biomarkers: The Current Gold Standard
Technological Foundation and Clinical Validation
Positron emission tomography imaging for AD has established itself as the gold standard for in vivo detection of AD pathology through direct visualization of amyloid plaques and tau neurofibrillary tangles. Amyloid and tau PET have contributed remarkably to understanding the biology of Alzheimer disease (AD), aided development of biomarker-driven AD diagnostic criteria, and facilitated approval of the first disease-modifying drugs for AD [10] [11]. The technology’s clinical validation stems from its unique ability to provide spatially resolved quantification of pathological protein deposits in living patients.
New neuroimaging methods not only facilitate the diagnosis of the most common neurodegenerative conditions (particularly Alzheimer Disease [AD]) after symptom onset, but also show diagnostic promise even in the very early or presymptomatic phases of disease. Positron emission tomography (PET) is increasingly recognized as a key clinical tool for differentiating normal age-related changes in brain metabolism from those seen in the earliest stages of specific forms of dementia [12].
The molecular specificity of PET imaging represents a paradigm shift from functional to pathological assessment. The carbon-11 Pittsburgh Compound B (or 11C-PIB) is one of the most studied amyloid radioligands for PET imaging. Compared to a control population, the extent of binding of this radioligand increases by 50% in AD. Other compounds that are approved for beta-amyloid PET imaging include 18F-florbetapir and 18F-flutemetamol [13]. These tracers enable quantitative assessment of amyloid burden with high specificity and sensitivity.
Tau PET Imaging: Beyond Amyloid Assessment
The development of tau-specific PET tracers has expanded diagnostic capabilities beyond amyloid assessment. The recent development of tau-specific positron emission tomography (PET) tracers enables in vivo quantification of regional tau pathology, one of the key lesions in Alzheimer’s disease (AD). Tau PET imaging may become a useful biomarker for clinical diagnosis and tracking of disease progression [14] [15].
Braak staging, global and region-specific tau measures yielded similar diagnostic accuracies. While all tau measures were related to amyloid and global cognition, memory and hippocampal/entorhinal volume/thickness were associated with regional tracer retention in the medial temporal lobe. Key regions of tau accumulation included medial temporal and inferior/middle temporal regions, retrosplenial cortex, and banks of the superior temporal sulcus. Whole-brain tau PET measures might be adequate biomarkers to detect AD-related tau pathology [16].
The clinical relevance of tau PET extends beyond diagnostic accuracy to prognostic utility. Increasing levels of tau most consistently relate to declines in cognition preceding biomarker collection. These findings support models of Alzheimer disease (AD) staging that suggest that elevated β-amyloid alone may be insufficient to produce cognitive change [17] [18].
Clinical Implementation and Appropriate Use Criteria
The clinical implementation of PET imaging has been guided by evidence-based appropriate use criteria. For amyloid PET, 7 scenarios were rated as appropriate, 2 as uncertain, and 8 as rarely appropriate. For tau PET, 5 scenarios were rated as appropriate, 6 as uncertain, and 6 as rarely appropriate. AUC for amyloid and tau PET provide expert recommendations for clinical use of these technologies in the evolving landscape of diagnostics and therapeutics for Alzheimer’s disease [19].
Limitations and Accessibility Challenges
Despite its clinical validation, PET imaging faces notable implementation barriers. The administration of these drugs presents challenges owing to the invasiveness, high cost and limited availability of amyloid-PET and cerebrospinal fluid tests for guiding drug administration. Amyloid-PET and CSF tests are invasive and expensive and are not universally available, which limits their use in routine clinical practice [20] [21] [22].
The accessibility limitations of PET imaging extend beyond cost considerations to include infrastructure requirements, specialized personnel, and geographic availability. These constraints have created a major gap between the clinical need for biomarker-based diagnosis and the practical capacity to deliver such services at scale.
Plasma Biomarkers: The Emerging Paradigm
Analytical Platform Evolution
The development of ultra-sensitive analytical platforms has transformed the feasibility of blood-based AD biomarker testing. Recently, low-sensitive plasma assays have been replaced by new ultra-sensitive assays such as single molecule enzyme-linked immunosorbent assay (Simoa), the Mesoscale Discovery (MSD) platform, and immunoprecipitation-mass spectrometry (IP-MS) with higher accuracy in the determination of plasma biomarkers of Alzheimer’s disease (AD). Despite the noteworthy variability, many studies have established in-house cut-off values for the most promising available biomarkers [23].
