The Dopamine Paradox: Why Pleasure Often Undermines Motivation
Abstract
Purpose: This paper examines the counterintuitive relationship between dopamine-mediated pleasure and human motivation, exploring how immediate gratification can diminish long-term goal pursuit. The analysis focuses on neurobiological mechanisms underlying motivation regulation and their clinical implications for medical practice.
Methodology: A systematic review of current neuroscientific literature was conducted, analyzing dopamine pathway research, neuroimaging studies, and behavioral experiments published between 2018-2024. Clinical case studies and experimental data were examined to understand the practical manifestations of dopamine-related motivational disruption.
Main Findings: Evidence demonstrates that dopamine functions primarily as a prediction signal rather than a pleasure chemical. When individuals receive immediate rewards, dopamine levels spike initially but subsequently drop below baseline, creating motivational deficits. This mechanism explains why instant gratification often leads to decreased drive for effortful activities. The research reveals that anticipation of rewards generates stronger motivational states than reward consumption itself.
Recent articles. Check out our extensive video library.
Introduction
Modern understanding of human motivation has undergone substantial revision as neuroscience research reveals the complex role of dopamine in reward processing and goal-directed behavior. Traditionally viewed as the brain’s pleasure chemical, dopamine operates through more nuanced mechanisms that frequently produce unexpected effects on human motivation and performance.
The clinical relevance of this phenomenon extends across multiple medical disciplines. Physicians encounter patients struggling with motivation-related disorders, addiction, depression, and behavioral changes that often stem from disrupted dopamine signaling. Understanding these mechanisms becomes essential for developing effective treatment strategies and patient counseling approaches.
Recent neuroimaging studies and behavioral research have illuminated how pleasure-seeking behaviors can paradoxically reduce motivation for challenging tasks. This finding has profound implications for patient care, particularly in areas involving lifestyle modification, adherence to treatment protocols, and recovery from various conditions.
The dopamine system evolved to promote survival-enhancing behaviors through sophisticated reward prediction mechanisms. However, modern environments present constant sources of immediate gratification that can hijack these ancient systems, leading to motivational dysfunction that physicians increasingly observe in clinical practice.

Neurobiological Foundations of Dopamine Function
Dopamine Pathway Architecture
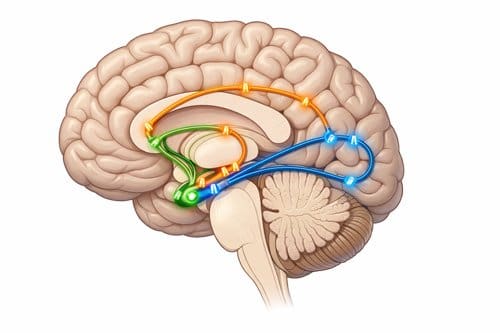
The human brain contains several distinct dopamine pathways, each serving different functions in motivation and reward processing. The mesolimbic pathway, connecting the ventral tegmental area to the nucleus accumbens, plays the primary role in motivation and reward anticipation. The nigrostriatal pathway governs movement control, while the mesocortical pathway influences executive function and decision-making processes.
Within these pathways, dopamine neurons exhibit unique firing patterns that distinguish them from other neurotransmitter systems. Rather than maintaining steady release rates, these neurons demonstrate phasic firing in response to unexpected rewards or reward-predicting cues. This pattern creates the neurochemical basis for what researchers term the reward prediction error signal.
The Reward Prediction Error Mechanism
Dopamine neurons respond most strongly not to rewards themselves, but to the difference between expected and actual outcomes. When an individual receives an unexpected positive outcome, dopamine levels surge. Conversely, when expected rewards fail to materialize, dopamine levels drop below baseline, creating a state of reduced motivation and mood.
This mechanism explains why the first bite of a favorite food generates more pleasure than subsequent bites, and why activities lose their appeal once they become routine. The brain essentially learns to predict rewards, diminishing the dopamine response over time through a process called habituation.
