Venetoclax-based Regimens in AML: The New Standard or a Temporary Fix?
Abstract
Acute myeloid leukemia (AML) remains a challenging hematologic malignancy, particularly among older adults and patients unfit for intensive chemotherapy. Over the past decade, treatment models have shifted with the advent of venetoclax, a selective BCL-2 inhibitor, in combination with hypomethylating agents. This development has redefined therapeutic strategies, offering a less intensive yet highly active regimen for a population historically limited to supportive care or low-intensity therapy with modest benefit.
This review provides a comprehensive analysis of the clinical efficacy, safety, resistance mechanisms, and future directions of venetoclax-based regimens in AML. Results from pivotal trials, most notably VIALE-A, demonstrated a remarkable survival advantage, with venetoclax plus azacitidine achieving a median overall survival of 14.7 months compared with 9.6 months for azacitidine alone.[1] [2] [3] These findings established venetoclax-based therapy as a preferred frontline option for patients ineligible for intensive induction. Real-world data have corroborated these outcomes, showing high composite complete remission rates, rapid disease clearance, and meaningful improvements in quality of life.
Despite these advances, challenges remain. Approximately 30 percent of patients do not respond to venetoclax-based therapy, and among initial responders, relapse is common, reflecting the persistence of drug-resistant leukemic clones.[4] Mechanisms of resistance include upregulation of alternative anti-apoptotic proteins such as MCL-1 and BCL-XL, clonal evolution, and metabolic reprogramming. Furthermore, prolonged myelosuppression and infectious complications pose notable management concerns, highlighting the need for careful patient selection and supportive care optimization.
Emerging strategies aim to overcome these limitations through rational combination therapies, including the addition of FLT3, IDH1/2, or menin inhibitors, as well as novel agents targeting apoptotic pathways and leukemic stem cell survival. Ongoing trials are also exploring sequencing approaches, biomarker-driven patient stratification, and strategies to mitigate toxicity while sustaining efficacy.
Taken together, venetoclax-based regimens represent a major advancement in AML therapy, offering meaningful survival gains and improved tolerability for patients previously considered untreatable with curative intent. However, their long-term impact remains tempered by resistance and relapse, underscoring the need for continued innovation. The evolving role of venetoclax is likely to be defined by its integration into combination and precision-based strategies that aim to transform AML from a largely fatal disease into a more manageable condition.
Keywords: Acute myeloid leukemia, venetoclax, BCL-2 inhibition, hypomethylating agents, resistance mechanisms, targeted therapy

Introduction
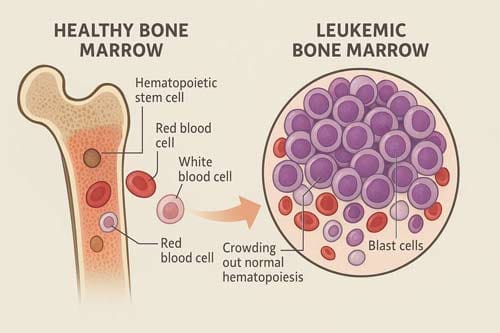
Acute myeloid leukemia (AML) represents one of the most challenging hematologic malignancies, with historically poor outcomes, particularly in older patients who comprise the majority of cases. For decades, intensive chemotherapy has been the frontline treatment for AML but has yielded only poor patient outcomes as exemplified by a 5-year survival rate of < 30%, even in younger adults [5]. The landscape of AML treatment underwent a drastic shift with the introduction of venetoclax, a selective BCL-2 inhibitor that targets the apoptotic machinery of malignant cells.
Venetoclax is a specific B-cell lymphoma-2 (BCL-2) inhibitor that can restore activation of apoptosis in malignancies, the survival of which depends on dysregulation of this pathway [6]. The development of venetoclax represented a breakthrough in precision medicine for AML, offering a targeted approach that diverged from the traditional cytotoxic chemotherapy model. As predicted by preclinical work, the use of venetoclax in the clinical setting has resulted in promising outcomes for patients with this disease, particularly when combined with hypomethylating agents or low-dose cytarabine in older patients with newly diagnosed AML who were not candidates for intensive induction chemotherapy [7].