Single Molecule Array (Simoa) Technology
The Simoa HD-1 Analyzer provides full automation of single-molecule array (Simoa) technology for digital immunoassays. The instrument is capable of single-molecule sensitivity and multiplexing with short turnaround times and a throughput of 66 samples/h [24] [25]. The average sensitivity improvement of the Simoa immunoassays versus conventional ELISA was >1200-fold, with coefficients of variation of <10% [26].
The analytical performance of Simoa technology has been validated across multiple biomarker applications. Ella returned plasmatic NfL levels notably higher than SiMoA, however the results were strongly correlated (r = 0.94), and a proportional coefficient of 0.58 between the two assays was calculated. Both assays detected higher plasma NfL levels in patients with dementia than in the control group (p < 0.0001) and allowed their discrimination with excellent diagnostic performance (AUC > 0.95). No difference was found between Alzheimer’s and Frontotemporal dementia either using SiMoA or Ella. Both the analytical platforms resulted effective in analysing plasma levels of NfL [27].
Mesoscale Discovery (MSD) Platform
The MSD platform utilizes electrochemiluminescence technology for biomarker quantification. MSD HPE and Quanterix Simoa are analytic platforms to detect biofluid cytokines. However, Simoa demonstrated overall higher concentrations and the two platforms did not show agreement when directly compared against one another. Relative cytokine ratios and associations demonstrated similar patterns across platforms. Absolute cytokine concentrations may not be directly comparable across platforms [28].
Platform Comparison and Standardization
Cross-platform analytical validation has revealed both concordance and discordance in biomarker measurements. Lumipulse and SIMOA AD-related markers showed a fair correlation in plasma. In the comparison between SIMOA and Lumipulse plasma markers, both techniques exhibited similar diagnostic accuracy for AD for p-tau181 (0.87; 95 %CI 0.81–0.94, vs 0.85; 95 %CI 0.78–0.93), whereas the best performance was reached by p-tau181/ Aβ42 Lumipulse ratio (ROC AUC 0.915, 95 %CI 0.86–0.97). The study thus confirmed the construct validity of both Lumipulse and SIMOA techniques for the identification of CSF AD pattern in clinical settings [29] [30].
Key Plasma Biomarker Categories
Phosphorylated Tau Species
Phosphorylated tau (p-tau) biomarkers have emerged as the most promising plasma biomarkers for AD. Plasma phosphorylated(p)-tau, specifically plasma p-tau217, is a robust candidate across both primary and secondary care settings [31] [32]. All assays showed robust analytical performance, and particularly P-tau217 Eli Lilly; P-tau231 Gothenburg and all P-tau181 assays showed robust clinical performance to differentiate AD from controls, with AUCs 0.936-0.995. Results obtained with all P-tau181 assays, P-tau217 Eli Lilly assay, and P-tau231 Gothenburg assay strongly correlated [33].
The diagnostic utility of p-tau217 extends to preclinical stages of AD. Plasma p-tau217 has shown the best accuracy in distinguishing Aβ-PET+ from Aβ-PET-even in cognitively unimpaired individuals [34]. This capability addresses a critical clinical need for identifying individuals at risk of AD progression before symptom onset.
Amyloid-Beta Ratios
Plasma amyloid-beta measurements focus primarily on the Aβ42/40 ratio rather than absolute concentrations. A combination of plasma Aβ42/40 ratio, age, and APOE status showed the best accuracy in diagnosing brain amyloidosis with a liquid chromatography-mass spectrometry (LC-MS) assay [35]. ELISA and SIMOA demonstrated equivalent performances in detecting cerebral amyloidosis through plasma Aβ1-42/Aβ1-40, both with high negative predictive values, making them equally suitable non-invasive prescreening tools for clinical trials [36].
Neurodegeneration and Neuroinflammation Markers
Beyond core AD pathology markers, plasma biomarkers extend to markers of neurodegeneration and neuroinflammation. A combination of plasma p-tau181, NfL, and GFAP, but not Aβ1-42/1-40, might be useful to discriminate AD, FTD, and DLB [37]. The range of AD co-pathology can be detected with plasma biomarkers in the DLB continuum, particularly with plasma p-tau-181 and GFAP [38].
Clinical Validation and Diagnostic Performance
Diagnostic Accuracy Studies
Multiple large-scale validation studies have demonstrated the clinical utility of plasma biomarkers. Staging the severity of Alzheimer’s disease pathology using biomarkers is useful for therapeutic trials and clinical prognosis. Disease staging with amyloid and tau PET has face validity; however, this would be more practical with plasma biomarkers [39]. Plasma p-tau217 and amyloid PET provide useful information about predicting rates of future cognitive decline in cognitively unimpaired individuals at the population mean level, but not at the individual person level [40].
