Intelligence Of Offspring Related To Parental Obesity
Overview
The impact of maternal obesity on childhood cognitive development remains uncertain. Previous research has often lacked proper adjustments for key confounding factors, and preterm children, who represent a distinct developmental group, have been underexplored.
This study aimed to investigate whether maternal prepregnancy body mass index (BMI) influences the intelligence quotient (IQ) of children by age 5 and whether this relationship varies based on gestational age.
Data were analyzed from two French birth cohorts: EDEN (including children of all gestational ages) and EPIPAGE-2 (focused on preterm children born between 24 and 34 weeks of gestation). Maternal prepregnancy BMI was calculated using self-reported weight and height, and child IQ was measured using the Wechsler Preschool and Primary Scale of Intelligence at approximately 5 years. Confounding factors, such as socioeconomic status and paternal BMI, were accounted for in multivariable models.
The analysis included 1100 children from EDEN and 2629 from EPIPAGE-2. Among the children, lower intellectual functioning (defined as a full-scale IQ below 85) was observed in 8.1% in EDEN and 19.6% in EPIPAGE-2. Maternal obesity prevalence was higher among children with lower intellectual functioning (13.6% in EDEN and 21.3% in EPIPAGE-2) compared to those with normal intellectual functioning (8.9% in EDEN and 12.9% in EPIPAGE-2).
Maternal prepregnancy obesity was linked to an approximate 3-point reduction in full-scale IQ scores after adjusting for confounders. Specifically, the adjusted β was −2.8 (95% confidence interval [CI]: −5.6, −0.1) in EDEN and −2.6 (95% CI: −4.7, −0.6) in EPIPAGE-2. In EDEN, maternal obesity primarily affected verbal IQ scores, while in EPIPAGE-2, the impact extended to verbal, reasoning, and processing IQ domains. Adjusting for paternal BMI did not significantly alter these findings.
Higher maternal prepregnancy BMI is associated with reduced cognitive development in children at around 5 years of age, with distinct domain-specific effects observed among preterm children. This highlights the importance of maternal health in early childhood developmental outcomes.
Introduction
Maternal obesity is a growing global concern, with prevalence rates reaching as high as 70% in some regions. This trend is alarming due to its association with a heightened risk of adverse obstetric outcomes, including stillbirth, preterm birth, gestational diabetes, and pre-eclampsia. Furthermore, maternal obesity can have long-term health consequences for offspring, such as an increased risk of developing obesity and cardiovascular disease later in life.
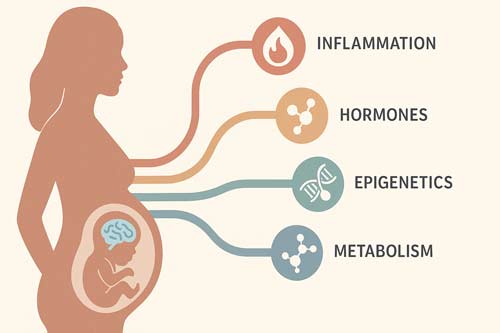
Emerging evidence also suggests a link between maternal obesity and the neurodevelopment of offspring. Studies indicate that children born to mothers with obesity before pregnancy are at a greater risk of developing conditions such as depression, anxiety, and schizophrenia. Although the biological mechanisms underlying these associations remain unclear, hypotheses include maternal inflammation, hormonal imbalances, metabolic changes, and epigenetic alterations. Additionally, there is speculation that these effects may not be purely intrauterine but could also result from shared genetic or environmental factors. This makes paternal body mass index (BMI) a valuable tool in research, as it can help determine whether the observed effects are influenced by familial or genetic factors rather than direct maternal contributions.
Research into the relationship between maternal obesity and offspring cognitive development has yielded mixed results. Around half of the studies on this topic report adverse impacts on general cognitive abilities, intelligence quotient (IQ), and language development. However, many of these studies fail to adequately account for potential confounding factors, such as socioeconomic status, maternal mental health, lifestyle, and parity. Moreover, limited attention has been given to the impact of maternal obesity on preterm-born children, a group already vulnerable to cognitive impairments, which worsen with decreasing gestational age.
Among the few studies focusing on preterm-born children, findings suggest that maternal obesity may impair cognitive outcomes. However, these studies primarily involve children born extremely preterm (<28 or ≤30 weeks gestation) and are limited by small sample sizes and incomplete adjustment for confounding variables, such as maternal age and mental health. This raises the possibility that preterm-born children, being developmentally and immunologically less mature, might be more susceptible to the perinatal effects of maternal obesity. Conversely, term-born children, having experienced longer exposure to maternal obesity, may also face significant risks.