The critical question facing the hematologic oncology community is whether venetoclax-based regimens represent a new standard of care that will endure or serve as an important but transitional step toward more definitive therapeutic solutions. This paper provides a comprehensive analytical examination of venetoclax-based therapy in AML, evaluating its clinical efficacy, real-world performance, resistance mechanisms, and future prospects within the broader context of evolving AML therapeutics.

Clinical Efficacy: The Foundation of a New Standard
The VIALE-A Paradigm
The pivotal VIALE-A trial established venetoclax in combination with azacitidine as a transformative therapy for treatment-naive AML patients ineligible for intensive chemotherapy. In VIALE-A, 431 patients were enrolled to venetoclax-azacitidine (n = 286) or placebo-azacitidine (n = 145). At 43.2 months median follow-up, median OS was 14.7 months with venetoclax-azacitidine, and 9.6 months with placebo-azacitidine [8]. The magnitude of survival benefit, with a hazard ratio of 0.66, represented one of the most vital advances in AML treatment for this patient population.
The incidence of complete remission was higher with azacitidine-venetoclax than with the control regimen (36.7% vs. 17.9%; P<0.001), as was the composite complete remission (complete remission or complete remission with incomplete hematologic recovery) (66.4% vs. 28.3%; P<0.001) [9]. These response rates were unprecedented for this patient population, establishing venetoclax-azacitidine as a new benchmark for treatment efficacy.
Real-World Validation
The translation of clinical trial results to real-world practice has been a critical test of venetoclax’s transformative potential. Multiple real-world studies have provided validation of the VIALE-A findings while revealing important nuances in clinical practice. Patients receiving venetoclax-azacitidine had a complete remission (CR)/CR with incomplete hematological recovery rate of 67%, day 30 and day 60 mortality of 5% and 8%, respectively, and median overall survival of 13.6 months [10] [11] in a large UK cohort, closely mirroring the trial results.
The REVIVE study, “to our knowledge, the first prospective study to demonstrate the effectiveness of venetoclax-containing therapy in the real world,” showed that “patient eligibility according to the VIALE-A registration trial criteria is associated with patient outcome in the clinic” [12]. This observation highlights an important distinction between trial populations and clinical practice, with median overall survival of 17.8 months for patients meeting VIALE-A eligibility criteria and 10.7 months for patients who did not (P = .027) [13].
Optimization of Treatment Regimens
Recognition of venetoclax’s myelosuppressive effects has led to efforts to optimize dosing and scheduling. The standard 28-day cycle of VEN is associated with a high degree of myelosuppression leading to treatment delays and dose modifications. Many small retrospective studies have successfully shown comparable outcomes to VIALE-A with reduced dose/duration of VEN. Furthermore, low dose metronomic dosing of HMA + VEN has shown clinical benefit while minimizing myelotoxicity [14].
These optimization efforts reflect the pragmatic challenges of implementing venetoclax-based therapy in clinical practice and suggest that the “standard” approach continues to evolve based on real-world experience.
Genetic Risk Stratification: Precision Medicine Challenges
Limitations of Traditional Risk Models
A key finding from venetoclax studies has been the inadequacy of traditional risk stratification systems when applied to patients receiving targeted therapy. ELN 2017 and 2022 prognostic classifiers did not adequately stratify OS outcomes for patients with AML treated with venetoclax-azacitidine. ELN prognostic classifiers did not provide clinically meaningful risk stratification of OS outcomes in patients treated with venetoclax-azacitidine [15] [16].
This finding has profound implications for clinical decision-making and suggests that venetoclax-based therapy may require entirely new prognostic frameworks. TP53, FLT3-ITD, NRAS, and KRAS mutation status allows the classification of these patients into 3 risk groups with distinct differences in median OS [17], pointing toward the need for therapy-specific risk stratification models.