Comparison with Traditional Biomarkers
Direct comparisons between plasma biomarkers and established methods have revealed both concordances and unique advantages. PET, CSF and plasma biomarkers of tau pathology may be differentially associated with Alzheimer’s disease (AD)-related demographic, cognitive, genetic and neuroimaging markers. Tau PET vs CSF p-tau181 showed differential associations with AD-related features, with specific patterns observed in different analytical models [41] [42].
Implementation Challenges and Considerations
Pre-analytical and Analytical Variability
Despite the high performance and robustness demonstrated in research, plasma p-tau217, like all plasma biomarkers, can be affected by analytical and pre-analytical variability as well as patient comorbidities, sex, ethnicity, and race. This review also discusses the advantages of the two-point cut-off approach to mitigating these factors, and the challenges raised by the resulting intermediate range measurements, where clinical guidance is still unclear. Further validation of plasma p-tau217 in heterogeneous, real-world cohorts will help to increase confidence in testing and support establishing a standardized approach [43].
Clinical Integration Challenges
The challenges include understanding the effect of pre-analytical and analytical conditions, potential confounding factors, and comorbidities that could influence outcomes of blood biomarkers and their use in diverse populations. Additionally, distinct scenarios present their own specific challenges. In memory clinics, the successful integration of blood biomarkers in diagnostic tests will require well-established diagnostic accuracy and comprehensive assessments of the effect of blood biomarkers on the diagnostic confidence and patient management of clinicians. In primary care settings, and even more when implemented in population-based screening programmes, the implementation of blood biomarkers will be challenged by the need for education of primary care clinical staff and clear guidelines [44] [45].

Comparative Analysis: PET versus Plasma Biomarkers
Diagnostic Performance Metrics
The comparative diagnostic performance between PET and plasma biomarkers reveals complementary strengths and applications. PET- and CSF-related A/T/N biomarkers in combination can accurately predict the specific stages of AD neuropathology. PET- and CSF-related A/T/N biomarkers alone may serve as a precise diagnostic tool for detecting AD neuropathology at autopsy [46]. However, plasma biomarkers demonstrate competitive performance in specific clinical contexts.
Plasma pTau-217 and N-terminal tau (NTA) enhance sensitivity to identify tau PET positivity in amyloid-β positive individuals [47], demonstrating the potential for plasma biomarkers to complement rather than simply replace PET imaging in clinical algorithms.
Cost-Effectiveness Analysis
Economic considerations represent a critical factor in biomarker selection and implementation strategies. Despite their lower accuracy, blood biomarker tests could be a cost-effective alternative. However, the administration of these drugs presents challenges owing to the invasiveness, high cost and limited availability of amyloid-PET and cerebrospinal fluid tests for guiding drug administration. Our manuscript explores the potential of less invasive blood biomarkers as a diagnostic method, with a cost-effectiveness analysis and a comparison with traditional tests [48] [49].
The implementation of plasma biomarkers could save a remarkable proportion of more expensive traditional exams, making the diagnostic workup more cost-effective and improving patient care [50]. The economic advantage of plasma biomarkers extends beyond direct testing costs to include reduced infrastructure requirements and improved accessibility.
Clinical Utility and Accessibility
The accessibility dimension represents perhaps the most significant differentiator between PET and plasma approaches. Plasma biomarkers are poised to become a more affordable and less invasive alternative to PET and CSF testing. However, understanding the factors that impact plasma biomarker measurement and interpretation is critical prior to their implementation in routine clinical use [51].
Plasma biomarkers are poised to become a more affordable and less invasive alternative to PET and CSF testing. As novel, anti-amyloid therapies have become more widely available, access to timely and accurate diagnosis has become integral to ensuring optimal treatment of patients with early-stage Alzheimer’s disease (AD). Plasma biomarkers are a promising tool for identifying AD pathology; however, several technical and clinical factors need to be considered prior to their implementation in routine clinical use [52] [53].
Sensitivity to Disease Progression
Both PET and plasma biomarkers demonstrate utility in tracking disease progression, though with different temporal dynamics. Plasma biomarkers differ across diagnostic groups (DEM > MCI > CU) and are altered in Aβ-PET-positive individuals. Altered plasma biomarker levels are associated with poorer brain health and kidney function [54].
