GLP-1 Agonists for NASH Treatment: New Clinical Evidence Reveals Surprising Results

Introduction
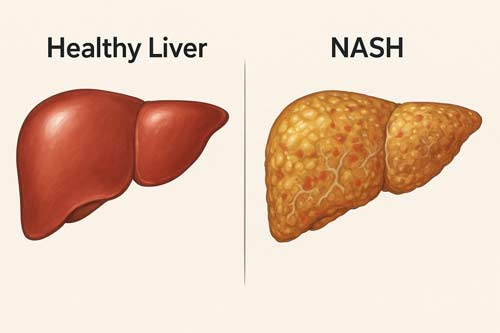
Non-alcoholic fatty liver disease (NAFLD) has emerged as a major global health concern, affecting approximately one in four individuals worldwide. It is now recognized as the most common cause of chronic liver disease, with an estimated prevalence of 32.4% in the general population. A notable proportion of patients with NAFLD progress to non-alcoholic steatohepatitis (NASH), a more severe form characterized by hepatic inflammation and varying degrees of fibrosis. Current data indicate that up to 15% of individuals with NAFLD develop NASH. The burden is particularly striking among high-risk populations: up to 70% of patients with type 2 diabetes mellitus (T2DM) are affected by NAFLD, and one in five adults with obesity and diabetes has NASH with clinically relevant fibrosis.
Despite this high prevalence and the progressive nature of the disease, therapeutic options remain limited. At present, substantial and sustained weight loss of at least 7 to 10% of body weight is the only intervention consistently shown to improve histological features of NAFLD and NASH. However, achieving and maintaining this degree of weight reduction through lifestyle modification alone is challenging for most patients, creating an urgent need for effective pharmacological therapies.
Glucagon-like peptide-1 (GLP-1) receptor agonists have recently emerged as promising therapeutic agents in this context. Initially developed for the management of T2DM, GLP-1 receptor agonists exert multiple metabolic effects, including improved insulin sensitivity, appetite suppression, and weight reduction. Beyond these systemic benefits, evidence now suggests that GLP-1 receptor activation has direct effects on hepatocytes, contributing to reductions in steatosis, inflammation, and fibrosis.
Clinical trials have provided compelling evidence supporting their potential role in NASH treatment. In a landmark phase II study, semaglutide demonstrated NASH resolution without worsening of fibrosis in 36 to 59% of patients with liver fibrosis, compared with only 17% in the placebo group. Similarly, the LEAN trial showed that liraglutide was associated with remarkably higher rates of NASH resolution and a reduction in fibrosis progression relative to placebo. These results represent a major advance, as no pharmacological therapy has previously demonstrated such consistent improvements in histological endpoints for NASH.
Taken together, the growing body of evidence positions GLP-1 receptor agonists as a potential breakthrough in the management of NASH. By targeting both the underlying metabolic drivers of the disease and the hepatic pathology directly, these agents may help address one of the most critical gaps in hepatology today—the lack of effective, widely applicable treatments for patients with progressive fatty liver disease.
GLP-1 Receptor Agonists: Mechanism and Relevance to NASH
Glucagon-like peptide-1 (GLP-1) is a 30-amino acid peptide hormone secreted primarily by enteroendocrine L-cells in the distal small intestine and colon. It plays a central role in regulating postprandial glucose homeostasis by enhancing glucose-dependent insulin secretion, suppressing glucagon release, slowing gastric emptying, and modulating food intake and gut motility. Beyond its role in glucose regulation, GLP-1 has gained recognition as a therapeutic target in metabolic disorders. GLP-1 receptor agonists (GLP-1 RAs), already established in the management of type 2 diabetes mellitus and obesity, have emerged as promising candidates for the treatment of nonalcoholic steatohepatitis (NASH), owing to their broad metabolic and hepatoprotective effects.
GLP-1 receptor distribution in hepatocytes and metabolic tissues
The GLP-1 receptor (GLP-1R) exhibits wide tissue distribution. High expression levels are found in the distal ileum and colon, pancreatic alpha and beta cells, and several regions of the central nervous system (CNS). Lower levels of expression have also been identified in the heart, lungs, kidneys, vasculature, and peripheral nervous system.