Emerging Prognostic Models
The development of venetoclax-specific prognostic models represents a critical area of ongoing research. The mutational status of TP53, FLT3 internal tandem duplication (FLT3-ITD), NRAS, and KRAS categorized patients into higher-, intermediate-, and lower-benefit groups (52%, 25%, and 23% of patients, respectively), each associated with a distinct median OS (26.5 months, 12.1 months, and 5.5 months, respectively) [18].
This four-gene model illustrates how precision medicine approaches must evolve alongside therapeutic advances, suggesting that venetoclax-based regimens may be optimally effective only in specific genetic contexts.

Resistance Mechanisms: The Achilles’ Heel
Primary Resistance Patterns
Understanding resistance to venetoclax-based therapy is crucial for determining its long-term role in AML treatment. Mechanisms of resistance to venetoclax-based therapy include TP53 gene mutations or inactivation of p53 protein, activating kinase mutations such as FLT3 and RAS, and upregulation of other BCL-2 family apoptotic proteins [19].
The mechanistic basis for resistance reveals fundamental limitations in venetoclax’s approach to targeting AML. Responses to venetoclax +azacitidine in patients with AML correlate closely with developmental stage, where phenotypically primitive AML is sensitive, but monocytic AML is more resistant. Mechanistically, resistant monocytic AML has a distinct transcriptomic profile, loses expression of venetoclax target BCL2, and relies on MCL1 to mediate oxidative phosphorylation and survival [20].
Acquired Resistance Evolution
The evolution of resistance during treatment represents perhaps the most significant challenge to venetoclax’s role as a definitive therapy. Primitive leukemic clones displayed IMPDH2-high states linked to BCL2 inhibitor sensitivity, while resistant monocytic populations upregulated glycolysis and MCL1 to bypass BCL2 dependence [21].
Single tumors may consist of cells mimicking multiple resistance states contributing to intra-tumor heterogeneity [22], highlighting the complex and dynamic nature of resistance that develops during treatment.
Molecular Mechanisms of Resistance
At the molecular level, resistance to venetoclax involves multiple pathways beyond simple BCL-2 family protein alterations. The acquired resistance to venetoclax in human AML cell lines depends on NF-κB activation rather than on the upregulation of anti-apoptotic BCL2L1 expression [23] [24]. This finding suggests that resistance mechanisms may be more complex and targetable than initially anticipated.
Furthermore, protein analysis of resistant cells using immunoblotting demonstrated increased expression of MCL-1, a known resistance factor to VEN, in 4 resistant cell lines and BCL-XL increase in resistant cells [25], indicating that compensatory upregulation of alternative anti-apoptotic proteins represents a common resistance mechanism.
Real-World Outcomes: Promise and Limitations
Treatment Outcomes in Clinical Practice
Real-world data has provided both validation and sobering insights into venetoclax’s clinical impact. The overall response rate (ORR) was 69/105 (66%), was highest for patients with NPM1 (78%) and IDH1/2 (82%) mutations and lowest with TP53 mutations (40%). The median overall survival (OS) was 9.6 months, and 16.3 months for those achieving CR/CRi [26].
These outcomes, while encouraging, reveal significant heterogeneity in treatment response that depends heavily on molecular characteristics. Patients with FLT3-ITD/RAS or TP53 mutations had an inferior OS compared with the other patients (median OS 8.1, 1.7 and 16 months, respectively) [27], highlighting the limitations of a one-size-fits-all approach.
Temporal Trends in Outcomes
An important observation from real-world studies has been the improvement in outcomes over time, suggesting a learning curve in venetoclax implementation. Patients treated between 2022-24 had a lower early death rate (8% vs. 22%) and better OS (median 10.4 vs 5.8 mos, p = 0.033) than those treated between 2020-21 [28].
This temporal improvement likely reflects growing experience with supportive care, patient selection, and optimal dosing strategies, suggesting that venetoclax’s clinical impact may continue to improve with institutional experience.