Amyloid PET detects the deposition of brain Aβ earlier than CSF fluid biomarkers [55], suggesting temporal advantages for PET imaging in the earliest disease stages. However, plasma biomarkers demonstrate utility across the disease continuum with practical advantages for longitudinal monitoring.
Clinical Implementation Considerations
Regulatory and Standardization Framework
The clinical implementation of AD biomarkers requires robust regulatory frameworks and standardization protocols. Plasma biomarkers such as phosphorylated tau-217 (p-tau217) offer a promising, accessible alternative to cerebrospinal fluid (CSF) and positron emission tomography (PET) for detecting Alzheimer’s disease pathology, especially in settings with limited diagnostic resources. Clinical integration of plasma biomarker testing presents challenges, particularly in interpreting results. This includes uncertainties around intermediate results and their role in patient management. Clear frameworks and guidelines are essential to optimize the use of plasma biomarkers [56].
Healthcare System Integration
The integration of biomarker testing into existing healthcare frameworks presents multifaceted challenges. In memory clinics, the successful integration of blood biomarkers in diagnostic tests will require well-established diagnostic accuracy and comprehensive assessments of the effect of blood biomarkers on the diagnostic confidence and patient management of clinicians. In primary care settings, and even more when implemented in population-based screening programmes, the implementation of blood biomarkers will be challenged by the need for education of primary care clinical staff and clear guidelines. However, despite the challenges, blood biomarkers hold great promise for substantially enhancing the diagnostic accuracy and effectively streamlining referral processes, leading to earlier diagnosis and access to treatments. The ongoing efforts that are shaping the integration of blood biomarkers across diverse clinical settings pave the way towards precision medicine in Alzheimer’s disease [57].
Education and Training Requirements
The successful implementation of biomarker-based diagnostics requires comprehensive education and training programs. Despite these advancements, however, much work is needed before AD BBMs can be implemented in widespread clinical practice. Cutpoints must be established, the influence of chronic conditions and medications on BBM levels must be better understood, and guidelines must be created for healthcare providers related to interpreting and communicating information obtained from AD BBMs. Additionally, the development of BBMs for synaptic dysfunction, inflammation, and cerebrovascular disease may provide better precision medicine approaches to treating AD and related dementia. Future research and collaboration between scientists and physicians are essential to addressing these challenges and further advancing AD BBMs [58].
Quality Assurance and Standardization
Quality assurance represents a critical component of biomarker implementation. The recent development of fully automated tests for fluid-based biomarkers improves test reliability. The continued development of plasma biomarkers holds promise for the future management of patients with Alzheimer’s disease [59].
The standardization challenges extend beyond analytical platforms to include interpretation guidelines, cut-point establishment, and quality control procedures across diverse clinical settings and populations.
Future Directions and Emerging Technologies
Technological Advances
The continuous evolution of analytical technologies promises further improvements in plasma biomarker performance. Recent technological advances have improved the sensitivity and specificity of blood-based biomarkers for Alzheimer’s disease and related dementias. Accurate quantification of amyloid-ß peptide, phosphorylated tau (pTau) isoforms, as well as markers of neurodegeneration (neurofilament light chain [NfL]) and neuro-immune activation (glial fibrillary acidic protein [GFAP] and chitinase-3-like protein 1 [YKL-40]) in blood has allowed researchers to characterize neurobiological processes at scale in a cost-effective and minimally invasive manner [60] [61].
Precision Medicine Applications
The integration of multiple biomarker modalities promises enhanced precision in AD diagnosis and treatment selection. Multiple specific biomarkers need to be used to improve the precision of these tests. Research into new blood biomarkers and their clinical efficacy is needed [62]. Established AD diagnostic models using plasma biomarkers for Chinese participants suggest the simplified diagnostic model provides an accessible and practical way for large-scale screening in the clinic and community, especially in developing countries [63].
Point-of-Care Testing Development
Emerging point-of-care testing technologies represent the next frontier in biomarker accessibility. Continued advances in label-free electrical biosensors pave the way to simple, rapid, cost-effective, high-sensitivity, and quantitative biomarker testing at the point-of-care setting that would profoundly transform healthcare. However, implementation in routine diagnostics is faced with significant challenges associated with the inherent requirement for biofluid sample processing before and during testing [64] [65].
Population-Level Implementation
The scalability of plasma biomarkers to population-level screening presents both opportunities and challenges. As the prevalence of Alzheimer’s disease (AD) and its impact on healthcare systems increase, developing tools for accurate diagnosis and monitoring of disease progression is a priority. Recent technological advancements have allowed for the development of blood-based biomarkers (BBMs) to aid in the diagnosis of AD [66].