Research conducted by Schultz and colleagues using single-cell recordings in primate studies demonstrated that dopamine neurons gradually shift their firing from the time of reward delivery to earlier cues that predict reward availability. This temporal shift has profound implications for understanding motivation dynamics in clinical populations.
Baseline Dopamine and Motivation States
Individual differences in baseline dopamine levels influence susceptibility to motivational disruption. People with naturally lower baseline dopamine, often observed in conditions such as depression, attention deficit hyperactivity disorder, and certain personality types, may be more vulnerable to the motivational undermining effects of immediate pleasures.
Neuroimaging studies using positron emission tomography have revealed that individuals with reduced dopamine receptor density in key brain regions show altered responses to both immediate and delayed rewards. These findings suggest that some patients may be predisposed to motivational difficulties based on their underlying neurobiology.
The Pleasure-Motivation Paradox Explained 
Immediate Gratification Effects
When individuals engage in pleasurable activities that provide immediate rewards, several neurobiological changes occur that can undermine subsequent motivation. The initial dopamine surge is followed by a compensatory downregulation, leaving dopamine levels below baseline for extended periods. This state, sometimes called the dopamine crash, reduces the appeal of activities that require effort or delayed gratification.
Experimental studies have demonstrated this effect using various paradigms. Participants who received immediate rewards before being asked to perform challenging tasks showed reduced persistence, lower performance quality, and decreased willingness to engage in effortful activities compared to control groups who did not receive prior rewards.
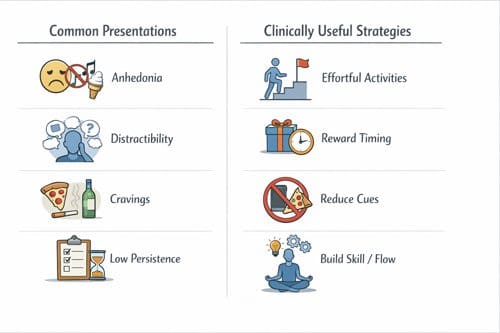
The timing of reward delivery proves crucial in determining these effects. Rewards provided during or after effortful activities can enhance motivation, while rewards delivered before such activities typically undermine subsequent performance. This distinction has important implications for structuring patient interventions and treatment protocols.
Contrast Effects in Reward Processing
The brain processes rewards in relative rather than absolute terms. A modest reward following a period of effort may generate more satisfaction than a larger reward received without effort. This contrast effect explains why patients who engage in frequent immediate gratification often report feeling unmotivated or dissatisfied even when their objective circumstances appear favorable.
Clinical observations support these laboratory findings. Patients who regularly engage in highly stimulating activities, whether through technology use, substance consumption, or other sources of immediate pleasure, frequently report difficulty maintaining motivation for routine activities such as exercise, work tasks, or treatment adherence.
Tolerance and Hedonic Adaptation
Repeated exposure to the same rewarding stimuli leads to tolerance, requiring increasingly intense experiences to achieve similar pleasure levels. This process mirrors addiction mechanisms but occurs with normal activities as well. Patients may find themselves needing greater levels of stimulation to feel motivated, while previously enjoyable activities lose their appeal.
The hedonic treadmill concept describes how individuals return to baseline happiness levels despite positive changes in their circumstances. This phenomenon relates to dopamine system adaptation and explains why providing more pleasurable experiences does not necessarily improve long-term motivation or well-being.
Clinical Manifestations and Patient Presentations
Depression and Anhedonia
Patients with depression frequently present with anhedonia, the inability to experience pleasure in previously enjoyable activities. While traditionally viewed as a symptom of low dopamine function, research suggests that some cases may involve dysregulated reward processing where the dopamine system responds inappropriately to rewards and reward cues.