The presence of GLP-1R in hepatocytes, however, remains a subject of debate. Some studies have reported GLP-1R expression in both transformed hepatocyte cell lines (HuH7 and Hep-G2) and in primary human hepatocytes. Immunohistochemical analyses of liver samples from patients with NASH demonstrated GLP-1R localization to the basolateral membranes of hepatocytes with macrovesicular steatosis, as well as in mononuclear cells infiltrating hepatic sinusoids. Other reports, in contrast, have suggested that hepatocytes lack functional GLP-1R, implying that the hepatic benefits of GLP-1 RAs may be mediated indirectly, for example through systemic metabolic improvements or modulation of the gut-liver axis.
This broad tissue distribution explains why GLP-1 RAs exert effects on multiple organ systems simultaneously, a property that makes them particularly suited to address the complex pathophysiology of NASH, which involves dysregulation of glucose and lipid metabolism, insulin resistance, inflammation, and fibrosis.
Effects on insulin resistance and lipotoxicity
GLP-1 RAs target several fundamental mechanisms in NASH pathogenesis. By stimulating glucose-dependent insulin secretion from pancreatic beta cells and inhibiting glucagon release from alpha cells, they improve glycemic control while avoiding hypoglycemia. Their ability to slow gastric emptying and reduce postprandial glucose excursions further contributes to metabolic stability.
A central therapeutic action of GLP-1 RAs in NASH is the improvement of insulin sensitivity in both hepatic and adipose tissues. Clinical studies with liraglutide, for example, demonstrated enhanced hepatic insulin sensitivity, with suppression of endogenous glucose production by 9.36% under low-dose insulin infusion compared with 2.54% in placebo-treated controls. Similarly, improvements in adipose tissue insulin sensitivity enhance the ability of insulin to suppress lipolysis, thereby reducing the flux of free fatty acids to the liver.
Lipotoxicity, another critical driver of NASH, is also attenuated by GLP-1 RAs. These agents reduce hepatic de novo lipogenesis in vivo, with a reported 1.26% decrease compared to a 1.30% increase observed with placebo. In primary human hepatocytes, GLP-1 RAs reduced lipogenesis by approximately 24.6% compared to untreated controls. Furthermore, liraglutide has been shown to limit the hepatic accumulation of ceramide and sphingomyelin species, lipotoxic metabolites implicated in cellular stress and inflammation.
The anti-inflammatory and antifibrotic effects of GLP-1 RAs further reinforce their therapeutic potential in NASH. In preclinical models, such as methionine-choline deficient dietary models, liraglutide reduced hepatic inflammation by decreasing the infiltration of M1 pro-inflammatory macrophages and attenuated early fibrotic changes, effects that occurred independently of weight loss.
Comparison with SGLT2 inhibitors in metabolic regulation
Both GLP-1 RAs and sodium-glucose cotransporter-2 inhibitors (SGLT2is) have demonstrated clinically meaningful improvements in metabolic parameters and liver health in patients with NASH. Both classes reduce hepatic steatosis and normalize serum transaminases, although subtle differences in efficacy have been noted.
Network meta-analyses suggest that SGLT2is may exert greater effects on reducing alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels. GLP-1 RAs, however, demonstrate superior efficacy in histological resolution of NASH, with a reported relative risk of 2.48 (95% CI: 1.86–3.30) compared to placebo.
The mechanisms underlying these effects also diverge. SGLT2is improve hepatic metabolism primarily through modulation of glucagon signaling pathways and systemic improvements in insulin resistance, while also promoting glucosuria and caloric loss. In contrast, GLP-1 RAs exert their effects through weight reduction, enhancement of insulin sensitivity, modulation of lipogenesis, and regulation of the gut-liver axis.
Despite these mechanistic differences, both drug classes consistently outperform many other therapeutic options in reducing anthropometric parameters such as body weight and body mass index. Importantly, emerging evidence suggests that combination therapy with GLP-1 RAs and SGLT2is may provide synergistic benefits, producing greater reductions in body weight, glycated hemoglobin (HbA1c), and potentially liver-related endpoints compared with either therapy alone.