Discussion
The evolution from PET to plasma biomarkers represents a paradigmatic shift in Alzheimer’s disease diagnostics that extends far beyond technological advancement. This transition embodies a fundamental reconceptualization of how healthcare systems can address the growing burden of neurodegenerative diseases while maintaining diagnostic precision and expanding accessibility.
Analytical Performance and Clinical Validation
The analytical evidence demonstrates that plasma biomarkers, while not achieving the absolute precision of PET imaging, provide clinically meaningful diagnostic accuracy across multiple clinical contexts. Recently developed assays for plasma biomarkers have undeniable importance in AD research, with improved analytical and diagnostic performance. Some biomarkers have been extensively used in clinical trials and are now clinically available. Nonetheless, several challenges remain to their widespread use in clinical practice [67].
The comparative analysis reveals that the choice between PET and plasma biomarkers should not be viewed as an either-or decision, but rather as complementary approaches optimized for different clinical scenarios. PET imaging maintains advantages in spatial resolution and pathological specificity, making it ideal for research applications and complex diagnostic cases. Conversely, plasma biomarkers excel in accessibility, cost-effectiveness, and longitudinal monitoring capabilities.
Implementation Paradigms
The implementation challenges identified in this analysis highlight the complexity of translating biomarker research into clinical practice. Given the potential for plasma biomarkers to enhance Alzheimer’s disease diagnosis in primary care, it is important to understand how to interpret the biomarkers in light of factors that physiologically impact blood biomarker levels. This information will be critical for the establishment of reference ranges and thus the correct interpretation of these biomarkers in clinical screening [68].
The successful integration of plasma biomarkers requires a comprehensive approach addressing analytical standardization, clinical interpretation guidelines, healthcare provider education, and quality assurance frameworks. These implementation considerations represent as significant a challenge as the original biomarker development, requiring sustained collaboration between researchers, clinicians, regulatory agencies, and healthcare systems.
Healthcare System Transformation
The transition to plasma biomarkers has implications extending beyond AD diagnostics to broader healthcare system transformation. The democratization of biomarker testing through accessible blood-based approaches could fundamentally alter patient care pathways, enable earlier intervention, and support population-level screening initiatives previously considered impractical.
However, this transformation must be carefully managed to avoid potential pitfalls including overdiagnosis, inadequate clinical interpretation, and healthcare system disruption. The intermediate result ranges that characterize plasma biomarker testing present particular challenges for clinical decision-making, requiring sophisticated clinical algorithms and provider training.
Economic and Social Implications
The economic implications of the PET-to-plasma transition extend beyond direct testing costs to encompass broader healthcare system efficiency gains. Dementia management has evolved with drugs such as lecanemab, shifting management from palliative care to early diagnosis and intervention. As a result, a focus on early diagnosis and swift therapeutic intervention is critical. Amyloid-PET and CSF biomarkers are now widely accepted research tools used to assess the Aβ status for AD diagnoses [69] [70].
The social implications include improved patient experience through reduced invasiveness, enhanced accessibility for underserved populations, and the potential for earlier intervention with disease-modifying therapies. These benefits must be balanced against the risks of increased healthcare utilization and the psychological impact of biomarker-positive results in asymptomatic individuals.
Limitations and Future Research Directions
This analysis acknowledges several important limitations. The rapidly evolving nature of the field means that some findings may be superseded by emerging research. The heterogeneity of study populations, analytical platforms, and clinical endpoints complicates direct comparisons between studies. Additionally, the long-term clinical outcomes associated with biomarker-guided decision-making remain to be fully established.
Future research priorities should focus on standardization of analytical procedures, establishment of population-specific reference ranges, validation in diverse demographic groups, and longitudinal studies evaluating clinical outcomes associated with biomarker-guided care. The development of integrated diagnostic algorithms combining multiple biomarker modalities represents a particularly promising research direction.

Conclusion 
The transition from PET to plasma biomarkers in Alzheimer’s disease diagnostics represents a transformative shift with profound implications for clinical practice, healthcare accessibility, and patient outcomes. While PET imaging maintains its role as the gold standard for pathological confirmation and research applications, plasma biomarkers offer unprecedented opportunities for accessible, cost-effective screening and monitoring across diverse clinical settings.
The analytical evidence supports the clinical utility of plasma biomarkers, particularly phosphorylated tau-217 and amyloid-beta ratios, across the Alzheimer’s disease continuum. These biomarkers demonstrate competitive diagnostic accuracy with traditional approaches while offering substantial advantages in accessibility, patient acceptability, and implementation scalability.