Predictive Biomarkers and Ex Vivo Testing
The development of predictive biomarkers represents a critical advancement in optimizing venetoclax therapy. Ex vivo venetoclax sensitivity was the strongest predictor for a favorable treatment response and survival. This trial demonstrates the feasibility of integrating ex vivo drug testing into clinical practice to identify patients with AML, particularly in the R/R setting, who benefit from venetoclax [29].
Such personalized approaches may help address the heterogeneity in treatment response and optimize patient selection for venetoclax-based therapy.
Combination Strategies: Expanding the Therapeutic Window
Beyond Azacitidine: Alternative Combinations
While venetoclax-azacitidine has become the established standard, exploration of alternative combinations continues. In the 149 patients with NPM1 mutated AML, outcomes were similar for those treated with venetoclax-azacitidine and venetoclax-LDAC [30], suggesting that low-dose cytarabine may be an acceptable alternative in specific genetic contexts.
The exploration of venetoclax with intensive chemotherapy in younger, fit patients represents another frontier. Venetoclax in combination with intensive chemotherapy or doublets or triplets with targeted or immune therapies is the focus of numerous ongoing trials [31].
Overcoming Resistance Through Combinations
Recognition of resistance mechanisms has driven development of rational combination strategies. Co-treatment with SNDX-50469 and BCL2 inhibitor (venetoclax), or CDK6 inhibitor (abemaciclib) induces synergistic lethality in cell lines and patient-derived AML cells harboring MLL1-r or mtNPM1 [32].
However, early combination studies have shown mixed results. Venetoclax-cobimetinib showed limited preliminary efficacy similar to single-agent venetoclax, but with added toxicity. Our findings will inform future trials of BCL-2/MAPK pathway inhibitor combinations [33].
Emerging Alternatives: The Next Generation
Menin Inhibitors: A Targeted Approach
The development of menin inhibitors for specific AML subtypes represents a potentially innovative advance. Menin inhibitors are new and promising agents currently in clinical development that target the HOX/MEIS1 transcriptional program which is critical for leukemogenesis in histone-lysine N-methyltransferase 2A-rearranged (KMT2Ar) and in NPM1-mutated (NPM1mut) acute leukemias [34].
Revumenib demonstrated consistent efficacy across five pivotal trials, achieving MRD-negative rates of 70-90% in both KMT2A-rearranged and NPM1-mutated leukemias, leading to FDA approval in November 2024 [35]. This development suggests that highly targeted approaches may achieve superior outcomes in genetically defined subsets of AML.
Novel BCL-2 Family Inhibitors
Recognition of venetoclax resistance has spurred development of next-generation BCL-2 family inhibitors. Sonrotoclax effectively inhibits venetoclax-resistant BCL2 variants, such as G101V. The crystal structures revealed that sonrotoclax adopts a novel binding mode within the P2 pocket of BCL2 and could explain why sonrotoclax maintains stronger potency than venetoclax against the G101V mutant. Sonrotoclax emerges as a potential second-generation BCL2 inhibitor for the treatment of hematologic malignancies with the potential to overcome BCL2 mutation–induced venetoclax resistance [36].
Immunotherapeutic Approaches
The integration of immunotherapy with venetoclax-based regimens represents another promising avenue. Pre-clinical data support the development of CD64 CAR T cells for a planned phase I/II clinical trial for patients with post-Ven/Aza relapsed AML. These data suggest that CD64 CAR T cells can target venetoclax-resistant m-LSCs and support the development of a phase I/II clinical trial to test the safety of this potential salvage regimen for patients who relapse after Ven/Aza therapy [37] [38].
Future Perspectives: Evolution of AML Treatment
The Precision Medicine Paradigm
The venetoclax experience has accelerated the shift toward precision medicine in AML. The development of mutation-targeted therapies has greatly enhanced the treatment armamentarium, with FLT3 inhibitors and isocitrate dehydrogenase inhibitors improving outcomes in frontline and relapsed/refractory (RR) AML, and menin inhibitors showing efficacy in RR NPM1mut and KMT2A-rearranged AML [39].
This evolution suggests that the future of AML treatment may involve increasingly specific targeting based on molecular characteristics rather than broad-spectrum approaches.