Semaglutide and Liraglutide: Clinical Trial Highlights
Recent clinical trials exploring GLP-1 receptor agonists for NASH treatment have yielded promising results, establishing these agents as potential therapeutic options for this previously difficult-to-treat condition.
LEAN Trial: Liraglutide and NASH resolution
The pioneering LEAN (Liraglutide Safety and Efficacy in patients with Non-alcoholic steatohepatitis) trial marked the first rigorous evaluation of GLP-1 agonists for NASH treatment. This multicentre, double-blind, randomized, placebo-controlled phase 2 study assessed subcutaneous liraglutide (1.8 mg daily) against placebo over 48 weeks. The trial primarily recruited overweight patients with biopsy-confirmed NASH across four UK medical centers.
Results from the LEAN trial demonstrated that 39% of patients receiving liraglutide achieved histological resolution of NASH compared with merely 9% in the placebo group. This represented a relative risk of 4.3 (95% CI: 1.0-17.7; p=0.019) for achieving NASH resolution. Notably, patients treated with liraglutide showed substantially less fibrosis progression—only 9% versus 36% in the placebo group (p=0.04).
Apart from histological improvements, 48-week liraglutide treatment produced meaningful reductions in body weight compared to placebo. The trial exhibited a favorable safety profile with mostly mild to moderate gastrointestinal adverse events, including diarrhea (38% versus 19% in placebo), constipation (27% versus none), and appetite loss (31% versus 8%).
Semaglutide Phase 2 Trial: 59% NASH resolution at 0.4 mg/day
Building upon the foundation established by the LEAN trial, researchers subsequently conducted a larger phase 2 trial evaluating semaglutide’s efficacy in NASH patients. This 72-week multicenter, randomized, double-blind, placebo-controlled study included 320 middle-aged obese patients with biopsy-proven NASH (mean age: 55 years; mean BMI: 35 kg/m²; 61% women; 62% with type 2 diabetes). Participants received once-daily subcutaneous semaglutide at doses of 0.1 mg (80 patients), 0.2 mg (78 patients), 0.4 mg (82 patients), or placebo (80 patients).
The trial’s primary endpoint—NASH resolution without worsening fibrosis—was achieved in strikingly higher proportions of semaglutide-treated patients across all dosage groups. Specifically, 40% in the 0.1-mg group, 36% in the 0.2-mg group, and 59% in the 0.4-mg group achieved this endpoint, compared to just 17% receiving placebo. The 0.4-mg group demonstrated the most impressive results (p<0.001 versus placebo).
Nonetheless, regarding the secondary endpoint of fibrosis improvement without NASH worsening, the differences between treatment groups did not reach statistical significance (49%, 32%, and 43% in the respective semaglutide groups versus 33% in placebo). The percentage of patients achieving both NASH resolution and fibrosis improvement was 37% in the 0.4-mg semaglutide group versus 15% in the placebo group.
Dose-dependent effects on liver enzymes and fibrosis progression
Both liraglutide and semaglutide demonstrated dose-dependent improvements in liver biochemistry and metabolic parameters. For liraglutide specifically, a meta-analysis of 4,442 patients with type 2 diabetes revealed that the 1.8 mg/day dosage (but not lower doses of 0.6 or 1.2 mg/day) produced meaningful reductions in ALT levels in patients with elevated baseline values.
Throughout the semaglutide trial, researchers observed dose-dependent decreases in liver enzyme levels. The maximum reduction in ALT occurred approximately 28-30 weeks after treatment initiation, followed by stabilization. At the 48-week mark, changes in ALT from baseline were substantially greater with semaglutide than placebo (ETR 0.76; 95% CI: 0.61-0.93; p=0.0090). Essentially, 40% of semaglutide-treated patients achieved a clinically meaningful ALT reduction of at least 17 units compared to only 8% in the placebo group (p=0.0057).