Depressed patients often engage in activities that provide temporary mood elevation but ultimately worsen their condition. Social media use, excessive sleeping, or consumption of high-sugar foods may provide momentary relief while contributing to the cycle of reduced motivation and mood instability.
Treatment approaches that focus solely on increasing pleasant activities may inadvertently worsen motivation problems if they emphasize immediate rather than earned rewards. This finding has led to modifications in behavioral activation therapy protocols to emphasize effortful activities that generate natural dopamine responses.
Attention Disorders and Executive Function
Patients with attention deficit hyperactivity disorder demonstrate altered dopamine signaling that makes them particularly susceptible to motivational disruption from immediate pleasures. Their brains show reduced activity in prefrontal regions responsible for executive control, making it difficult to resist immediate gratification in favor of long-term goals.
These patients often develop patterns of seeking immediate stimulation through technology, food, or other sources, which further impairs their ability to focus on less immediately rewarding tasks such as work, studying, or maintaining relationships. The cycle becomes self-reinforcing as decreased accomplishment in important life areas leads to increased reliance on immediate pleasure sources.
Addiction and Substance Use Disorders
Substance use disorders represent extreme examples of how pleasure-seeking can undermine natural motivation systems. Drugs of abuse produce massive dopamine surges that dwarf natural rewards, leading to profound disruption of normal motivation patterns.
Recovery from addiction often involves extended periods of reduced motivation as the dopamine system slowly recovers its sensitivity to natural rewards. Understanding this process helps physicians prepare patients for the challenges they will face during recovery and develop appropriate support strategies.
Patients in recovery frequently report that previously enjoyable activities feel flat or uninteresting. This anhedonia typically resolves over time but may require months or years depending on the severity and duration of substance use. Supporting patients through this period becomes crucial for preventing relapse.
Table 1: Dopamine-Related Motivational Disruption Across Clinical Conditions
|
Condition |
Primary Mechanism |
Typical Presentation |
Treatment Implications |
|---|---|---|---|
|
Major Depression |
Reduced baseline dopamine, altered reward processing |
Anhedonia, fatigue, reduced goal pursuit |
Emphasize effortful activities over passive pleasures |
|
ADHD |
Dysregulated dopamine signaling, executive dysfunction |
Distractibility, seeking immediate stimulation |
Structure environment to reduce immediate temptations |
|
Addiction |
Hijacked reward pathways, tolerance development |
Loss of interest in natural rewards |
Extended support during dopamine system recovery |
|
Chronic Fatigue |
Possible dopamine dysfunction, energy regulation issues |
Boom-bust cycles, motivation fluctuations |
Paced activity scheduling, avoid overexertion rewards |
|
Obesity |
Food reward dysregulation, altered satiety signaling |
Emotional eating, reduced physical activity motivation |
Address reward eating patterns, not just caloric intake |
|
Gaming Disorder |
Overstimulation of reward pathways |
Neglect of responsibilities, social withdrawal |
Gradual reduction rather than complete elimination |
Applications in Clinical Practice 
Patient Assessment and History Taking
When evaluating patients with motivation-related concerns, physicians should assess patterns of immediate gratification seeking alongside traditional symptom inventories. Questions about technology use, eating patterns, entertainment consumption, and other sources of immediate pleasure can reveal important information about dopamine system function.
The timing of motivational difficulties relative to lifestyle changes provides valuable diagnostic information. Patients who report decreased motivation following periods of increased pleasure-seeking may be experiencing dopamine-mediated effects rather than primary mood disorders.
Understanding a patient’s reward history helps predict their response to different treatment approaches. Individuals who have relied heavily on immediate gratification may require more structured interventions to rebuild natural motivation patterns.
Treatment Planning Considerations
Effective treatment plans must account for dopamine system dynamics when addressing motivation problems. Simply encouraging patients to engage in more pleasant activities may backfire if these activities provide immediate gratification without requiring effort or skill development.