Challenges in Implementation
Despite promising developments, significant challenges remain in implementing precision medicine approaches. Prognostic systems derived specifically for patients treated with venetoclax-azacitidine performed better than the European LeukemiaNet and Medical Research Council classifications; however, improved risk classifications are still required [40].
The need for therapy-specific prognostic models highlights the complexity of implementing precision medicine and suggests that the current venetoclax-based approach represents an intermediate step in treatment evolution.
Economic and Access Considerations
The sustainability of venetoclax-based therapy must also be considered within healthcare economic constraints. The drug’s cost, need for specialized monitoring, and requirement for extended treatment duration raise questions about long-term accessibility and healthcare system sustainability.
These practical considerations may influence the development and adoption of next-generation therapies, potentially favoring approaches that offer superior efficacy with reduced treatment burden.

Synthesis: Standard or Stepping Stone?
Evidence for New Standard Status
Several factors support venetoclax-based regimens as a new standard of care:
- Unprecedented efficacy: Venetoclax-azacitidine is approved for treatment of patients with newly diagnosed acute myeloid leukemia (AML) ineligible for intensive chemotherapy based on survival benefit. Long-term efficacy and safety confirm venetoclax-azacitidine is an improvement in standard-of-care for patients with AML who are not eligible for intensive chemotherapy [41] [42].
- Broad applicability: The treatment can be applied across diverse AML populations, with particular benefit in specific molecular subsets.
- Real-world validation: Multiple studies have confirmed the translation of trial benefits to clinical practice.
- Established infrastructure: Treatment protocols, monitoring systems, and supportive care measures are now well-established.
Evidence for Transitional Role
Conversely, several factors suggest venetoclax may represent a transitional solution:
- Universal resistance: Approximately 30% of AML patients fail to respond to venetoclax-based regimens and almost all treatment responders eventually relapse [43].
- Genetic limitations: ELN prognostic classifiers did not provide clinically meaningful risk stratification of OS outcomes in patients treated with venetoclax-azacitidine [44], suggesting fundamental limitations in broad applicability.
- Emerging alternatives: The rapid development of menin inhibitors and other targeted therapies suggests the field is moving toward more precise interventions.
- Resistance mechanisms: This differential sensitivity drives a selective process in patients which favors the outgrowth of monocytic subpopulations at relapse. We propose that optimal AML therapies should be designed so as to independently target AML subclones that may arise at differing stages of pathogenesis [45] [46].
Discussion
The question of whether venetoclax-based regimens represent a new standard or a temporary fix cannot be answered definitively, as the evidence supports elements of both perspectives. Venetoclax has undoubtedly transformed AML treatment, providing meaningful survival benefits and establishing new benchmarks for efficacy in older patients with AML. The consistency of results across clinical trials and real-world studies supports its role as a current standard of care.
However, the universal development of resistance, limitations in genetic applicability, and rapid emergence of potentially superior targeted therapies suggest that venetoclax-based regimens may represent an important but transitional phase in AML treatment evolution. The experience with venetoclax has provided crucial insights into precision medicine approaches while revealing the limitations of broadly applied targeted therapies.
The future likely lies in a more nuanced approach that incorporates venetoclax-based therapy as one component of an increasingly sophisticated treatment algorithm. Current clinical trials are exploring strategies such as doublet or triplet regimens incorporating a p53 activator, an anti-CD47 antibody, or other novel agents that target genes and proteins responsible for resistance to venetoclax. Further studies should focus on identifying predictive biomarkers of response to venetoclax-based therapy and incorporating immunotherapeutic approaches such as checkpoint inhibitors, bispecific antibodies, antibody-drug conjugates, and CAR T-cell therapy [47].
The venetoclax model has established important principles for AML treatment: the value of targeting specific cellular dependencies, the importance of combination approaches, and the need for therapy-specific prognostic models. These lessons will likely inform the development of next-generation treatments that may ultimately supersede venetoclax-based regimens.