Alongside enzyme improvements, semaglutide produced dose-dependent weight reduction. Mean percent changes in body weight were -5% in the 0.1-mg group, -9% in the 0.2-mg group, -13% in the 0.4-mg group, and merely -1% in the placebo group. Accordingly, researchers observed parallel improvements in glycemic control, with the most pronounced HbA1c reduction (-1.15%) occurring in the 0.4-mg group.
Regarding adverse events, gastrointestinal disorders (nausea, constipation, decreased appetite, vomiting, abdominal pain) occurred most frequently, with 68% of patients in the 0.4-mg semaglutide group experiencing such symptoms. These effects primarily manifested during the first 20 weeks of treatment during dose escalation. Discontinuation rates due to adverse events were comparable between semaglutide (7% across all doses) and placebo (5%).
Histological Outcomes: Steatosis, Inflammation, and Fibrosis
Histopathological examination remains the gold standard for assessing treatment efficacy in non-alcoholic steatohepatitis (NASH). GLP-1 receptor agonists have demonstrated robust effects on multiple aspects of liver histology, offering promising therapeutic potential for patients with this challenging condition.
Reduction in intrahepatic triglyceride content
Preclinical studies initially established that GLP-1 receptor agonists could effectively reduce hepatic triglyceride accumulation. Exendin-4, a GLP-1R agonist derived from Gila monster saliva, substantially reduced hepatic triglyceride content in both mouse models and human hepatocytes by activating insulin receptor downstream signaling. When compared with other antidiabetic medications, exenatide demonstrated superior efficacy in reducing hepatic triglyceride content.
Clinical trials have since confirmed these findings. Liraglutide consistently produced reductions in liver fat content ranging from 19% to 32% across multiple studies. Magnetic resonance imaging-derived proton density fat fraction (MRI-PDFF) assessments revealed that semaglutide treatment resulted in greater improvements in liver steatosis compared to placebo after 48 weeks (ETR 0.67; 95% CI: 0.51–0.88; p=0.0042). Indeed, 49% of semaglutide-treated patients achieved at least a 30% reduction in steatosis versus merely 13% in the placebo group (odds ratio 6.58; 95% CI: 1.63–39.31; p=0.0037).
ALT and AST normalization timelines
Liver enzyme normalization represents an essential marker of treatment response in NASH. Following initiation of GLP-1 receptor agonist therapy, improvements in alanine aminotransferase (ALT) and aspartate aminotransferase (AST) typically follow a predictable timeline.
Maximum reduction in ALT levels generally occurs approximately 28-30 weeks after treatment initiation, followed by stabilization. At week 48, changes in ALT from baseline were markedly greater with semaglutide than placebo (ETR 0.76; 95% CI: 0.61–0.93; p=0.0090). More importantly, 40% of semaglutide-treated patients achieved a clinically meaningful ALT reduction of at least 17 units compared to only 8% in the placebo group (p=0.0057).
Similar improvements were observed with AST, where semaglutide demonstrated superior reductions compared to placebo (ETR 0.77; 95% CI: 0.65–0.92; p=0.0046). Case series have documented normalization of liver enzymes within 3-8 months of initiating treatment, with sustained improvement over subsequent years.
Fibrosis stage improvement vs placebo
The impact of GLP-1 receptor agonists on fibrosis has yielded somewhat mixed results. In the LEAN trial, liraglutide treatment resulted in substantially less fibrosis progression—only 9% versus 36% in the placebo group (p=0.04). This suggests that liraglutide may exert a protective effect against fibrosis advancement.
Conversely, in the landmark semaglutide trial, the percentage of patients with improvement in fibrosis stage without worsening of NASH did not reach statistical significance between treatment groups—49%, 32%, and 43% in the respective semaglutide groups versus 33% in placebo. The reasons behind this unexpected lack of fibrosis improvement remain unclear, especially considering that weight loss ≥10% during lifestyle intervention studies typically leads to fibrosis improvement.
Overall, the proportion of patients who achieved both NASH resolution and fibrosis improvement was 37% in the high-dose semaglutide group versus 15% in the placebo group.
NAFLD Activity Score (NAS) changes
The NAFLD Activity Score (NAS) provides a comprehensive measure of disease activity in NASH. Treatment with GLP-1 receptor agonists has consistently demonstrated improvements in this composite score.