However, successful clinical implementation requires addressing significant challenges including analytical standardization, clinical interpretation guidelines, healthcare provider education, and quality assurance frameworks. The complexity of these implementation considerations underscores the need for coordinated efforts among researchers, clinicians, regulatory agencies, and healthcare systems.
The future of AD diagnostics likely involves a tiered approach leveraging plasma biomarkers for initial screening and risk stratification, with PET imaging reserved for confirmatory testing and complex clinical scenarios. This integrated approach could maximize the complementary strengths of both modalities while optimizing healthcare resource utilization.
As disease-modifying therapies continue to evolve, the demand for accurate, accessible biomarker testing will only intensify. The successful transition to plasma-based diagnostics could democratize access to precision medicine approaches in AD, ultimately improving patient outcomes while managing healthcare system sustainability.
The evidence supports cautious optimism regarding the clinical implementation of plasma biomarkers, provided that implementation is guided by rigorous scientific evidence, comprehensive standardization efforts, and sustained commitment to quality assurance. The ultimate success of this paradigm shift will be measured not only in diagnostic accuracy metrics but in improved patient outcomes, healthcare system efficiency, and equitable access to precision medicine approaches for Alzheimer’s disease.
Key References
- Pais, M. V., Forlenza, O. V., & Diniz, B. S. (2023). Plasma Biomarkers of Alzheimer’s Disease: A Review of Available Assays, Recent Developments, and Implications for Clinical Practice. Journal of Alzheimer’s Disease Reports, 7(1), 355-380.
- Schöll, M., Vrillon, A., Ikeuchi, T., Quevenco, F. C., Iaccarino, L., Vasileva-Metodiev, S. Z., … & Palmqvist, S. (2025). Cutting through the noise: A narrative review of Alzheimer’s disease plasma biomarkers for routine clinical use. Journal of Prevention of Alzheimer’s Disease, 12(4), 100056.
- Rabinovici, G. D., Knopman, D. S., Arbizu, J., Benzinger, T. L. S., Donohoe, K. J., Hansson, O., … & Johnson, K. A. (2024). Diagnosis of Alzheimer’s disease using plasma biomarkers adjusted to clinical probability. Nature Medicine.
- Woo, M. S., Tissot, C., Lantero-Rodriguez, J., Snellman, A., Therriault, J., Rahmouni, N., … & Rosa-Neto, P. (2024). Predicting amyloid PET and tau PET stages with plasma biomarkers. Alzheimer’s & Dementia, 20(2), 1166-1174.
- Baiardi, S., Quadalti, C., Mammana, A., Dellavalle, S., Zenesini, C., Sambati, L., … & Parchi, P. (2023). Plasma biomarkers for Alzheimer’s disease: a field-test in a memory clinic. Alzheimer’s Research & Therapy.
- Diaz-Galvan, P., Przybelski, S. A., Algeciras-Schimnich, A., Figdore, D. J., Lesnick, T. G., Schwarz, C. G., … & Kantarci, K. (2024). Plasma biomarkers of Alzheimer’s disease in the continuum of dementia with Lewy bodies. Alzheimer’s & Dementia.
- Hazan, J., Liu, K. Y., Isaacs, J. D., & Howard, R. (2025). Cut-points and gray zones: The challenges of integrating Alzheimer’s disease plasma biomarkers into clinical practice. Alzheimer’s & Dementia, 21(3), e70113.
- Sun, Q., Ni, J., Wei, M., Long, S., Li, T., Fan, D., … & Tian, J. (2023). Associations of the A/T/N profiles in PET, CSF, and plasma biomarkers with Alzheimer’s disease neuropathology at autopsy. Frontiers in Aging Neuroscience.
- Rudolph, M. D., Sutphen, C. L., Register, T. C., Whitlow, C. T., Sai, K. K. S., Hughes, T. M., … & Lockhart, S. N. (2024). Associations among plasma, MRI, and amyloid PET biomarkers of Alzheimer’s disease and related dementias and the impact of health-related comorbidities in a community-dwelling cohort. Alzheimer’s & Dementia, 20(6), 4159-4173.
- Mattsson-Carlgren, N., Salvadó, G., Ashton, N. J., Tideman, P., Stomrud, E., Zetterberg, H., … & Hansson, O. (2024). Comparison of plasma biomarkers and amyloid PET for predicting memory decline in cognitively unimpaired individuals. JAMA Neurology.
