Thrombocytopenia in the ICU: Essential Guide for Clinical Hematologists
Please like and subscribe if you enjoyed this video 🙂
Introduction
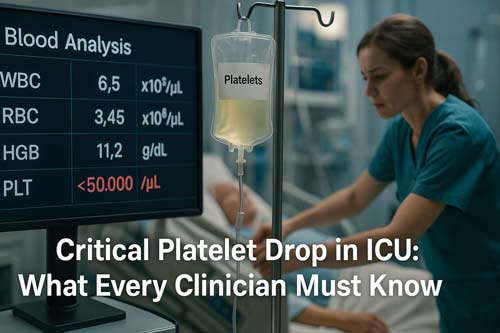
Thrombocytopenia is a frequent hematologic abnormality in critically ill patients, affecting up to 67.6% at ICU admission, with an additional 14–44% developing it during their stay. It serves as a sensitive marker of physiological stress and is associated with major clinical implications.
Thrombocytopenia in the ICU is linked to increased bleeding risk and higher mortality. Major bleeding occurs in 20% of thrombocytopenic patients compared to 13% of those with normal platelet counts. Mortality rates are also markedly higher; 33% in thrombocytopenic patients versus 16% in non-thrombocytopenic counterparts.
The timing and duration of thrombocytopenia carry important prognostic value. In septic shock, platelet counts typically begin to decline around day 2 post-admission and persist for a median of 6 days in survivors. Persistent thrombocytopenia beyond 14 days correlates with a mortality rate of 66%, compared to 16% in patients whose platelet counts recover.
Severity is graded as:
- Mild: 100–149 × 10⁹/L
- Moderate: 50–99 × 10⁹/L
- Severe: <50 × 10⁹/L
Severe thrombocytopenia occurs in 1.6–20% of ICU patients.
Multiple mechanisms contribute to thrombocytopenia in critical illness:
- Decreased production (e.g., bone marrow suppression)
- Increased destruction (e.g., immune-mediated causes)
- Consumption (e.g., disseminated intravascular coagulation)
- Sequestration (e.g., splenomegaly)
- Dilution (e.g., massive transfusion or fluid resuscitation)
Sepsis is the most common cause, responsible for nearly 50% of cases. However, other etiologies include drug-induced thrombocytopenia, thrombotic microangiopathies, and heparin-induced thrombocytopenia (HIT).
Accurate diagnosis relies on clinical context and targeted investigations:
- Initial workup: CBC with smear, coagulation profile, renal and liver function tests
- Specific tools: The 4T score is useful in assessing the likelihood of HIT.
- Further testing: May include HIT antibody assays, ADAMTS13 activity (if TTP is suspected), or bone marrow evaluation in selected cases.
Management focuses on:
- Treating the underlying cause (e.g., infection, drug withdrawal)
- Minimizing bleeding risk (e.g., platelet transfusions in high-risk or actively bleeding patients)
- Monitoring trends rather than isolated platelet counts
- Avoiding unnecessary interventions in stable, non-bleeding patients
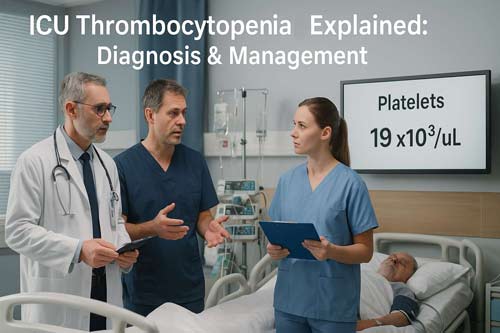
Platelet transfusion thresholds vary based on bleeding risk and procedure needs. In general:
- <10 × 10⁹/L: Transfuse regardless of symptoms
- <20 × 10⁹/L: Transfuse if febrile or septic
- <50 × 10⁹/L: Consider transfusion before invasive procedures
Thrombocytopenia in the ICU is both common and clinically notable, offering valuable insight into a patient’s physiological status and prognosis. Understanding its timing, severity, and underlying causes is essential for effective diagnosis and management. A structured, evidence-based approach can improve outcomes and guide appropriate use of interventions in critically ill patients.

Epidemiology and Clinical Impact of ICU Thrombocytopenia
The epidemiological profile of thrombocytopenia varies considerably across different intensive care settings, with major implications for patient outcomes. A closer examination reveals the scope, consequences, and prognostic value of this common hematologic abnormality in critically ill patients.