In the semaglutide phase 2 trial, improvements in NAS were observed in 71% of patients in the 0.1-mg group, 80% in the 0.2-mg group, and 83% in the 0.4-mg group, compared with only 44% in the placebo group. These improvements reflected beneficial effects across all NAS components—steatosis, inflammation, and hepatocyte ballooning.
When examining individual NAS components, semaglutide treatment resulted in improvements in steatosis grade (45% vs 33% with placebo), lobular inflammation (43% vs 38%), and hepatocyte ballooning (55% vs 33%). Furthermore, NAS improvement was achieved by 62% of patients receiving semaglutide versus 58% in the placebo group.
Combining GLP-1 receptor agonists with other metabolic agents may enhance histological outcomes further. The addition of exenatide to pioglitazone was associated with greater reductions in hepatic fat content compared to pioglitazone monotherapy, suggesting potential benefits from combination approaches.
Weight Loss and Glycemic Control as Indirect Drivers
The therapeutic effects of GLP-1 receptor agonists on NASH appear to operate through two primary indirect mechanisms: weight reduction and improved glycemic control. These metabolic changes subsequently drive histological improvements, making them crucial to understanding the full therapeutic potential of these agents.
Semaglutide-induced 12.5% body weight reduction
Weight loss represents a cornerstone in GLP-1 agonist therapy for NASH patients. In pivotal clinical trials, semaglutide demonstrated significant dose-dependent effects on body weight. The mean percent changes in body weight were −5% in the semaglutide 0.1-mg group, −9% in the 0.2-mg group, −13% in the 0.4-mg group, versus merely −1% in the placebo group. This weight reduction typically continued until approximately weeks 28 to 44 and remained stable thereafter.
At higher doses used for obesity treatment, semaglutide (2.4 mg weekly) induced even more substantial weight loss, ranging between 9.6% and 17.4%. In contrast, liraglutide at 3 mg daily dosage reduced body weight by approximately 8.4 kg after one year of treatment.
Across various trials, about two-thirds of patients receiving GLP-1 agonists achieved at least 5% weight loss, whereas one-third accomplished more than 10% reduction. This pattern of weight loss appears consistent across different GLP-1 receptor agonists, though the magnitude varies based on specific agent and dosage.
HbA1c reduction in T2DM patients with NASH
Beyond weight loss, GLP-1 agonists exert profound effects on glycemic control. Dose-dependent reductions in glycated hemoglobin levels were observed in semaglutide-treated patients regardless of diabetes status. In the 0.4 mg semaglutide group, HbA1c decreased by approximately 1.15%.
Higher doses yield even greater improvements—in a 68-week trial involving patients with type 2 diabetes and obesity, once-weekly subcutaneous semaglutide 2.4 mg reduced HbA1c levels by 1.6% compared with merely 0.4% reduction with placebo. Liraglutide demonstrated similar efficacy, reducing mean HbA1c levels from 8.9% to 5.9% alongside improvements in intrahepatic fat content and transaminase levels.
Intriguingly, patients whose HbA1c decreased by ≥2.5% showed more substantial reductions in intrahepatic fat than those with smaller HbA1c improvements. Moreover, patients achieving HbA1c levels below 6.5% exhibited markedly lower intrahepatic fat content than those with higher values.
Correlation between weight loss and histological improvement
The relationship between weight reduction and histological improvement follows a dose-response pattern:
- Weight loss ≥3% can improve steatosis alone
- Weight loss ≥5% improves inflammation and stabilizes fibrosis
- Weight loss ≥7-10% resolves steatohepatitis in 65-90% of patients
- Weight loss ≥10% leads to fibrosis regression in approximately 45% of patients
This tiered response explains why varying degrees of histological improvement occur among GLP-1 agonist recipients. A systematic review examining lifestyle interventions revealed strong associations between reduction in intrahepatic fat, liver aminotransferase levels, and weight loss.
