Gastrointestinal diseases (aka GI disease or GI disorder) are those that affect the digestive tract (GI tract). This may include sections from the esophagus to the rectum, and the accessory digestive organs liver, gallbladder, and pancreas. Gastrointestinal diseases can be acute, chronic, or recurrent. It covers a wide range of diseases, including IBS, lactose intolerance, dyspepsia, GERD, diverticular disease, etc.
A few words about the Gastrointestinal (GI) tract
The GI or digestive tract starts at the mouth and ends at the anus. In between are the esophagus, stomach, small intestine, and large intestine. The liver and pancreas produce bile and pancreatic juices aid digestion. Whereas the gallbladder stores bile until it is needed for digestion.
The GI tract is divided into two main sections: the upper and the lower GI tracts.
- Upper GI tract – includes mouth, pharynx, esophagus, and stomach. The stomach leads to small intestine.
- Lower GI tract includes small & large intestines and the anus. Important parts of small intestine are the duodenum, jejunum, and ileum. Cecum, colon, and rectum makes the large intestine.
A number of different conditions or diseases can affect the GI tract. Some conditions share same symptoms, and some may show serious complications that demands further medical investigations.
Common gastrointestinal diseases
Upper gastrointestinal diseases:
Achalasia
Heartburn and achalasia have some things in common, but they’re not the same. While both cause trouble swallowing, achalasia happens when nerve cells in the esophagus degenerate for unknown reasons. Achalasia is rare; approx. 1 in 100,000 people gets it. Although there’s no cure, treatment will help one live with it. The most evident symptom of this upper gastrointestinal disease is difficulty swallowing. Heartburn, chest pain, difficulty burping, weight loss are the other symptoms. Foods such as bread and red meat worsen the symptoms.
The barium swallow test is the most common diagnostic procedure. So is Esophageal manometry. Drug therapy, Balloon dilation, Myotomy (surgical removal of the muscle fibers of lower esophageal sphincter), and Botulinum toxin injection are suggested for long-term reliefs.
Dyspepsia
This fancy medical term is nothing but indigestion, something we all experience from time to time. Typical symptoms include pain or discomfort in the upper abdomen, bloating, nausea, belching and gas, and burping. People often have heartburn and an acidic taste in the stomach as well. But these could be an indication of another gastrointestinal disease.
Talking about the causes, sometimes it could be just an upset stomach. Excess alcohol consumption, caffeine, drugs such as aspirin, and anxiety or depression may also trigger dyspepsia. In some individuals, ingestion may arise due to ulcers, GERD, IBS, and chronic pancreatitis.
Treatment majorly depends on diagnosing and treating the underlying condition causing it. The best ways to prevent indigestion are,
- Saying ‘no’ to overeating
- Avoiding acidic foods, caffeine-filled beverages, and alcohol
- Relaxation therapy (for stress-related indigestion)
- Avoiding workouts with a full stomach
- Sleeping with the head elevated (at least 6 inches) above the feet. This will prevent digestive juices from refluxing back.
Gastroparesis
Gastroparesis means “stomach paralysis”. It is an upper GI disorder characterized by abnormal or lack of gastric motility. In healthy individuals, gastric contractions help to break down ingested food and then propel it into the small intestine for digestion and absorption. On the other hand, in individuals suffering gastroparesis, due to poor contraction, normal digestion may not occur. This, in turn, causes nausea and vomiting. In certain individuals, it can even cause problems with blood sugar levels.
The causes of gastroparesis can include:
- Uncontrolled diabetes
- Vagus nerve damage during gastric surgery
- Narcotics and antidepressants
- Parkinson’s disease or Multiple sclerosis
- Amyloidosis (protein fiber deposits in tissues and organs) and scleroderma (a connective tissue disorder)
It’s not completely curable but can manage and control the symptoms using,
- Medications (erythromycin, antiemetics, Reglan, etc)
- Dietary modifications
- Surgical treatment
Gastroesophageal Reflux Disease (GERD)
In normal digestion, the food travels down the esophagus and into the stomach where the lower esophageal sphincter (LES) acts as a gateway for the food. But sometimes the LES acts weird and doesn’t close properly, allowing stomach acid to reflux back into the esophagus. That’s acid reflux. It may also cause a burning sensation in the chest called heartburn. Acid reflux or heartburn often occurs after meals or at night.
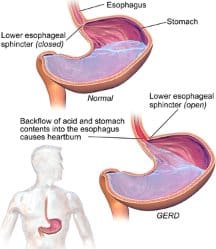
Frequent, strong acid reflux is one of the signs of gastroesophageal reflux disease (GERD), a gastrointestinal disease that affects about 20 percent of the U.S. population. Symptoms include:
- A burning sensation behind the chest, that radiates into the throat
- Acidic or sour taste in the mouth
- Chronic sore throat, cough and frequent hiccups
- Regurgitations
- Asthma
- Bad breath
- Loss of tooth enamel
If left untreated, GERD may cause complications including esophageal lesions, ulcers, and cancer of the esophagus or larynx.