Prevalence across ICU populations
Large-scale studies demonstrate that thrombocytopenia affects between 8.3% to 67.6% of patients upon ICU admission, with an additional 14% to 44% developing this condition during their ICU stay. The substantial variation in reported prevalence reflects differences in patient populations, ICU specialties, and defining thresholds. The recent prospective international PLOT-ICU cohort study, which included 1168 patients from 52 ICUs across 10 countries, reported an overall thrombocytopenia frequency of 43.2%, with 23.4% present at baseline and 19.8% acquired during ICU admission.
The prevalence exhibits distinctive patterns across ICU specialties:
- Medical ICUs: approximately 20% of patients
- Surgical ICUs: approximately 35% of patients
- Trauma ICUs: approximately 45% of patients
In the PROTECT trial, new-onset thrombocytopenia was categorized by severity, with mild (100-149 × 10^9/L) affecting 15.3%, moderate (59-99 × 10^9/L) affecting 5.1%, and severe (<50 × 10^9/L) affecting 1.6% of patients. Remarkably, risk factors consistently associated with ICU-acquired thrombocytopenia include severity of illness, organ dysfunction, sepsis, vasopressor use, and renal failure.
Association with mortality and bleeding risk
The presence of thrombocytopenia strongly correlates with adverse outcomes. Patients with thrombocytopenia exhibit markedly higher mortality rates; 33% versus 16% in non-thrombocytopenic patients. Furthermore, this relationship follows a dose-response pattern, with more severe thrombocytopenia associated with worse outcomes. In one large-scale analysis, the crude odds ratio for mortality was 5.0 (95% CI 2.7–9.1) in thrombocytopenic patients. Additionally, patients who develop thrombocytopenia after ICU admission face a mortality rate of 31.9%, with an odds ratio of 4.6 (95% CI 2.1–10.0).
Bleeding complications increase dramatically with declining platelet counts. The incidence of bleeding rises from 4.1% in non-thrombocytopenic patients to 21.4% in those with mild thrombocytopenia and 51.9% in patients with platelet counts below 100 × 10^9/L. Particularly concerning is that 57.6% of bleeding episodes in thrombocytopenic patients are severe or debilitating (WHO grade 3 or 4), whereas non-thrombocytopenic patients mostly experience milder bleeding. The median platelet count during grade 3 or 4 bleeding was reported as 23 × 10^9/L.
Besides mortality and bleeding, thrombocytopenia correlates with:
- Increased transfusion requirements
- Extended ICU and hospital length of stay
- Greater need for organ support, including vasopressors (73% vs 45.8%), mechanical ventilation (63.3% vs 44.6%), and renal replacement therapy (25% vs 5.3%)
Platelet trajectory as a prognostic marker
The dynamic evolution of platelet counts throughout ICU stay provides valuable prognostic information beyond single-point measurements. After admission, platelet counts typically decrease, reaching their lowest point (nadir) around day 4-5. Analysis of these patterns reveals three distinct trajectories:
First, the descending pattern (DS) represents patients whose platelet counts decline rapidly from a high baseline. These patients face the poorest prognosis, with a hazard ratio for mortality of 1.58 (95% CI: 1.40–1.79) compared to the ascending pattern. Second, the ascending pattern (AS) characterizes patients with low baseline counts that recover quickly, associated with better outcomes. Finally, the stable pattern (ST) describes patients maintaining consistently low platelet counts, with intermediate prognosis (HR: 1.26, 95% CI: 1.14–1.38).
Especially notable is that persistent thrombocytopenia beyond 14 days correlates with a 66% mortality rate, versus only 16% in patients whose platelet counts normalize. Moreover, the rate of recovery itself serves as a prognostic indicator—survivors typically show an average increase of 30 × 10^9/L per day, while non-survivors demonstrate increases of ≤6 × 10^9/L per day.
Interestingly, thrombocytopenia mediates approximately 27.2% of the effects of platelet trajectory on 28-day mortality. This relationship maintains significance even in patients who never develop thrombocytopenia by conventional definitions, indicating that relative changes in platelet counts, rather than absolute values alone, provide essential prognostic information.
Mechanisms of Thrombocytopenia in Critical Illness
Thrombocytopenia in critical illness results from multiple pathophysiological processes that often coexist in the same patient. Understanding these mechanisms is essential for accurate diagnosis and effective management. The complex interplay between decreased production, increased destruction, consumption, sequestration, and dilution determines the severity and clinical implications of platelet count reduction.