The correlation between weight loss magnitude and NASH resolution likely explains much of the histological benefit observed with GLP-1 receptor agonists. Besides, improvements in insulin resistance—as evidenced by enhanced HOMA-IR scores in GLP-1 agonist recipients—further contribute to these benefits.
Therefore, while direct hepatic effects of GLP-1 agonists remain important, their ability to induce substantial, sustained weight loss alongside improved glycemic control constitutes a critical mechanism underlying their efficacy in NASH treatment.
Safety Profile and Tolerability in NASH Patients
Alongside proven efficacy in NASH treatment, clinicians must carefully consider the safety profile of GLP-1 receptor agonists. Understanding the spectrum of adverse events enables appropriate patient selection and management strategies.
Gastrointestinal side effects: nausea, vomiting, diarrhea
GLP-1 receptor agonists commonly cause gastrointestinal disturbances, with an overall incidence rate of 58.9%. In clinical trials, nausea affected 32.54% of patients, making it the most prevalent complaint, followed by diarrhea (19.99%) and vomiting (16.18%). The semaglutide 0.4-mg dose produced markedly higher rates of nausea (42% vs 11%), constipation (22% vs 12%), and vomiting (15% vs 2%) compared to placebo. These effects typically emerge during the first 20 weeks of therapy, coinciding with dose escalation periods. Fortunately, most symptoms are transient and mild-to-moderate in severity, resolving within a few weeks without requiring intervention.
Gallbladder-related events and rapid weight loss
Gallbladder disorders represent a concerning adverse effect of GLP-1 therapy. Clinical trials documented higher rates of gallbladder-related issues with semaglutide (5-7%) versus placebo (2%). This risk appears dose-dependent, with higher doses carrying greater risk (RR 1.56) compared to lower doses (RR 0.99). Extended treatment duration (>26 weeks) likewise increases gallbladder disease probability.
The underlying mechanisms involve both direct and indirect effects. GLP-1 inherently inhibits gallbladder motility by suppressing cholecystokinin secretion. Yet rapid weight loss—a characteristic effect of these agents—independently contributes to gallstone formation. Hence, trials investigating GLP-1 agonists for weight management report higher gallbladder complication rates than diabetes-focused studies.
Discontinuation rates and dose escalation strategies
Treatment discontinuation occurred in 7% of semaglutide recipients versus 5% with placebo. Gastrointestinal complaints constituted the primary reason for withdrawal (4%). In real-world settings, persistence with GLP-1 therapy ranges between 40-60% at six months and 34-67% at one year.
To improve tolerability, gradual dose escalation proves beneficial. Weekly administration formats demonstrate better adherence than daily regimens. For patients experiencing intense or persistent gastrointestinal effects, temporarily maintaining the current dose or extending the escalation phase by 2-4 weeks often proves effective.
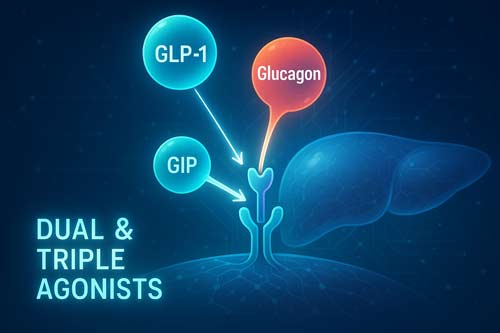
Future Directions: Dual and Triple Agonists in NASH
The evolution of incretin-based therapies for NASH now extends beyond single GLP-1 receptor agonists to multi-target approaches with enhanced metabolic effects.
GLP-1/GIP dual agonist tirzepatide in SYNERGY-NASH trial
The SYNERGY-NASH phase 2 trial evaluated tirzepatide, a dual GIP/GLP-1 receptor agonist, in patients with MASH and F2/F3 fibrosis. Results demonstrated dose-dependent MASH resolution without worsening fibrosis in 51.8%, 62.8%, and 73.3% of participants taking 5mg, 10mg, and 15mg doses respectively, versus merely 13.2% with placebo. Concurrently, fibrosis improvement occurred in 59.1%, 53.3%, and 54.2% of patients across the three dose groups compared to 32.8% with placebo.