GERD treatment depends on the severity of the symptoms. For some, GERD becomes manageable with simple lifestyle changes. Others may need proton pump inhibitors (PPI) such as lansoprazole, omeprazole, or esomeprazole to lower stomach acid production.
Lower gastrointestinal diseases
Constipation
Constipation means infrequent bowel movements (three or fewer) a week. It is another common GI disorder, afflicting about 40 million people in the United States. So, what causes constipation? Besides the obvious culprits – low fiber diet and inactive lifestyle – aging, medications (painkillers) or medical conditions (inflammatory bowel disease) may make one constipated.
Fortunately, in many cases, because constipation is due to a low fiber diet, eating fiber-rich foods often reverses the condition. Drinking enough water and regular exercises may also be helpful. It can then move on to Stimulants, Osmotics, Stool softeners, Enemas or suppositories if needed.
Biofeedback and bowel retraining are the popular alternative remedies suggested for constipation. Yes, these aren’t research-backed, but they can be used along with other treatment methods. Ultimately, treatment for constipation largely depends on the underlying cause.
Inflammatory bowel disease (IBD)
IBD is the inflammation or destruction of the intestine. It is a term used for a broad spectrum of GI diseases, but Crohn’s disease and ulcerative colitis are the most common. The exact cause of IBD is unknown. However, for many, genetics seems to play a vital role. IBD also arises from immune reactions (including autoimmune reactions) in the digestive tract.
- Crohn’s disease (CD): It can affect any part of the GI tract from the mouth to the anus; the small intestine and the colon are more susceptible. The possible complications of CD include ulcers, fistula, bowel obstructions, patchy tissue inflammation, internal bleeding, and tears in the anal skin.
- Ulcerative colitis (UC): It affects only the colon or large intestine. Unlike CD, UC causes continuous tissue inflammation which usually starts from the anus and moves up the intestine. The most common symptom of UC is bloody diarrhea. In some cases, ulcerative colitis may lead to an acute condition called toxic megacolon wherein colon paralyzes. This can cause cramping abdominal pain, tiredness, weight loss, and fever. It is serious and can be fatal if left untreated.
At present, there’s no cure for IBD. Medication to suppress IBD symptoms and lifestyle changes may help as well. In severe cases, IBD treatment may involve colectomy – surgical removal of the colon.
Irritable Bowel Syndrome (IBS)
IBS is the most common functional GI disease worldwide. Some studies estimate that 60 million people struggle with it, and it’s more common in people under age 45. These people are plagued by symptoms like cramping, abdominal pain, bloating, gas, diarrhea, and/or constipation.
The cause is unknown. Doctors believe that a mix of factors such as lifestyle, a bacterial infection in the GI tract, and depression/anxiety can trigger IBS symptoms. Because about two-thirds of the sufferers are women, some believe reproductive hormones play a role. Some studies also suggest a brain-gut connection in IBS; altered serotonin (the important neurotransmitter involved in peristaltic movement) levels are believed to change bowel functions.
IBS is of four types. The most common ones are IBS with constipation (IBS-C) and IBS with diarrhea (IBS-D). When there’s both constipation and diarrhea, it is called mixed IBS (IBS-M). People with unsubtyped IBS (IBS-U) don’t fit into these categories.
Speaking of the diagnosis, there aren’t any specific IBS tests. However, doctors look for a pattern in the symptoms. Also, blood tests, a stool test, a colonoscopy, or X-rays of the lower GI tract are suggested to rule out food allergy, GI tract infection or IBD.
IBS treatment is different for everyone. The right treatment plan involves lifestyle changes, antispasmodic drugs, anti diarrhoea medication, Bulk-forming laxatives, or Tricyclic antidepressants (TCAs).
Additional information can be found
here.
Hemorrhoids: a common gastrointestinal disease
Hemorrhoids, aka piles, are another common lower gastrointestinal disease. It affects nearly half of the American population age 50 and above. It develops when the veins in the anus or rectum swell in response to overweight, constipation, heavy lifting, or pregnancy.
Hemorrhoids can develop inside the lower rectum (internal hemorrhoids) or under the skin around the anus (external hemorrhoids). Nearly three out of four adults will develop symptoms, which include rectal pain, itching, bleeding, swelling or inflammation. Diagnosing piles might include a visual or digital examination. At times colonoscopy is also suggested to evaluate the risk of colorectal cancer.
Relieving mild pain and discomfort involves topical medications, dietary changes, oral pain killers, and sitz bath. Thrombectomy is the only effective treatment in case of external hemorrhoids involving blood clots.
Celiac Disease
An estimated 1 in 100 individuals worldwide have celiac disease, according to the recent reports. In simple terms, Celiac disease is gluten sensitivity. Gluten is a protein found in wheat, barley, and rye. When consumed, gluten triggers an autoimmune reaction in the small intestine. This damages villi, the finger-like protrusions in the small intestines that help in nutrient absorption.