Conclusion 
Conclusion
Venetoclax-based regimens in AML represent both a current standard of care and a stepping stone toward more sophisticated therapeutic approaches. The therapy has achieved unprecedented efficacy in previously untreatable patient populations, established new treatment models, and provided valuable insights into precision medicine in AML. However, universal resistance development, genetic limitations, and emerging targeted alternatives suggest that venetoclax-based therapy may serve as an important transitional phase rather than a permanent solution.
The true measure of venetoclax’s legacy may not be its durability as a standard therapy, but rather its role in catalyzing the precision medicine revolution in AML. By demonstrating the potential of targeted therapy while revealing its limitations, venetoclax has paved the way for increasingly sophisticated treatment approaches that promise to further transform AML care.
Future research should focus on optimizing patient selection through improved biomarkers, developing rational combination strategies to overcome resistance, and establishing therapeutic sequences that incorporate both current venetoclax-based approaches and emerging targeted therapies. The goal should be to maximize the benefit of venetoclax while preparing for its eventual integration into more comprehensive and effective treatment prototypes.
As the field continues to evolve, venetoclax-based regimens will likely be remembered as a pivotal advance that bridged the gap between traditional cytotoxic therapy and the precision medicine era, establishing principles that will guide AML treatment for years to come. Whether viewed as a new standard or a temporary fix, venetoclax has undeniably changed the trajectory of AML treatment and improved outcomes for thousands of patients worldwide.
References:
[1] A systematic review of venetoclax for the treatment of unfit AML patients in real-world: is all that glitters gold? – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/39150561/
[2] Azacitidine and Venetoclax in Previously Untreated Acute Myeloid Leukemia – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32786187/
[3] Genetic risk stratification and outcomes among treatment-naive patients with AML treated with venetoclax and azacitidine – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/39133921/
[4] Mechanisms of Acquired Resistance to Venetoclax in Preclinical AML Models – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S0006497118473077
[5] Venetoclax for AML: changing the treatment paradigm – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31869416/
[6] Venetoclax for AML: changing the treatment paradigm – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31869416/
[7] Venetoclax for AML: changing the treatment paradigm – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31869416/
[8] Azacitidine and Venetoclax in Previously Untreated Acute Myeloid Leukemia – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32786187/
[9] Genetic risk stratification and outcomes among treatment-naive patients with AML treated with venetoclax and azacitidine – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/39133921/
[10] Real-world outcomes of newly diagnosed AML treated with venetoclax and azacitidine or low-dose cytarabine in the UK NHS – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S2950328024000177
[11] Real-world outcomes of newly diagnosed AML treated with venetoclax and azacitidine or low-dose cytarabine in the UK NHS – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S2950328024000177
[12] Trial eligibility, treatment patterns, and outcome for venetoclax-based therapy in AML: a prospective cohort study – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S2473952924007080
[13] Trial eligibility, treatment patterns, and outcome for venetoclax-based therapy in AML: a prospective cohort study – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S2473952924007080
[14] Ven the dose matters: Venetoclax dosing in the frontline treatment of AML – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/39217050/
[15] Genetic risk stratification and outcomes among treatment-naive patients with AML treated with venetoclax and azacitidine – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S0006497124021980
[16] Genetic risk stratification and outcomes among treatment-naive patients with AML treated with venetoclax and azacitidine – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S0006497124021980
[17] Genetic risk stratification and outcomes among treatment-naive patients with AML treated with venetoclax and azacitidine – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S0006497124021980
[18] Genetic risk stratification and outcomes among treatment-naive patients with AML treated with venetoclax and azacitidine – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S0006497124021980