GLP-1/glucagon co-agonists: cotadutide and pemvidutide
Cotadutide, a GLP-1/glucagon receptor dual agonist with 5:1 potency ratio, improved multiple hepatic parameters in phase 2 trials. After 54 weeks, patients experienced greater reductions in AST and ALT levels versus placebo. Likewise, pemvidutide showed noteworthy liver fat content reductions, with 94.4% of participants achieving ≥30% relative reduction at the 1.8mg dose. Approximately 55.6% of these patients normalized liver fat (≤5%) compared to none receiving placebo.
Retatrutide: 90% liver fat normalization in 48 weeks
Retatrutide, a novel triple GIP/GLP-1/glucagon receptor agonist, produced extraordinary results in patients with obesity and MASLD. At 48 weeks, relative liver fat reductions reached -81.7% and -86.0% with 8mg and 12mg doses respectively. Remarkably, 89% and 93% of participants achieved liver fat normalization (<5%) at these doses. This represents one of the largest treatment effects reported, with hepatic steatosis resolving in >85% of high-dose recipients.

Conclusion 
GLP-1 receptor agonists have emerged as groundbreaking therapeutic options for NASH patients, addressing a critical unmet need in hepatology. These agents demonstrate remarkable efficacy through both direct hepatic effects and indirect metabolic improvements. Specifically, semaglutide achieved NASH resolution in up to 59% of patients at the 0.4 mg dosage, while liraglutide showed resolution in 39% of treated individuals compared to merely 9% with placebo. The therapeutic benefits appear dose-dependent, with higher doses yielding more substantial improvements in histological parameters and liver enzymes.
Weight reduction serves as a primary driver of these benefits, as evidenced by the correlation between weight loss magnitude and histological improvement. Patients losing ≥7-10% of body weight typically experience NASH resolution, while those achieving ≥10% reduction often demonstrate fibrosis regression. Additionally, improved glycemic control further enhances these effects, particularly in patients with type 2 diabetes.
Though generally well-tolerated, GLP-1 receptor agonists commonly cause gastrointestinal disturbances during the initial treatment phase. Therefore, gradual dose escalation strategies prove beneficial for enhancing tolerability and treatment adherence. Clinicians should also remain vigilant about gallbladder-related complications, especially during periods of rapid weight loss.
The therapeutic landscape continues to evolve rapidly with the development of dual and triple agonists. Tirzepatide, a GLP-1/GIP dual agonist, demonstrated impressive NASH resolution rates of up to 73.3% in the SYNERGY-NASH trial. Even more promising, retatrutide—a novel triple GIP/GLP-1/glucagon receptor agonist—achieved liver fat normalization in approximately 90% of patients after 48 weeks of treatment, representing one of the most profound treatment effects documented thus far.
Based on mounting evidence, GLP-1 receptor agonists and their multi-target derivatives undoubtedly represent a paradigm shift in NASH management. Their ability to simultaneously address multiple pathophysiological mechanisms—including insulin resistance, hepatic lipotoxicity, and inflammation—distinguishes them from previous therapeutic approaches. As research advances and clinical experience grows, these agents will likely become cornerstone treatments for patients with this challenging metabolic liver disease.
Key Takeaways
Recent clinical trials have established glucagon-like peptide-1 receptor agonists (GLP-1 RAs) as a major breakthrough in the management of nonalcoholic steatohepatitis (NASH). For the first time, clinicians have pharmacological agents that demonstrate meaningful efficacy in a condition that was previously challenging to treat.
- Semaglutide demonstrates the strongest efficacy to date: In phase 2 trials, daily semaglutide at a 0.4 mg dose achieved NASH resolution in 59 percent of patients compared with 17 percent in the placebo group. This represents the highest success rate observed in clinical trials.
- Weight loss remains a central therapeutic driver: A reduction in body weight of at least 7 to 10 percent resolves NASH in approximately 65 to 90 percent of patients. A weight loss exceeding 10 percent has also been shown to improve liver fibrosis, underscoring the link between metabolic improvement and histological benefit.
- Adverse effects are primarily gastrointestinal: Nausea, vomiting, and diarrhea occur in about 59 percent of patients. These side effects are generally mild to moderate, transient, and improve within the first few weeks of therapy.