Decreased production: marrow suppression and chemotherapy
Diminished platelet production represents a fundamental mechanism of thrombocytopenia in the ICU. Although inflammatory cytokines typically stimulate thrombopoiesis (unlike their inhibitory effect on erythropoiesis), several factors can impair megakaryocyte function and platelet production:
- Chemotherapy and radiation: Cytotoxic agents directly damage megakaryocyte precursors, leading to severe thrombocytopenia in 10-68% of patients with solid tumors or hematological cancers
- Viral infections: HIV, HCV, EBV, CMV, and parvovirus can suppress bone marrow function
- Alcohol toxicity: Acute alcohol intoxication causes direct bone marrow suppression
- Nutritional deficiencies: Vitamin B12 and folate deficiencies impair megakaryopoiesis
- Bone marrow infiltration: Leukemia, tumors, or fibrosis can displace normal hematopoietic tissue
Trauma patients exhibit profound bone marrow dysfunction characterized by decreased bone marrow cellularity (4.7 million cells/ml compared to 16.7 million cells/ml in healthy controls). Despite elevated thrombopoietin levels, trauma patients show reduced erythroid progenitor growth with 39.0 colonies per plate versus 66.5 in healthy controls.
Increased destruction: immune and non-immune causes
Platelet destruction occurs through both immune and non-immune mechanisms. Immune-mediated destruction involves antibody-dependent cellular phagocytosis, complement-dependent cytotoxicity, and direct cytotoxic T-lymphocyte attack. Platelet-associated IgG antibodies are present in 30-40% of septic patients, contributing to accelerated clearance.
Non-immune destruction can result from physical damage to platelets. Extracellular histones released during cellular injury induce platelet aggregation and destruction. These histones originate from neutrophil extracellular traps (NETs) and correlate with thrombocytopenia severity.
ADAMTS13 depletion represents another critical mechanism. This metalloproteinase normally cleaves large von Willebrand factor (vWF) multimers. In cirrhosis and sepsis, ADAMTS13 levels decline, allowing accumulation of vWF multimers that enhance shear-stress induced platelet aggregation.
Consumption: DIC, sepsis, trauma
Consumption coagulopathy constitutes a major cause of thrombocytopenia in critically ill patients. In sepsis, which accounts for approximately 50% of all ICU thrombocytopenias, multiple consumption mechanisms operate simultaneously:
Thrombin generation activates platelets extensively, causing them to adhere to damaged endothelium and form microthrombi. This process, termed immunothrombosis, serves a physiological role in preventing pathogen dissemination but can become pathological in severe sepsis.
Disseminated intravascular coagulation (DIC) develops in 9-19% of ICU patients with thrombocytopenia. DIC involves widespread activation of coagulation with intravascular fibrin formation and microvascular thrombosis, consequently depleting platelets and coagulation factors.
In trauma, platelets exhibit qualitative dysfunction despite initially normal counts. Nevertheless, post-injury, platelets show balloon-like morphology and increased circulating platelet extracellular vesicles. Furthermore, trauma-induced coagulopathy triggers enhanced platelet consumption, with platelet counts progressively falling by 24 hours post-injury.
Sequestration: splenomegaly and liver disease
Splenic sequestration accounts for a substantial proportion of thrombocytopenia cases, particularly in patients with hepatic disease. Physiologically, approximately 30% of platelets are sequestered in the spleen. However, with splenomegaly, this percentage can increase to 90%.
In liver cirrhosis, thrombocytopenia results from both sequestration and decreased thrombopoietin production. Portal hypertension causes redistribution of splanchnic venous blood flow, leading to splenic congestion and enlargement. Consequently, a greater proportion of platelets become trapped in the enlarged spleen.
Dilutional thrombocytopenia from massive transfusion
Dilutional thrombocytopenia occurs following massive transfusion, defined as replacement of more than total blood volume within 24 hours. This results from both platelet loss during hemorrhage and dilution with transfused red cells and crystalloids.
Prior to the advent of modern blood banking practices, 75% of patients receiving 20 or more red blood cell units developed platelet counts below 50,000/μL. Currently, severe thrombocytopenia rarely occurs before replaced volume surpasses 150% of total blood volume.
Automated blood cell counters now enable rapid platelet count monitoring, allowing earlier intervention. Platelet transfusion is typically considered when counts fall below 50,000/mm³. Nevertheless, despite improved management protocols, excessive platelet transfusion has emerged as a new concern in massive transfusion scenarios.