[19] Dynamic evolution of venetoclax resistance in acute myeloid leukemia unveiled by longitudinal single-cell RNA-seq – ScienceDirect –https://www.sciencedirect.com/science/article/abs/pii/S0304383525004203
[20] Transcriptional and phenotypic heterogeneity underpinning venetoclax resistance in AML – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/38352538/
[21] Venetoclax therapy and emerging resistance mechanisms in acute myeloid leukaemia – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/38866760/
[22] Resistance to venetoclax and hypomethylating agents in acute myeloid leukemia – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33796823/
[23] Acute myeloid leukemia resistant to venetoclax-based therapy: What does the future hold? – ScienceDirect –https://www.sciencedirect.com/science/article/abs/pii/S0268960X22001102
[24] Acute myeloid leukemia resistant to venetoclax-based therapy: What does the future hold? – ScienceDirect –https://www.sciencedirect.com/science/article/abs/pii/S0268960X22001102
[25] Mechanisms for resistance in AML insights into molecular pathways mediating resistance to venetoclax – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/33762105/
[26] A Real-World Evaluation of Frontline Treatment for Acute Myeloid Leukemia With Azacitidine Plus Venetoclax – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S2152265025000527
[27] A Real-World Evaluation of Frontline Treatment for Acute Myeloid Leukemia With Azacitidine Plus Venetoclax – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S2152265025000527
[28] A Real-World Evaluation of Frontline Treatment for Acute Myeloid Leukemia With Azacitidine Plus Venetoclax – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S2152265025000527
[29] Design of the VIALE-M phase III trial of venetoclax and oral azacitidine maintenance therapy in acute myeloid leukemia – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/35852098/
[30] Real-world outcomes of newly diagnosed AML treated with venetoclax and azacitidine or low-dose cytarabine in the UK NHS – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S2950328024000177
[31] Venetoclax and Cobimetinib in Relapsed/Refractory AML: A Phase 1b Trial – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S2152265024000363
[32] Menin inhibitors in the treatment of acute myeloid leukemia – ScienceDirect –https://www.sciencedirect.com/science/article/abs/pii/S0006497124114504
[33] Refined ELN 2024 risk stratification improves survival prognostication following venetoclax-based therapy in AML – ScienceDirect –https://www.sciencedirect.com/science/article/abs/pii/S0006497124108841
[34] Menin Inhibitors in Acute Myeloid Leukemia-What Does the Future Hold? – PubMed – pubmed.ncbi.nlm.nih.govhttps://pubmed.ncbi.nlm.nih.gov/35072375/
[35] Targeted therapy in NPM1-mutated AML: Knowns and unknowns – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36237321/
[36] Acute myeloid leukemia resistant to venetoclax-based therapy: What does the future hold? – ScienceDirect –https://www.sciencedirect.com/science/article/abs/pii/S0268960X22001102
[37] Venetoclax plus cytarabine and azacitidine in relapsed/refractory AML: An open-label, single-arm, phase 2 study – ScienceDirect –https://www.sciencedirect.com/science/article/abs/pii/S0959804924001357
[38] Venetoclax plus cytarabine and azacitidine in relapsed/refractory AML: An open-label, single-arm, phase 2 study – ScienceDirect –https://www.sciencedirect.com/science/article/abs/pii/S0959804924001357
[39] Venetoclax and Cobimetinib in Relapsed/Refractory AML: A Phase 1b Trial – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S2152265024000363
[40] Real-world outcomes of newly diagnosed AML treated with venetoclax and azacitidine or low-dose cytarabine in the UK NHS – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S2950328024000177
[41] Azacitidine and Venetoclax in Previously Untreated Acute Myeloid Leukemia – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32786187/
[42] Azacitidine and Venetoclax in Previously Untreated Acute Myeloid Leukemia – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32786187/
[43] Mechanisms of Acquired Resistance to Venetoclax in Preclinical AML Models – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S0006497118473077
[44] Genetic risk stratification and outcomes among treatment-naive patients with AML treated with venetoclax and azacitidine – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S0006497124021980
[45] Transcriptional and phenotypic heterogeneity underpinning venetoclax resistance in AML – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/38352538/
[46] Transcriptional and phenotypic heterogeneity underpinning venetoclax resistance in AML – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/38352538/
[47] Genetic risk stratification and outcomes among treatment-naive patients with AML treated with venetoclax and azacitidine – ScienceDirect –https://www.sciencedirect.com/science/article/pii/S0006497124021980