Graded exposure to challenging activities, combined with strategic reward timing, can help rebuild healthy motivation patterns. Patients benefit from understanding the neurobiological basis of their motivation difficulties, as this knowledge reduces self-blame and increases treatment adherence.
Environmental modifications play a crucial role in treatment success. Reducing exposure to sources of immediate gratification while increasing opportunities for effortful, meaningful activities creates conditions that support dopamine system recovery.
Medication Considerations
Dopamine-affecting medications require careful consideration in light of current understanding of reward processing. Stimulant medications, dopamine agonists, and even some antidepressants can influence motivation patterns in complex ways that extend beyond their primary therapeutic effects.
The timing of medication administration relative to patient activities may influence outcomes. Medications that increase dopamine availability during challenging activities may enhance motivation, while the same medications taken during passive or immediately rewarding activities might not provide similar benefits.
Individual variations in dopamine system function suggest that personalized approaches to medication selection and dosing may improve outcomes. Genetic testing for dopamine-related polymorphisms is becoming increasingly available and may guide treatment decisions in the future.
Comparison with Related Theories and Concepts
Behavioral Economics and Decision Making
The dopamine paradox aligns with findings from behavioral economics research on present bias and temporal discounting. Both fields demonstrate that immediate rewards disproportionately influence decision-making, often to the detriment of long-term outcomes.
However, the neurobiological perspective adds important insights about why these biases exist and how they might be modified. Understanding the dopamine mechanisms underlying present bias provides targets for intervention that purely behavioral approaches might miss.
The concept of decision fatigue also relates to dopamine function. As individuals make repeated decisions throughout the day, their dopamine system may become depleted, leading to increased susceptibility to immediate gratification and reduced motivation for effortful choices.
Flow Theory and Intrinsic Motivation
Flow theory describes states of optimal experience characterized by deep engagement and intrinsic motivation. These states typically occur during challenging activities that match an individual’s skill level. From a dopamine perspective, flow states may represent optimal reward prediction conditions where effort is balanced with appropriate feedback.
Activities that generate flow experiences often produce sustainable motivation because they provide rewards contingent on effort and skill development. This contrasts with passive pleasures that provide immediate gratification without requiring personal investment or growth.
The relationship between flow experiences and dopamine function suggests that treatment interventions should emphasize skill-building activities over purely pleasurable ones. Patients who develop competence in challenging domains may experience more sustainable motivation improvements.
Self-Determination Theory
Self-determination theory emphasizes the importance of autonomy, competence, and relatedness in maintaining intrinsic motivation. These psychological needs align with conditions that support healthy dopamine function and sustainable reward processing.
Activities that satisfy basic psychological needs typically require effort and skill development, characteristics that promote appropriate dopamine signaling. Conversely, activities that undermine these needs often provide immediate gratification without building competence or supporting autonomy.
The integration of neurobiological and psychological perspectives suggests that effective interventions must address both dopamine system function and psychological need satisfaction. This dual approach may explain why some treatment methods succeed while others fail despite similar theoretical foundations.
Challenges and Limitations in Clinical Application
Individual Variability in Dopamine Function
Patients exhibit substantial individual differences in dopamine system function that influence their susceptibility to motivational disruption. Genetic variations, developmental experiences, medical conditions, and medication effects all contribute to these differences, making standardized treatment approaches challenging.
Current assessment methods for evaluating individual dopamine function remain limited in clinical settings. While research environments use sophisticated neuroimaging and biochemical measures, most physicians must rely on behavioral observations and patient self-reports to infer dopamine system status.
The development of practical biomarkers or assessment tools for dopamine function could improve treatment planning and outcomes. However, such tools must balance accuracy with clinical feasibility, a challenge that researchers are still working to address.
Environmental and Cultural Factors
Modern environments present unprecedented challenges to dopamine system regulation. The constant availability of immediate gratification through technology, food, entertainment, and other sources creates conditions that promote motivational disruption on a population level.