Diagnostic Framework for ICU Thrombocytopenia
Establishing a systematic diagnostic approach to thrombocytopenia in critically ill patients requires evaluation across multiple time frames and diagnostic modalities. Accurate diagnosis facilitates appropriate management and helps predict clinical outcomes.
Stepwise evaluation: past, present, future platelet trends
A comprehensive diagnostic framework for thrombocytopenia in the ICU centers around three critical time frames. First, examining the past involves assessing pre-ICU platelet counts, medical history, comorbidities, and medications. Obtaining previous complete blood counts helps determine whether thrombocytopenia existed before critical illness or developed acutely. Second, analyzing the present requires tracking the platelet trajectory in relation to clinical course. Different patterns yield valuable diagnostic clues:
- Platelets low at presentation with persistent depression suggests independent causes like marrow failure
- Immediate fall with quick recovery typically follows major surgery or massive transfusion
- Gradual decline within the first few days with recovery paralleling clinical improvement indicates sepsis or inflammatory conditions
- Continued depression despite clinical improvement raises suspicion for iatrogenic causes
Third, predicting the future trajectory guides monitoring and intervention strategies. The severity of thrombocytopenia and presence of thrombosis provide additional diagnostic insights. Severe thrombocytopenia (<20 × 10^9/L) narrows the differential to profound bone marrow failure, overt DIC, or immune-mediated destruction.
Peripheral smear findings: schistocytes, blasts, clumps
Peripheral blood smears offer vital diagnostic information that automated counters cannot provide. Hence, examining blood smears becomes essential in the initial evaluation of thrombocytopenia. Key findings include:
- Platelet clumps suggesting pseudothrombocytopenia (false low count)
- Schistocytes (red cell fragments) indicating microangiopathy in TTP or DIC
- Blasts pointing toward acute leukemia
- Teardrops and nucleated red cells suggesting marrow infiltration
- Giant platelets indicating peripheral destruction mechanisms
Importantly, pseudothrombocytopenia occurs in 0.1-2% of hospitalized patients due to EDTA-induced platelet agglutination. This laboratory artifact can lead to unnecessary interventions if unrecognized. When suspected, repeating counts in citrate tubes often resolves the issue, though up to 17% of EDTA-dependent pseudothrombocytopenia also occurs with citrate.
Role of bone marrow biopsy in unclear cases
Bone marrow examination provides unique insights into megakaryocyte quantity and morphology. While often considered, studies question its routine use in ICU thrombocytopenia. A prospective study of 208 critically ill thrombocytopenic patients found that bone marrow aspirates yielded new information in only 22% of cases and changed management in merely 9%.
Current guidelines recommend bone marrow evaluation primarily when:
- The cause remains unclear after initial workup
- Multiple cell lines are affected
- Clinical suspicion of hematologic malignancy exists
- Platelet counts fail to recover as expected
When performed, aspirates typically reveal megakaryocytes in 93% of ICU patients with thrombocytopenia, indicating peripheral consumption mechanisms predominate. Hemophagocytosis, often associated with sepsis and transfusions, appears in bone marrow of approximately 26.3% of ICU patients with thrombocytopenia.
Use of MPV and platelet indices in differential
Mean platelet volume (MPV) and other platelet indices offer additional diagnostic value. MPV reflects platelet size and activation status, with normal range between 9.5-12.7 fL. Elevated MPV suggests consumptive thrombocytopenia with increased platelet turnover, as younger platelets are typically larger. Conversely, reduced MPV points toward impaired bone marrow production.
Beyond diagnostic applications, MPV demonstrates prognostic value. Multiple studies found MPV >11.4 fL independently predicts increased mortality (adjusted HR 2.640, 95% CI 1.208-5.767). Furthermore, the trajectory of MPV provides superior prognostic information compared to single measurements. Increasing MPV from baseline correlates with higher mortality, particularly when ΔMPV exceeds 0.8-0.9 fL by the third day.
Additional platelet indices including platelet distribution width (PDW) and plateletcrit (PCT) further refine the diagnostic picture. Descending platelet count and PCT trajectories alongside ascending PDW patterns correlate with increased 90-day mortality. Thus, integrating these readily available indices enhances both diagnostic accuracy and prognostic assessment in ICU thrombocytopenia.
Thrombocytopenia in Sepsis and Systemic Inflammation
Sepsis-induced thrombocytopenia represents one of the most complex and frequent causes of platelet depletion in the ICU. Platelets interact with diverse inflammatory and coagulation pathways, creating a bidirectional relationship where inflammation promotes thrombocytopenia while platelet depletion further aggravates systemic inflammation.