The most common signs and symptoms of this GI disease include,
- Diarrhea
- Fatigue
- Weight loss
- Bloating and gas
- Iron deficiency anemia
- Abdominal pain
- Headaches, Nausea, and vomiting
- Constipation
Celiac disease runs in families. Individuals with a first-degree relative suffering from celiac disease (parents, children, or siblings) have a 1 in 10 risks of developing celiac disease. Celiac disease is more prevalent in people who have,
- Type 1 diabetes
- Down syndrome or Turner syndrome
- Autoimmune thyroid disease
- Addison’s disease
There’s no cure for celiac disease. But it’s important to treat celiac disease because it can lead to anemia, osteoporosis or lymphoma in adults and slow growth in children. Following a strict gluten-free diet can help reduce symptoms of celiac disease.
There’s another good news for one’s suffering gluten-intolerance. The clinical trials by the Northwestern Medicine show that immune tolerance to gluten can be induced.
Colon polyps and cancer
Colorectal cancer is the third leading cause of cancer deaths in the United States, says the American Cancer Society. In most cases, it starts as polyps – growths on the inner lining of the colon or rectum. In general, the polyps aren’t harmful and, not all polyps become cancer. But some can turn into colorectal cancer over time. The chances of developing cancer depend on the type of polyps.
- Hyperplastic polyps: These aren’t precancerous and can be removed surgically.
- Adenomas: These are the precancerous polyps. About two-thirds of colon polyps are, in fact, adenomas. However, the percentage of adenomas turning into colorectal cancer is unpredictable.
- Sessile serrated polyps: These polyps increase the risk factor tenfold.
Fortunately, with advances in early detection and treatment, this gastrointestinal disease can be prevented. Colonoscopy revealing polyps larger than 2 cm, multiple polyps and dysplasia after polyp removal, etc need follow-up visits.
GI diseases: Prevention
Many lower gastrointestinal disorders are preventable with proper diet, good bowel habits, and submitting to regular screening tests. Aging may spur the signs and symptoms, but they are manageable with medications and regular exercises. In general, one should consult doctor if she/he has,
GI Diseases: Symptoms Needing Emergency Care
Whether or not the GI symptoms are anxiety-, diet- or age-related, diagnosis
is mandatory. Detailed evaluation is required when there is:
- Sudden weight loss
- Persistent fever
- Feeling bloated for longer
- Blood in the stool
- Change in bowel habits
- Unusual abdominal cramps and pains
Immediate medical care is warranted if the symptoms include:
- Severe abdominal pain
- Chronic diarrhea
- Chest, neck, shoulder or jaw pain
- Rectal bleeding
Gastroenterology and related calculators
Gastrointestinal Diseases- an overview
Calculators / Tools
ABIC score – Stratification of risk of death in alcoholic hepatitis (AH)
Alcoholic Hepatitis Histological Score (AHHS)– Prognostic Stratification of Alcoholic Hepatitis
Child-Turcotte-Pugh Score -chronic liver disease – used to assess the prognosis of chronic liver disease, mainly cirrhosis. Although it was originally used to predict mortality during surgery, it is now used to determine the prognosis, as well as the required strength of treatment and the necessity of liver transplantation.
Crohn’s Disease Activity Index (CDAI)– The CDAI is an important research tool for quantifying symptoms as well as determining the impact of drug therapy on overall symptoms.
Forrest classification – Risk stratification of upper gastrointestinal hemorrhage -UGIB
Glasgow alcoholic hepatitis score (GAHS) predicts survival from alcoholic hepatitis with respect to individual Glasgow alcoholic hepatitis score (GAHS) values
Glasgow-Blatchford bleeding score (GBS)– Screening tool for acute upper gastrointestinal bleeding (UGIB)
Harvey-Bradshaw Index – useful tool for assessing the degree of illness (activity) in patient’s with Crohn’s disease
Irritable Bowel Syndrome (IBS) treatment options
Lille Model Scoring in Severe Alcoholic Hepatitis – helps to identify patients ‘early’ with severe alcoholic hepatitis that are likely to respond to steroid therapy or who will require alternative treatment options.
Mayo Scoring System for Assessment of Ulcerative Colitis
MELD Score (Model For End-Stage Liver Disease) – useful tool in predicting the probability of death from liver disease and how urgently an individual needs a liver transplant in the next three months.
MELD-Na Score (Model For End-Stage Liver Disease) -United Network for Organ Sharing proposed that MELD-Na score (an extension of MELD) may better rank candidates based on their risk of pre-transplant mortality and is projected to save 50-60 lives total per year.
Modified Maddrey’s discriminant function (mDF) – (Score) is a predictive statistical model useful for evaluating the severity and prognosis in alcoholic hepatitis
Ransons Criteria mortality risk for acute pancreatitis- clinical prediction rule for predicting the prognosis and mortality risk of acute pancreatitis.
Rockall score for the evaluation of upper gastrointestinal bleeding – based on clinical criteria including age, shock and presence of other comorbidities. The scoring system helps evaluate patients at risk of re-bleeding or death following acute upper gastrointestinal bleeding
Rome iii criteria for IBS
Rome IV diagnostic criteria -Irritable Bowel Syndrome
Stool Osmotic Gap– Secretory vs Osmotic diarrhea