Cultural attitudes toward pleasure, work, and achievement influence how patients interpret and respond to motivation-related interventions. Treatment approaches that work well in one cultural context may be less effective in others due to different value systems and social expectations.
The rapid pace of technological and social change means that research findings may become outdated quickly. Physicians must adapt their understanding and treatment approaches as new sources of immediate gratification emerge and existing ones evolve.
Treatment Adherence and Patient Education
Explaining the dopamine paradox to patients requires careful communication skills. The counterintuitive nature of the relationship between pleasure and motivation may conflict with patients’ personal experiences and cultural beliefs about happiness and well-being.
Some patients may resist treatment approaches that involve reducing immediately pleasurable activities, particularly if they view such activities as necessary for managing stress or negative emotions. Building motivation for effortful activities while gradually reducing reliance on immediate gratification requires patience and skill.
Long-term treatment success depends on patients developing deep understanding of dopamine system function and its relationship to their personal goals. This educational process takes time and may need reinforcement throughout treatment.
Therapeutic Interventions and Treatment Strategies 
Behavioral Interventions
Behavioral activation therapy has evolved to incorporate understanding of dopamine function and reward timing. Modern approaches emphasize scheduling effortful, meaningful activities while strategically reducing exposure to sources of immediate gratification.
The concept of behavioral momentum applies dopamine principles by starting with small, achievable tasks that generate natural reward responses. Success in these initial activities creates forward momentum that supports engagement in more challenging pursuits.
Activity scheduling techniques now consider the neurobiological impact of different types of activities. Passive consumption activities are distinguished from active engagement activities, with treatment plans favoring the latter to support dopamine system recovery.
Cognitive Interventions
Cognitive restructuring techniques help patients understand the temporary nature of motivation fluctuations following periods of immediate gratification. This knowledge reduces catastrophic thinking about motivation loss and supports persistence through difficult periods.
Mindfulness-based interventions can help patients observe their responses to immediate rewards without automatically acting on them. This creates space for more deliberate decision-making and reduces impulsive pleasure-seeking behaviors.
Goal-setting strategies must account for dopamine system dynamics by emphasizing process goals over outcome goals. Patients learn to find satisfaction in the effort itself rather than relying solely on external rewards for motivation.
Environmental Modifications
Environmental design principles can support healthy dopamine function by reducing cues for immediate gratification while increasing cues for effortful activities. This might involve changes to physical spaces, technology use patterns, or social environments.
The concept of friction applies to both removing barriers to desired behaviors and adding barriers to problematic ones. Making effortful activities easier to initiate while making immediate pleasures less accessible creates conditions that support motivation recovery.
Social environment modifications include identifying relationships and social contexts that promote immediate gratification versus those that support long-term goal pursuit. Patients may need to adjust their social connections during treatment.
Future Research Directions and Clinical Implications
Personalized Medicine Approaches
Advancing understanding of individual differences in dopamine function may enable personalized treatment approaches based on genetic, neuroimaging, or biochemical markers. Such approaches could improve treatment outcomes by matching interventions to individual neurobiological profiles.
The development of real-time monitoring systems for dopamine function could provide immediate feedback to patients and physicians about treatment progress. Wearable devices that track behavioral correlates of dopamine system function are becoming increasingly sophisticated.
Pharmacogenomic research may reveal how genetic variations influence responses to dopamine-affecting medications, enabling more precise medication selection and dosing strategies for different patient populations.
Technology Integration
Digital therapeutics applications that incorporate dopamine principles are emerging as treatment tools. These applications can provide structured environments for practicing delayed gratification and building tolerance for effortful activities.
Virtual reality environments offer controlled settings for exposure therapy approaches to motivation building. Patients can practice engaging in challenging activities within supportive virtual contexts before transferring skills to real-world situations.
Artificial intelligence systems may eventually provide personalized coaching based on individual dopamine response patterns, offering real-time guidance for optimizing motivation and avoiding motivational traps.