- Iaccarino, L., Burnham, S. C., Dell’Agnello, G., Dowsett, S. A., & Epelbaum, S. (2023). Diagnostic Biomarkers of Amyloid and Tau Pathology in Alzheimer’s Disease: An Overview of Tests for Clinical Practice in the United States and Europe. Journal of Prevention of Alzheimer’s Disease, 10(3), 426-442.
- Chatterjee, P., Pedrini, S., Doecke, J. D., Thota, R., Villemagne, V. L., Doré, V., … & AIBL Research Group. (2023). Predicting amyloid PET and tau PET stages with plasma biomarkers. Alzheimer’s & Dementia, 19(4), 1117-1134.
- Jack, C. R., Rabinovici, G. D., Shaw, L. M., Gotschalk, J., Ashton, N. J., Benzinger, T. L. S., … & Johnson, K. A. (2025). The Impact of Amyloid and Tau PET on Alzheimer Disease Diagnostics: AJR Expert Panel Narrative Review. American Journal of Roentgenology.
- Nasrallah, I. M., Chen, Y. J., & Hsieh, M. K. (2020). Amyloid and Tau PET Imaging of Alzheimer Disease and Other Neurodegenerative Conditions. Neuroimaging Clinics of North America, 30(4), 427-447.
- Rabinovici, G. D., Knopman, D. S., Arbizu, J., Benzinger, T. L. S., Donohoe, K. J., Hansson, O., … & Johnson, K. A. (2025). Updated Appropriate Use Criteria for Amyloid and Tau PET: A Report from the Alzheimer’s Association and Society for Nuclear Medicine and Molecular Imaging Workgroup. Alzheimer’s & Dementia.
- Schöll, M., Lockhart, S. N., Schonhaut, D. R., O’Neil, J. P., Janabi, M., Ossenkoppele, R., … & Rabinovici, G. D. (2017). Comparison of multiple tau-PET measures as biomarkers in aging and Alzheimer’s disease. NeuroImage, 157, 448-463.
- Nasrallah, I. M., Chen, Y. J., & Hsieh, M. K. (2020). Amyloid and Tau PET Imaging of Alzheimer Disease and Other Neurodegenerative Conditions. Neuroimaging Clinics of North America, 30(4), 427-447.
- Mattsson-Carlgren, N., Janelidze, S., Palmqvist, S., Cullen, N., Svenningsson, A. L., Strandberg, O., … & Hansson, O. (2021). Tau PET correlates with different Alzheimer’s disease-related features compared to CSF and plasma p-tau biomarkers. EMBO Molecular Medicine, 13(8), e14161.
- Lecouteux, C., Fasseur, M., Frere, D., & Janin, Y. L. (2017). Tau protein aggregation in Alzheimer’s disease: An attractive target for the development of novel therapeutic agents. European Journal of Medicinal Chemistry, 139, 153-177.
- Adams, J. N., Maass, A., Harrison, T. M., Baker, S. L., & Jagust, W. J. (2018). Influence of tau PET, amyloid PET, and hippocampal volume on cognition in Alzheimer disease. Neurology, 91(9), e859-e866.
- Pais, M. V., Forlenza, O. V., & Diniz, B. S. (2023). Plasma Biomarkers of Alzheimer’s Disease: A Review of Available Assays, Recent Developments, and Implications for Clinical Practice. Journal of Alzheimer’s Disease Reports, 7(1), 355-380.
- Walker, K. A., Bown, C. W., Artiga, E. J., Tran, T. H., Reitz, C., Silverberg, N., … & Gottesman, R. F. (2018). A comparison of biofluid cytokine markers across platform technologies: Correspondence or divergence?. Cytokine, 111, 481-491.
- Chatziefstathiou, A., Canaslan, S., Kanata, E., Vekrellis, K., Constantinides, V. C., Paraskevas, G. P., … & Dafou, D. (2023). Neurofilament-light chain quantification by Simoa and Ella in plasma from patients with dementia: a comparative study. Biomedicines, 12(6), 1253.
- Ingannato, A., Bagnoli, S., Mazzeo, S., Giacomucci, G., Bessi, V., Ferrari, C., … & Nacmias, B. (2024). Plasma p-tau181 and amyloid markers in Alzheimer’s disease: A comparison between Lumipulse and SIMOA. Neurobiology of Aging, 143, 58-66.
- Chatziefstathiou, A., Canaslan, S., Kanata, E., Vekrellis, K., Constantinides, V. C., Paraskevas, G. P., … & Dafou, D. (2024). SIMOA Diagnostics on Alzheimer’s Disease and Frontotemporal Dementia. Biomedicines, 12(6), 1253.