Thrombin generation and DIC in septic shock
Thrombin stands as a central mediator in sepsis pathophysiology. In septic patients, excessive thrombin production results from tissue factor upregulation on activated endothelial cells and monocytes. This process leads to disseminated intravascular coagulation (DIC), which occurs in up to 80% of sepsis patients. The resulting microthrombi form predominantly in smaller vessels, causing organ damage and circulatory collapse.
Calibrated automated thrombography reveals distinct patterns in severe infection. Patients with higher Sequential Organ Failure Assessment (SOFA) scores demonstrate longer lag time (5.2 vs. 4.3 min) and reduced endogenous thrombin potential (1834 vs. 2015 nM*min). Furthermore, non-survivors exhibit lower thrombin peak values (284 vs. 345 nM) compared to survivors, suggesting thrombin generation parameters hold prognostic value.
ADAMTS13 depletion and microvascular injury
ADAMTS13 (A Disintegrin and Metalloprotease with ThromboSpondin type 1 motif, member 13) plays a crucial role in regulating platelet adhesion by cleaving ultralarge von Willebrand factor (vWF) multimers. Septic patients exhibit markedly reduced ADAMTS13 activity compared to those with non-infectious systemic inflammatory response syndrome (P = 0.014). Even moderately decreased ADAMTS13 activities (<50%) correlate with:
- Platelet depletion
- Development of DIC
- Increased need for fresh frozen plasma transfusion
In fact, ADAMTS13 activity <30% independently predicts hospital mortality (odds ratio 11.86; 95% CI 1.36 to 103.52). This depletion allows accumulation of ultralarge vWF multimers, enhancing platelet adhesion to damaged endothelium and subsequent sequestration in microvasculature.
Hemophagocytosis and cytokine storm
Hemophagocytosis—characterized by unrestrained activation of macrophages that phagocytose blood cells—represents another thrombocytopenia mechanism in sepsis. Remarkably, hemophagocytosis appears in 64% of ICU patients with sepsis and thrombocytopenia. The presence of bone marrow hemophagocytosis strongly predicts mortality (OR = 5.27 [1.11–24.97]).
This process closely connects with cytokine storm syndrome, where hyperinflammation drives coagulopathy and thrombocytopenia. Elevated inflammatory markers (particularly IL-6) demonstrate a stepwise increase with coagulation abnormalities—median IL-6 concentration rising from 78 pg/mL in mild cases to 1835 pg/mL in severe cases. Essentially, IL-6 may directly inhibit ADAMTS13 activity, establishing a mechanistic link between cytokine storm and thrombocytopenia.
Complement activation and platelet destruction
The complement system emerges as a fundamental contributor to sepsis-associated thrombocytopenia. C5a, a potent anaphylatoxin released during complement activation, transforms endothelium from antiadhesive to proadhesive for inflammatory cells. C5a likewise stimulates tissue factor expression on neutrophils and induces the release of neutrophil extracellular traps (NETs).
Beyond direct effects, complement activation amplifies thrombocytopenia through crosstalk with coagulation pathways. The membrane attack complex (C5b-9) induces endothelial vesiculation with prothrombinase activity. Subsequently, these prothrombotic microvesicles disseminate throughout circulation, augmenting the hypercoagulable state and accelerating platelet consumption.
Treatment Strategies and Transfusion Thresholds
Managing thrombocytopenia requires a balanced approach between treating underlying pathologies and providing supportive care. The appropriate platelet transfusion strategy hinges on clinical context, bleeding risk, and procedural requirements.
Treating the underlying cause vs symptomatic management
The cornerstone of thrombocytopenia management involves identifying and addressing the primary etiology. In sepsis-induced thrombocytopenia, source control and appropriate antibiotic therapy take precedence. For DIC, treating the inciting disorder remains essential, while other measures serve as supportive care. Nonetheless, platelet transfusions often become necessary when severe thrombocytopenia persists despite addressing underlying causes.
Therapeutic platelet transfusion: WHO grade ≥2 bleeding
Active bleeding mandates immediate intervention. Clinicians should transfuse platelets when bleeding reaches WHO grade 2 or higher in thrombocytopenic patients. Current guidelines recommend:
- Platelet counts <50 × 10^9/L with serious active bleeding
- Higher thresholds (100 × 10^9/L) for intracranial hemorrhage or traumatic brain injury
- Early platelet administration in massive bleeding, particularly in trauma
In the SPRINT trial, bleeding grades decreased following only 21% of therapeutic platelet transfusions, remained unchanged after 69%, and increased after 10%. This highlights the multifactorial nature of bleeding beyond simple platelet counts.