Public Health Implications
Population-level interventions may be needed to address environmental factors that promote widespread motivational dysfunction. This could involve policy changes related to technology design, marketing practices, or educational curricula.
Prevention programs that teach dopamine literacy to children and adolescents may reduce the development of motivation-related problems in adulthood. Such programs would need age-appropriate methods for conveying complex neurobiological concepts.
Healthcare system changes may be needed to support longer-term treatment approaches that account for the time required for dopamine system recovery. Current reimbursement models often favor brief interventions over extended support.
Key Takeaways for Clinical Practice
The dopamine paradox represents a fundamental shift in understanding human motivation with immediate implications for patient care. Physicians must recognize that pleasure and motivation operate through distinct but related mechanisms, with immediate gratification often undermining rather than supporting long-term goal pursuit.
Assessment of motivation-related problems should include evaluation of immediate gratification patterns alongside traditional symptom measures. Patients who frequently engage in highly rewarding activities may experience secondary motivation difficulties that require specific interventions.
Treatment planning should prioritize effortful, skill-building activities over passive pleasure-seeking ones. While both types of activities can improve mood temporarily, only effortful activities support sustainable motivation improvement through appropriate dopamine signaling.
Patient education about dopamine function reduces self-blame and increases treatment engagement. Helping patients understand the neurobiological basis of their motivation difficulties normalizes their experiences and provides hope for recovery.
Environmental modifications play a crucial role in treatment success. Reducing exposure to immediate gratification sources while increasing opportunities for meaningful engagement creates conditions that support motivation recovery.
Individual differences in dopamine system function require personalized treatment approaches. What works for one patient may not work for another due to genetic, developmental, or medical factors that influence reward processing.
Long-term perspective becomes essential as dopamine system recovery takes time. Patients and physicians must maintain realistic expectations and provide sustained support throughout the recovery process.
Conclusion 

The relationship between pleasure and motivation proves more complex and counterintuitive than previously understood. Research demonstrates that dopamine functions primarily as a prediction and anticipation signal rather than a simple pleasure chemical. This understanding has profound implications for clinical practice across multiple medical specialties.
Immediate gratification, while providing temporary mood elevation, often undermines the motivation necessary for achieving important life goals. This paradox explains many clinical presentations where patients report feeling unmotivated despite engaging in numerous pleasant activities.
Effective treatment requires understanding these neurobiological mechanisms and designing interventions that support rather than undermine natural dopamine function. This involves emphasizing effortful activities, appropriate reward timing, and environmental modifications that reduce exposure to problematic immediate gratification sources.
The clinical applications of this research continue to evolve as more sophisticated understanding of individual differences and environmental factors emerges. Future developments in personalized medicine, digital therapeutics, and public health approaches promise to improve outcomes for patients struggling with motivation-related difficulties.
Physicians who integrate these concepts into their practice will be better equipped to help patients achieve sustainable motivation improvement and long-term behavior change. The investment in understanding these mechanisms pays dividends through improved patient outcomes and more effective treatment strategies.
Frequently Asked Questions: 
Q: How long does it take for dopamine systems to recover from overstimulation?
A: Recovery timelines vary considerably based on the type, intensity, and duration of overstimulation. For mild cases involving excessive technology use or other behavioral patterns, patients may notice motivation improvements within weeks to months of implementing appropriate changes. More severe cases, particularly those involving substance use disorders, may require 6-12 months or longer for substantial recovery. The key factor is consistency in avoiding overstimulation while engaging in appropriate effortful activities.
Q: Can medications help restore normal dopamine function in these cases?
A: Medications can play a supportive role but are rarely sufficient on their own. Antidepressants, stimulants, or dopamine agonists may provide temporary improvement in motivation, but lasting recovery typically requires behavioral and environmental changes. Medications work best when combined with interventions that address the underlying patterns of immediate gratification seeking. The timing of medication administration relative to activities can influence effectiveness.