Given that maternal obesity is a risk factor for preterm birth and has potential implications for both preterm and term-born children, it is critical to explore this relationship in greater depth. The present study aims to investigate the association between maternal prepregnancy obesity and offspring IQ at approximately five years of age, using data from two French birth cohorts. The analysis considers children born across a spectrum of gestational ages (24–34 weeks and term) while accounting for important confounding factors, such as socioeconomic status and maternal age, and incorporating paternal BMI as a negative control. This approach seeks to provide a comprehensive understanding of how maternal obesity impacts cognitive outcomes in early childhood.
Method
From 2003 to 2006, pregnant women (<24 weeks gestation) were enrolled in Nancy and Poitiers maternity wards in France. Eligibility required a singleton pregnancy, no pre-existing diabetes, literacy in French, and residency in the region during the study. Of the 2002 participants, data on maternal and child health were collected via questionnaires, clinical evaluations, and cognitive assessments, spanning pregnancy to the child’s age of 12.
Recruitment took place in 2011 across 25 French regions, targeting pregnancies between 22 and 34 weeks gestation, including live births, stillbirths, and terminations. Infants were classified by gestational age: extremely preterm (22–26 weeks), very preterm (27–31 weeks), or moderately preterm (32–34 weeks). Weighted analyses were used to address recruitment period variations. Among the 7804 enrolled infants, 4467 survived neonatal care. Data were gathered through medical records and parent or physician-completed questionnaires at birth and during follow-ups (e.g., at 2 years).
Both studies adhered to rigorous ethical standards. EPIPAGE-2 received approval from the National Data Protection Authority and ethics committees, while the EDEN cohort was approved by the Bicêtre Hospital Ethics Committee and CNIL.
In EDEN, midwives measured maternal height, and pre-pregnancy weight was self-reported (24–26 weeks gestation). In EPIPAGE-2, both parameters were extracted from medical records during the first antenatal visit. BMI categories followed WHO standards: underweight (<18.5 kg/m²), normal (18.5–24.9 kg/m²), overweight (25–29.9 kg/m²), and obese (≥30 kg/m²).
Cognitive assessments at 5–6 years (EDEN, WPPSI-III) and 5.5 years (EPIPAGE-2, WPPSI-IV) were conducted by trained psychologists. The WPPSI measures IQ across various domains (e.g., verbal, performance, processing speed), with composite scores representing overall cognitive ability. Children scoring <85 on Full-Scale IQ (FSIQ) were categorized as having borderline or lower intellectual functioning.
Both cohorts collected extensive data, including parental demographics (age, education, employment, income), maternal lifestyle (diet, physical activity, smoking, alcohol), and pregnancy characteristics (e.g., gestational weight gain, complications, delivery type). Child variables included sex, birth weight, and gestational age.
Statistical and Sensitivity Analyses
Attrition bias at 5 years was addressed through inverse probability weighting. Logistic regression models (EDEN) and generalized estimating equations (EPIPAGE-2) evaluated associations between maternal BMI and child IQ. Adjustments included potential confounders identified via literature review and directed acyclic graphs. Sensitivity analyses excluded extreme outliers (FSIQ <60) and adjusted for additional maternal lifestyle factors during pregnancy.
Result
In the EDEN cohort, 8.1% of children demonstrated lower intellectual functioning (FSIQ < 85) by age five, compared to 19.6% in the EPIPAGE-2 cohort. Children with lower intellectual functioning often had mothers with indicators of lower socioeconomic status. Additionally, in EPIPAGE-2, these mothers were more likely to have higher prepregnancy BMI, a greater number of prior births, and children born at earlier gestational ages or with lower birthweights.

Unadjusted analyses revealed that maternal prepregnancy obesity was associated with a 4- to 5-point reduction in FSIQ in both cohorts compared to children of mothers with normal BMI. After adjusting for various factors, this reduction was approximately 3 points (adjusted β −2.8 in EDEN and −2.6 in EPIPAGE-2). The risk of lower intellectual functioning in children of obese mothers was modestly higher in EPIPAGE-2 (aRR 1.32) compared to EDEN (aRR 1.16). Maternal overweight, while associated with a smaller impact on FSIQ (1–1.5 point reduction), showed a slightly increased risk of lower intellectual functioning in both cohorts.