- Yang, C. C., Yang, S. Y., Chieh, J. J., Horng, H. E., Hong, C. Y., Yang, H. C., … & Chiu, M. J. (2021). Development of a Plasma Biomarker Diagnostic Model Incorporating Ultrasensitive Digital Immunoassay as a Screening Strategy for Alzheimer Disease in a Chinese Population. JAMA Network Open, 4(11), e2134516.
- De Meyer, S., Schaeverbeke, J. M., Verberk, I. M., Gille, B., De Schaepdryver, M., Luckett, E. S., … & Teunissen, C. E. (2020). Comparison of ELISA- and SIMOA-based quantification of plasma Aβ ratios for early detection of cerebral amyloidosis. Alzheimer’s Research & Therapy, 12, 162.
- Thijssen, E. H., Verberk, I. M., Vanbrabant, J., Keshavan, A., Stomrud, E., van der Lee, S. J., … & Teunissen, C. E. (2021). Clinical and analytical comparison of six Simoa assays for plasma P-tau isoforms P-tau181, P-tau217, and P-tau231. Alzheimer’s Research & Therapy, 13, 198.
- Rissin, D. M., Kan, C. W., Campbell, T. G., Howes, S. C., Fournier, D. R., Song, L., … & Duffy, D. C. (2015). The Simoa HD-1 Analyzer: A Novel Fully Automated Digital Immunoassay Analyzer with Single-Molecule Sensitivity and Multiplexing. Journal of Laboratory Automation, 15(6), 423-429.
- Baiardi, S., Quadalti, C., Mammana, A., Dellavalle, S., Zenesini, C., Sambati, L., … & Parchi, P. (2022). Differential diagnostic performance of a panel of plasma biomarkers for different types of dementia. Alzheimer’s Research & Therapy, 14, 153.
- Okada, D. (2024). Plasma proteins as potential biomarkers of aging of single tissue and cell type. Age, 25(1), 177-181.
- Schöll, M., Vrillon, A., Ikeuchi, T., Quevenco, F. C., Iaccarino, L., Vasileva-Metodiev, S. Z., … & Palmqvist, S. (2025). Cutting through the noise: A narrative review of Alzheimer’s disease plasma biomarkers for routine clinical use. Journal of Prevention of Alzheimer’s Disease, 12(4), 100056.
- Arslan, B., Zetterberg, H., & Ashton, N. J. (2024). Challenges in the practical implementation of blood biomarkers for Alzheimer’s disease. Clinical Chemistry and Laboratory Medicine, 62(6), 1063-1069.
- Noda, K., Lim, Y., Goto, R., Sengoku, S., & Kodama, K. (2024). Cost-effectiveness comparison between blood biomarkers and conventional tests in Alzheimer’s disease diagnosis. Drug Discovery Today, 29(3), 103911.
- Dark, H. E., Duggan, M. R., & Walker, K. A. (2024). Plasma biomarkers for Alzheimer’s and related dementias: A review and outlook for clinical neuropsychology. Archives of Clinical Neuropsychology, 39(3), 313-324.
- Lawler, M., Keeling, P., Kholmanskikh, O., Minnaard, W., Moehlig-Zuttermeister, H., Normanno, N., … & Lawler, M. (2024). Empowering effective biomarker-driven precision oncology: A call to action. European Journal of Cancer, 207, 114128.
- Ankeny, S. E., Bacci, J. R., Decourt, B., Sabbagh, M. N., & Mielke, M. M. (2024). Navigating the Landscape of Plasma Biomarkers in Alzheimer’s Disease: Focus on Past, Present, and Future Clinical Applications. Neurotherapeutics, 13(6), 1541-1557.
- Noda, K., Lim, Y., Goto, R., Sengoku, S., & Kodama, K. (2024). Cost-effectiveness comparison between blood biomarkers and conventional tests in Alzheimer’s disease diagnosis. Drug Discovery Today, 29(3), 103911.
- Li, L., Tian, S., He, Y., Gu, G., Xu, J., Zhang, H., … & Ren, Y. (2022). Integrated Platform Addressing the Finger-Prick Blood Processing Challenges of Point-of-Care Electrical Biomarker Testing. ACS Sensors, 7(1), 247-254.
- Pais, M. V., Forlenza, O. V., & Diniz, B. S. (2023). Plasma Biomarkers of Alzheimer’s Disease: A Review of Available Assays, Recent Developments, and Implications for Clinical Practice. Journal of Alzheimer’s Disease Reports, 7(1), 355-380.