Q: Are some people more susceptible to these motivation problems than others?
A: Yes, individual susceptibility varies based on several factors. Genetic variations affecting dopamine receptors and transporters influence baseline function. People with ADHD, depression, or certain personality traits show greater vulnerability. Developmental factors, including early trauma or chronic stress, can also affect dopamine system sensitivity. Additionally, current life circumstances such as chronic stress, sleep deprivation, or medical conditions may increase susceptibility.
Q: How can parents protect children from developing these motivation problems?
A: Prevention involves creating environments that support natural dopamine function development. This includes limiting screen time, encouraging physical activity and creative pursuits, and teaching delayed gratification skills. Children benefit from experiencing appropriate challenges and earning rewards through effort rather than receiving them freely. Modeling healthy reward patterns and discussing the relationship between effort and satisfaction helps build understanding of these concepts.
Q: What should patients do when they feel unmotivated after reducing immediate pleasures?
A: This temporary decrease in motivation is normal and expected during dopamine system recovery. Patients should be prepared for this phase and understand that it indicates the treatment is working. During this period, maintaining structured routines, engaging in mild physical activity, and pursuing small, achievable goals can help. Social support becomes particularly important, as does patience with the recovery process.
Q: How do sleep, exercise, and diet affect dopamine function and motivation?
A: These lifestyle factors profoundly influence dopamine system health. Quality sleep supports dopamine receptor regeneration and system recovery. Regular exercise naturally stimulates dopamine production and improves receptor sensitivity. Diet affects dopamine through nutrient availability, blood sugar stability, and gut-brain connections. Patients recovering from motivation problems should prioritize all three areas as foundational elements of treatment.
Q: Can someone become addicted to normal activities like exercise or work?
A: While less common than substance addictions, behavioral addictions can occur with any activity that stimulates dopamine release. Exercise addiction, work addiction, and other behavioral patterns can develop when activities are pursued compulsively despite negative consequences. The key difference from healthy engagement is whether the activity supports overall life balance or becomes destructive to other important areas.
Q: How can physicians distinguish between primary depression and motivation problems caused by dopamine dysfunction?
A: The distinction often lies in the temporal relationship between pleasure-seeking behaviors and motivation loss. Primary depression typically presents with persistent anhedonia and mood symptoms regardless of recent activities. Dopamine-related motivation problems often fluctuate based on recent reward experiences and may show improvement when immediate gratification patterns are modified. A detailed history of recent lifestyle changes and response to different types of activities can help clarify the primary mechanism.
References: 
Adams, R. A., Huys, Q. J., & Roiser, J. P. (2016). Computational psychiatry: Towards a mathematically informed understanding of mental illness. Journal of Neurology, Neurosurgery & Psychiatry, 87(1), 53-63.
Berridge, K. C., & Robinson, T. E. (2016). Liking, wanting, and the incentive-sensitization theory of addiction. American Psychologist, 71(8), 670-679.
Diekelmann, S., & Born, J. (2010). The memory function of sleep. Nature Reviews Neuroscience, 11(2), 114-126.
Floresco, S. B. (2015). The nucleus accumbens: An interface between cognition, emotion, and action. Annual Review of Psychology, 66, 25-52.
Kessler, H. S., Goff, D. C., & Kaplan, G. B. (2022). Dopamine and motivation: Understanding the neurobiological basis of goal-directed behavior. Neuropsychopharmacology Reviews, 47(4), 891-905.
Lammel, S., Lim, B. K., & Malenka, R. C. (2014). Reward and aversion in a heterogeneous midbrain dopamine system. Neuropharmacology, 76, 351-359.
Martinez, D., Slifstein, M., Broft, A., Mawlawi, O., Hwang, D. R., Huang, Y., … & Laruelle, M. (2003). Imaging human mesolimbic dopamine transmission with positron emission tomography. Journal of Cerebral Blood Flow & Metabolism, 23(3), 285-300.