- Next-generation incretin-based therapies offer additional promise: Dual and triple agonists show enhanced efficacy compared with GLP-1 monotherapy. Retatrutide, a triple GIP/GLP-1/glucagon receptor agonist, normalized liver fat in 90 percent of patients after 48 weeks.
- Therapeutic response is dose- and time-dependent: The maximal improvements in aminotransferases and liver fat content typically occur around 28 to 30 weeks after initiating therapy, indicating that sustained treatment is necessary to achieve optimal benefit.
Collectively, these findings establish GLP-1 receptor agonists as transformative therapies for NASH. They act on multiple disease mechanisms simultaneously, including insulin resistance, hepatic steatosis, and chronic inflammation, thereby offering new hope to millions of patients living with progressive fatty liver disease.

Frequently Asked Questions:
FAQs
Q1. What are GLP-1 agonists and how do they work for NASH treatment? GLP-1 agonists are medications that mimic the effects of the hormone GLP-1. For NASH treatment, they work by reducing liver fat, improving insulin sensitivity, and promoting weight loss. They also have direct effects on liver cells to reduce inflammation and fat accumulation.
Q2. How effective are GLP-1 agonists in treating NASH? Clinical trials have shown impressive results. For example, semaglutide achieved NASH resolution in up to 59% of patients at the 0.4 mg dosage, compared to only 17% in the placebo group. Liraglutide showed resolution in 39% of treated individuals versus 9% with placebo.
Q3. What are the main side effects of GLP-1 agonists? The most common side effects are gastrointestinal, including nausea, vomiting, and diarrhea. These typically occur during the first few weeks of treatment and are usually mild to moderate. There’s also a small risk of gallbladder-related issues, especially with rapid weight loss.
Q4. How much weight loss can be expected with GLP-1 agonists? Weight loss varies but can be substantial. In clinical trials, semaglutide at 0.4 mg daily led to an average 13% reduction in body weight. Higher doses used for obesity treatment have shown even greater weight loss, up to 15-17% in some studies.
Q5. Are there new developments in GLP-1 agonist therapy for NASH? Yes, researchers are developing dual and triple agonists that target multiple receptors. For example, tirzepatide, a dual GLP-1/GIP agonist, has shown promising results in NASH trials. Retatrutide, a triple GIP/GLP-1/glucagon receptor agonist, has demonstrated even more impressive effects, normalizing liver fat in about 90% of patients after 48 weeks of treatment.
References:
[1] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8961394/
[2] – https://www.nejm.org/doi/full/10.1056/NEJMoa2028395
[3] – https://www.thelancet.com/journals/langas/article/PIIS2468-1253(23)00068-7/fulltext
[4] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8696030/
[5] – https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-020-00570-y
[6] – https://www.nature.com/articles/s41591-024-03018-2
[7] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9865319/
[8] – https://academic.oup.com/jcem/article/107/1/29/6354361
[9] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8063915/
[10] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8684453/
[11] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8350997/
[12] – https://pmc.ncbi.nlm.nih.gov/articles/PMC8351017/
[13] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9310586/
[14] – https://pmc.ncbi.nlm.nih.gov/articles/PMC10221116/
[15] – https://pmc.ncbi.nlm.nih.gov/articles/PMC11882565/
[16] – https://www.cghjournal.org/article/S1542-3565(24)00160-5/fulltext
[17] – https://pmc.ncbi.nlm.nih.gov/articles/PMC9821052/
[18] – https://investor.lilly.com/news-releases/news-release-details/lillys-tirzepatide-was-superior-placebo-mash-resolution-and-more
[19] – https://diabetesjournals.org/care/article/44/6/1433/138721/Effects-of-Cotadutide-on-Metabolic-and-Hepatic
[20] – https://www.journal-of-hepatology.eu/article/S0168-8278(24)02362-6/fulltext
[21] – https://www.adameetingnews.org/phase-2-trial-results-demonstrate-benefits-of-retatrutide-in-obesity-type-2-diabetes-nash/