Prophylactic transfusion: <10 × 10^9/L or procedural need
For stable non-bleeding patients, prophylactic transfusion thresholds vary by clinical scenario:
- <10 × 10^9/L for patients without high bleeding risk
- <30-50 × 10^9/L for those at high risk of spontaneous bleeding
- ≥50 × 10^9/L before major surgery or invasive procedures
- ≥20 × 10^9/L before central venous catheter placement
Ultrasound guidance has reduced procedural bleeding risk, allowing lower platelet thresholds for interventions. Indeed, retrospective studies suggest safe ultrasound-guided CVC placement even with platelet counts <20 × 10^9/L.
Platelet refractoriness and HLA-matched transfusions
Platelet refractoriness—inadequate count increment after transfusion—affects 54.8% of ICU patients receiving platelet transfusions. Primarily, this results from immune (anti-HLA antibodies) or non-immune causes (sepsis, splenomegaly, medications).
For immunized refractory patients, HLA-matched platelets provide superior outcomes. These achieve higher median 14-hour corrected count increments (5643) compared to random units (1683). Alternatively, HLA epitope-matched platelets present a viable option when full antigen matching proves impossible. Younger age, non-trauma admission, and increased spleen size correlate with higher refractoriness risk.
Special Considerations: HIT, TTP, and Drug-Induced Cases
Among the myriad causes of thrombocytopenia in critically ill patients, certain conditions demand specialized diagnostic approaches and tailored interventions due to their unique pathophysiology and management requirements.
Heparin-induced thrombocytopenia: 4T score and PF4 testing
Heparin-induced thrombocytopenia (HIT) is uncommon yet potentially devastating, affecting approximately 0.4% of critically ill patients. The 4Ts score—evaluating Thrombocytopenia, Timing, Thrombosis, and oTher causes—provides a reliable pretest probability assessment. Patients with low 4Ts scores (≤3) rarely have positive serotonin release assays, making HIT highly unlikely. Accordingly, a low score occurred in 78% of patients investigated for HIT, none of whom had a positive SRA.
Diagnostic confirmation requires:
- Anti-PF4/heparin antibody testing (ELISA) as initial screening
- Functional assays (serotonin release assay) as the gold standard for confirmation
Unfractionated heparin poses a 10-fold higher risk than low-molecular-weight heparin. Upon suspicion of HIT, all heparin products must be discontinued and alternative anticoagulation initiated.
Thrombotic microangiopathies: TTP, HUS, HELLP
Thrombotic microangiopathies present with microangiopathic hemolytic anemia, thrombocytopenia, and organ dysfunction. Thrombotic thrombocytopenic purpura (TTP) is distinguished by ADAMTS13 activity <10%, whereas complement-mediated HUS features predominantly renal involvement with normal or slightly reduced ADAMTS13.
HELLP syndrome, typically occurring in the third trimester, presents with hemolysis, elevated liver enzymes, and low platelets. Unlike TTP, hypertension and proteinuria generally accompany HELLP. Differentiation between these entities is key since treatment differs dramatically; plasma exchange for TTP, eculizumab for atypical HUS, and delivery for HELLP syndrome.
Drug-induced immune thrombocytopenia: common culprits
Drug-induced immune thrombocytopenia (DITP) affects up to 25% of acutely ill patients. Typically, platelets decrease precipitously 5-14 days after medication initiation. Common culprits include:
- Glycoprotein IIb/IIIa inhibitors (abciximab, tirofiban)
- Antibiotics (vancomycin, trimethoprim/sulfamethoxazole, ceftriaxone)
- Quinine/quinidine
- NSAIDs and anticonvulsants
Diagnosis requires temporal association with drug administration, recovery after discontinuation, and exclusion of alternative causes. Alongside direct antibody-mediated destruction, some medications like platinum compounds may cause acute immune thrombocytopenia beyond their known myelosuppressive effects.
Post-transfusion purpura and alloimmune causes
Post-transfusion purpura (PTP) is characterized by severe thrombocytopenia 5-10 days following blood transfusion. This rare reaction occurs predominantly in females (85%) with prior sensitization through pregnancy or transfusion. Anti-HPA-1a antibodies represent the most common causative agent (81%), followed by HPA-1b, HPA-5b, and HPA-3a.