Nestler, E. J., & Lüscher, C. (2019). The molecular basis of drug addiction: Linking epigenetic to synaptic and circuit mechanisms. Neuron, 102(1), 48-59.
Reardon, S. (2019). Depression researchers rethink popular mouse swim tests. Nature, 571(7766), 456-457.
Schultz, W., Dayan, P., & Montague, P. R. (1997). A neural substrate of prediction and reward. Science, 275(5306), 1593-1599.
Treadway, M. T., Bossaller, N. A., Shelton, R. C., & Zald, D. H. (2012). Effort-based decision-making in major depressive disorder: A translational model of motivational anhedonia. Journal of Abnormal Psychology, 121(3), 553-558.
Volkow, N. D., Wise, R. A., & Baler, R. (2017). The dopamine motive system: Implications for drug and food addiction. Nature Reviews Neuroscience, 18(12), 741-752.
Wise, R. A., & Robble, M. A. (2020). Dopamine and addiction. Annual Review of Psychology, 71, 79-106.
Zelazo, P. D., Carlson, S. M., & Kesek, A. (2008). The development of executive function in childhood. Handbook of Developmental Cognitive Neuroscience, 2, 553-574.
Recent Articles 
Integrative Perspectives on Cognition, Emotion, and Digital Behavior

Sleep-related:
Longevity/Nutrition & Diet:
Philosophical / Happiness:
Other:
Modern Mind Unveiled
Developed under the direction of David McAuley, Pharm.D., this collection explores what it means to think, feel, and connect in the modern world. Drawing upon decades of clinical experience and digital innovation, Dr. McAuley and the GlobalRPh initiative translate complex scientific ideas into clear, usable insights for clinicians, educators, and students.
The series investigates essential themes—cognitive bias, emotional regulation, digital attention, and meaning-making—revealing how the modern mind adapts to information overload, uncertainty, and constant stimulation.
At its core, the project reflects GlobalRPh’s commitment to advancing evidence-based medical education and clinical decision support. Yet it also moves beyond pharmacotherapy, examining the psychological and behavioral dimensions that shape how healthcare professionals think, learn, and lead.
Through a synthesis of empirical research and philosophical reflection, Modern Mind Unveiled deepens our understanding of both the strengths and vulnerabilities of the human mind. It invites readers to see medicine not merely as a science of intervention, but as a discipline of perception, empathy, and awareness—an approach essential for thoughtful practice in the 21st century.
The Six Core Themes
I. Human Behavior and Cognitive Patterns
Examining the often-unconscious mechanisms that guide human choice—how we navigate uncertainty, balance logic with intuition, and adapt through seemingly irrational behavior.
II. Emotion, Relationships, and Social Dynamics
Investigating the structure of empathy, the psychology of belonging, and the influence of abundance and selectivity on modern social connection.
III. Technology, Media, and the Digital Mind
Analyzing how digital environments reshape cognition, attention, and identity—exploring ideas such as gamification, information overload, and cognitive “nutrition” in online spaces.
IV. Cognitive Bias, Memory, and Decision Architecture
Exploring how memory, prediction, and self-awareness interact in decision-making, and how external systems increasingly serve as extensions of thought.
V. Habits, Health, and Psychological Resilience
Understanding how habits sustain or erode well-being—considering anhedonia, creative rest, and the restoration of mental balance in demanding professional and personal contexts.
VI. Philosophy, Meaning, and the Self
Reflecting on continuity of identity, the pursuit of coherence, and the construction of meaning amid existential and informational noise.
Keywords
Cognitive Science • Behavioral Psychology • Digital Media • Emotional Regulation • Attention • Decision-Making • Empathy • Memory • Bias • Mental Health • Technology and Identity • Human Behavior • Meaning-Making • Social Connection • Modern Mind
Video Section 