In EDEN, prepregnancy obesity correlated with a 3-point reduction in performance and verbal IQ. In EPIPAGE-2, the reductions spanned multiple domains, with reasoning, verbal, and processing skills showing a 2–3 point decline, while visual–spatial and memory domains experienced smaller reductions. Maternal overweight was associated with smaller negative effects in most domains, except for a slightly greater impact on visual–spatial IQ and a minimal positive association with reasoning IQ.
Adjusting for paternal BMI did not significantly alter the relationship between maternal BMI and offspring FSIQ in either cohort. Paternal BMI as a primary factor showed no significant association with offspring IQ. Adjustments for maternal lifestyle during pregnancy slightly increased the observed effects of maternal obesity in EDEN but had minimal impact in EPIPAGE-2.
Maternal prepregnancy obesity demonstrates a dose-dependent association with a reduction in offspring FSIQ, with an approximate 3-point decrease in both term and preterm children. Overweight mothers showed smaller reductions (<2 points). These patterns were consistent across most IQ domains, with maternal obesity exhibiting the most pronounced effects. Paternal BMI and other factors had limited influence on these findings.
The study leverages two large cohorts, including one of preterm-born children, to examine a broad range of gestational ages. IQ was assessed by trained professionals using validated tools, and key confounders, such as maternal lifestyle and paternal BMI, were considered. Methodological approaches, such as multiple imputations, minimized potential biases.
The study faced challenges including limited statistical power in EDEN and potential biases in EPIPAGE-2 due to its exclusive focus on preterm births. Missing data on maternal prepregnancy lifestyle, postnatal environment, and maternal IQ may have contributed to residual confounding. The cohorts predominantly included women of higher socioeconomic status, potentially limiting generalizability to the broader French population. Additionally, self-reported maternal weight, while reliable, introduces some variability.
These findings underline the importance of addressing maternal health and prepregnancy weight as factors influencing early cognitive outcomes in children.
Conclusion
Maternal prepregnancy obesity appears to have a significant, albeit modest, impact on offspring Full-Scale Intelligence Quotient (FSIQ), with a decrease of approximately 3 points observed. While this change might seem minor on an individual level, its implications at the population level could be considerable, particularly given the widespread prevalence of maternal obesity. This decrease aligns with findings from the EDEN cohort, where it represents a comparable difference in IQ between children born at term and those born a month preterm. Such variations, though subtle, may hold public health relevance by influencing human capital across generations.
Previous research investigating the relationship between maternal obesity and child IQ has faced limitations, particularly in accounting for key confounding factors. Few studies have focused on preterm populations. However, a meta-analysis of six studies has suggested a small but consistent negative effect of maternal overweight and obesity on cognitive outcomes in children aged 1 to 10 years. Supporting this trend, other research has identified a 2-point reduction in FSIQ for children of obese mothers. Conversely, some studies have reported unexpected positive associations between maternal obesity and cognitive outcomes, which may stem from small sample sizes, diverse study populations, or insufficient control of variables like socioeconomic status and maternal lifestyle.
Fewer studies have explored the impact of maternal obesity on the cognitive development of preterm infants. In one small cohort of infants born ≤30 weeks gestation, maternal obesity was linked to reduced language scores at age 2 but not overall cognitive scores. Another study found maternal obesity nearly doubled the risk of cognitive impairment in infants born before 28 weeks gestation. Both studies, however, were limited by small sample sizes and a lack of control for critical confounders, such as maternal age and mental health. In contrast, the present study accounted for these factors while examining a broader gestational age range and used paternal BMI as a negative control to address familial and genetic confounding. The results suggest an intrauterine effect of maternal obesity on offspring intelligence, supported by the absence of an association between paternal BMI and offspring IQ.

The biological mechanisms underlying this association may include chronic low-grade inflammation linked to obesity, which can elevate pro-inflammatory cytokine levels in the placenta and fetal environment. These inflammatory responses have been associated with altered brain development, neuropsychiatric disorders, and behavioral issues. Other potential mechanisms include maternal metabolic changes, vitamin D deficiency, hormonal alterations, and epigenetic modifications triggered by maternal behaviors. Despite these hypotheses, certain studies have failed to find significant links between maternal obesity and abnormal neonatal brain structures, highlighting the need for further research. For instance, studies using mediation analyses have suggested that inflammatory markers like CRP might partially explain the observed cognitive outcomes, though the direct link to intelligence remains inconclusive.
In conclusion, maternal prepregnancy BMI has a dose-dependent relationship with offspring FSIQ, with obesity correlating to an approximate 3-point decrease and overweight contributing to smaller declines. These associations were consistent across both term and preterm populations. Future research should prioritize identifying the precise biological pathways responsible for this relationship to better inform interventions and public health strategies.