PTP produces profound thrombocytopenia (typically <10 × 10^9/L) with serious bleeding complications. Death occurs in 9% of cases. Treatment includes intravenous immunoglobulin, corticosteroids, and occasionally plasmapheresis, yielding adequate response in 83% of cases.
Conclusion
Thrombocytopenia is a common finding in critically ill patients, affecting up to 67.6% upon ICU admission, with an additional 14–44% developing it during their stay. Its impact extends far beyond abnormal lab values—patients with thrombocytopenia experience twice the mortality risk, increased rates of major bleeding, and greater healthcare resource utilization compared to those with normal platelet counts.
Platelet dynamics provide critical prognostic insight. Clinicians should monitor not only absolute platelet counts but also trends in decline and recovery. Three core principles should guide evaluation:
- Multifactorial etiology: Most cases arise from a combination of factors, including infection, medications, and organ dysfunction.
- Dynamic progression: Platelet counts evolve with disease severity and response to treatment.
- Systemic implications: Thrombocytopenia reflects and contributes to broader physiologic instability, including organ dysfunction.
A thorough diagnostic workup requires integration of clinical context over time. Peripheral blood smears remain essential, offering diagnostic clues that automated counters may miss. Bone marrow examination should be reserved for cases with unclear etiology. Platelet indices such as mean platelet volume (MPV) may also provide added value without additional cost or risk.
Although sepsis is the leading cause, accounting for nearly half of ICU-associated thrombocytopenia, other serious etiologies must be considered:
- Heparin-induced thrombocytopenia (HIT)
- Thrombotic microangiopathies (e.g., TTP, HUS)
- Drug-induced thrombocytopenia
Timely recognition of these conditions is important, as misdiagnosis can lead to inappropriate and potentially harmful interventions.
Treatment involves addressing the underlying cause while providing supportive care. Current transfusion guidelines recommend a restrictive approach in the absence of active bleeding:
- <10 × 10⁹/L: Prophylactic transfusion in stable, non-bleeding patients
- 30–50 × 10⁹/L: For patients with increased bleeding risk
- Procedure-specific thresholds: Adjusted based on the type of intervention and individual risk
- Active bleeding: Immediate transfusion regardless of count
In cases of platelet refractoriness, especially due to alloimmunization, HLA-matched platelets may be required. Furthermore, clinicians must weigh both bleeding and thrombotic risks when considering transfusion, particularly in conditions like HIT, where platelet transfusion may exacerbate thrombosis.
Thrombocytopenia in the ICU is not just a hematologic abnormality; it is a dynamic marker of critical illness and a key prognostic indicator. Optimal management requires a systematic, multidisciplinary approach that integrates evolving clinical data, recognizes life-threatening etiologies, and applies evidence-based transfusion strategies. For hematologists and intensivists alike, a nuanced understanding of thrombocytopenia is essential to improving outcomes in this vulnerable patient population.
Frequently Asked Questions:
FAQs
Q1. What is the most common cause of thrombocytopenia in ICU patients? Sepsis is the most common cause, accounting for approximately 50% of thrombocytopenia cases in critically ill patients. Other frequent causes include trauma, massive transfusion, and drug-induced thrombocytopenia.
Q2. How does thrombocytopenia impact patient outcomes in the ICU? Thrombocytopenia significantly increases mortality risk, with thrombocytopenic patients having a 33% mortality rate compared to 16% in non-thrombocytopenic patients. It also increases the risk of major bleeding and is associated with longer ICU stays and greater need for organ support.
Q3. What are the key diagnostic steps for evaluating thrombocytopenia in ICU patients? Evaluation should include examining past platelet counts, assessing present trends, and predicting future trajectories. A peripheral blood smear is crucial for identifying specific abnormalities. In unclear cases, bone marrow examination may be necessary. Platelet indices like mean platelet volume (MPV) can provide additional diagnostic information.
Q4. When should platelet transfusions be considered in ICU patients? Platelet transfusions are recommended for active bleeding (WHO grade ≥2) or when counts fall below 10 × 10^9/L in stable patients. Higher thresholds may be used before invasive procedures or in patients at high risk of bleeding. For intracranial hemorrhage, maintaining counts above 100 × 10^9/L is advised.
Q5. How is heparin-induced thrombocytopenia (HIT) diagnosed and managed in the ICU? HIT diagnosis involves using the 4Ts score for initial assessment, followed by anti-PF4/heparin antibody testing and functional assays for confirmation. If HIT is suspected, all heparin products must be discontinued immediately, and alternative anticoagulation initiated. HIT is rare but potentially devastating, affecting about 0.4% of critically ill patients.
References:
[1] – https://annalsofintensivecare.springeropen.com/articles/10.1186/s13613-025-01447-x
[2] – https://mmrjournal.biomedcentral.com/articles/10.1186/s40779-020-00244-w
[3] – https://pubmed.ncbi.nlm.nih.gov/16104535/
[4] – https://pmc.ncbi.nlm.nih.gov/articles/PMC4273722/
[5] – https://www.nature.com/articles/s41598-021-86915-7
[6] – https://karger.com/jin/article/16/1/337/908229/Unraveling-the-Intricate-Web-Complement-Activation
[7] – https://www.atsjournals.org/doi/full/10.1164/ajrccm.162.2.ncc3-00
[8] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9877263/
[9] – https://ashpublications.org/blood/article/142/Supplement 1/1294/502225/Post-Transfusion-Purpura-A-Literature-Review
[10] – https://pmc.ncbi.nlm.nih.gov/articles/PMC6679237/
[11] – https://pubmed.ncbi.nlm.nih.gov/34735904/
[12] – https://www.wjgnet.com/1007-9327/full/v28/i30/4061.htm
[13] – https://ashpublications.org/blood/article/128/26/3032/116533/How-I-evaluate-and-treat-thrombocytopenia-in-the
[14] – https://thrombosisjournal.biomedcentral.com/articles/10.1186/s12959-024-00637-0
[15] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9546174/
[16] – https://ccforum.biomedcentral.com/articles/10.1186/s13054-022-03928-y
[17] – https://www.webmd.com/a-to-z-guides/thrombocytopenia-symptoms-causes-treatments
[18] – https://pmc.ncbi.nlm.nih.gov/articles/PMC6142536/
[19] – https://www.atsjournals.org/doi/10.1164/ajrccm.162.2.ncc3-00
[20] – https://pmc.ncbi.nlm.nih.gov/articles/PMC5164902/
[21] – https://emcrit.org/ibcc/thrombocytopenia/
[22] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9482743/
[23] – https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0208715
[24] – https://www.tandfonline.com/doi/full/10.1080/00365513.2025.2453903?src=
[25] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10486945/
[26] – https://pubmed.ncbi.nlm.nih.gov/25643015/
[27] – https://pmc.ncbi.nlm.nih.gov/articles/PMC7953673/
[28] – https://ccforum.biomedcentral.com/articles/10.1186/cc13115
[29] – https://pmc.ncbi.nlm.nih.gov/articles/PMC4937543/
[30] – https://www.frontiersin.org/journals/medicine/articles/
10.3389/fmed.2021.735796/full
[31] – https://febs.onlinelibrary.wiley.com/doi/10.1002/1873-3468.13881
[32] – https://pmc.ncbi.nlm.nih.gov/articles/PMC6408643/
[33] – https://www.sciencedirect.com/topics/medicine-and-dentistry/thrombocyte-transfusion
[34] – https://journal.chestnet.org/article/S0012-3692(25)00279-X/fulltext
[35] – https://www.cureus.com/articles/105137-a-comprehensive-review-of-thrombocytopenia-with-a-spotlight-on-intensive-care-patients
[36] – https://www.nejm.org/doi/full/10.1056/NEJMoa2214322
[37] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8486553/
[38] – https://www.rarediseaseadvisor.com/news/study-shows-improved-transfusion-outcomes-with-hla-matched-platelet-units/
[39] – https://pubmed.ncbi.nlm.nih.gov/33475737/
[40] – https://pubmed.ncbi.nlm.nih.gov/20149589/
[41] – https://pmc.ncbi.nlm.nih.gov/articles/PMC3219407/
[42] – https://arupconsult.com/content/heparin-induced-thrombocytopenia
[43] – https://www.ncbi.nlm.nih.gov/books/NBK430721/
[44] – https://ashpublications.org/hematology/article/2017/
1/651/21144/Thrombocytopenia-in-hospitalized-patients-approach
[45] – https://bestpractice.bmj.com/topics/en-us/1000
[46] – https://pubmed.ncbi.nlm.nih.gov/20502168/
[47] – https://pmc.ncbi.nlm.nih.gov/articles/PMC2935185/

