Tau Accumulation And White Matter Changes Linked To Hypertension
Overview
This study explored how amyloid buildup and hypertension interact to affect tau accumulation and atrophy in the entorhinal cortex (EC), while also investigating cerebral blood flow (CBF) as a potential shared mechanism. The researchers analyzed data from two cohorts of older adults without dementia: participants from the Add-Tau study (n = 138) and the Alzheimer’s Disease Neuroimaging Initiative (ADNI) (n = 523). These individuals had undergone amyloid-PET, tau-PET, fluid-attenuated inversion recovery (FLAIR), and T1-weighted MRI scans. A subset also had arterial spin labeling (ASL) MRI data available (Add-Tau: n = 78; ADNI: n = 89).
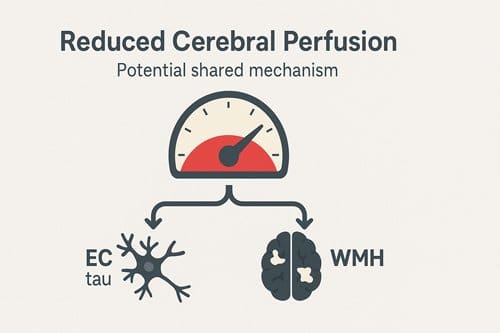
The findings revealed that the harmful impact of hypertension on Alzheimer’s pathology and EC thinning was more significant in the Add-Tau cohort. In the ADNI group, higher amyloid levels were linked to reduced cerebral blood flow in the occipital gray matter. Across both cohorts, lower gray matter CBF was associated with elevated tau in the EC and increased white matter hyperintensities (WMHs). The study concluded that reduced cerebral perfusion might serve as a common pathway through which amyloid and hypertension contribute to tau accumulation and white matter changes.
Introduction
Hypertension is a key factor contributing to subclinical brain damage, often leading to cognitive decline in older adults through various mechanisms. One well-understood pathway is through vascular brain damage, such as the development of white matter lesions. A second, less explored pathway may involve Alzheimer’s disease (AD) pathology, where hypertension either directly promotes amyloid beta (Aβ) accumulation or interacts with Aβ to enhance tau protein pathology. These mechanisms potentially converge in the medial temporal lobe (MTL), a critical area for episodic memory, resulting in its atrophy. The interplay between hypertension and AD pathology remains complex, underscoring the need for a deeper understanding to improve treatment approaches and risk assessment strategies.
A noteworthy link between hypertension and AD pathology is evident in the entorhinal cortex (EC), part of the MTL. The EC is an early site of neuronal damage and volume loss in aging and AD. Studies have found associations between vascular disease and tau pathology in the EC, independent of Aβ, as well as synergistic effects of vascular risk factors and Aβ on MTL tau burden and atrophy. Hypertension also increases the risk of white matter hyperintensities (WMHs), which have been linked to tau pathology, reduced MTL volume, and EC atrophy. Although WMHs are most strongly associated with deep frontal regions, EC atrophy is more pronounced when WMHs are found in the occipital and parietal lobes.
A common mechanism for these processes may involve impaired blood flow to affected brain regions. Both Aβ accumulation and chronic hypertension reduce cerebral blood flow (CBF), with ischemia playing a significant role in WMH development. Animal studies on chronic cerebral hypoperfusion have shown increased soluble tau levels, suggesting that ischemia could drive tau pathology. Thus, reduced CBF may not only exacerbate brain damage but also contribute to the progression of core AD processes.
This study aimed to examine how hypertension and AD pathology may together contribute to EC atrophy and memory decline. The hypothesis was that associations between hypertension, WMHs, and EC tau differ based on the presence of Aβ pathology and the specific lobar region where WMHs are present. Additionally, the study proposed that reduced CBF could serve as a shared pathway by which both Aβ and hypertension contribute to EC tau and WMH burden.
Method
This study analyzed data from 141 participants without dementia, part of a longitudinal clinical trial at the University of Zurich, Switzerland (Add-Tau study: NCT02958670). Participants had undergone amyloid-beta (Aβ) and tau PET scans and were volunteers recruited from previous studies involving Aβ imaging through newspaper ads. After exclusions due to imaging errors, 138 participants were included in the final analysis. Of these, cerebral blood flow (CBF) estimates were available for a subsample of 78 individuals. Cognitive status was determined according to consensus criteria, with participants classified as either cognitively unimpaired or having mild cognitive impairment (MCI).
Given the relatively low Aβ burden in the Add-Tau cohort, the analysis was extended to data from the Alzheimer’s Disease Neuroimaging Initiative (ADNI), which included 523 participants without dementia, all with Aβ-PET, tau-PET, memory assessments, and other imaging data. After excluding participants with low-quality scans, CBF estimates were obtained for 89 individuals. ADNI participants were also classified as cognitively unimpaired or MCI based on standardized criteria. The data from both cohorts were used to examine the impact of hypertension and Aβ on cerebral perfusion, tau pathology, and white matter changes.
MRI and PET acquisition protocols varied between the two cohorts, with MRI scans from the Add-Tau cohort acquired using a 3T General Electric (GE) scanner, while those from ADNI were captured using a mix of Siemens, GE, and Philips scanners. Aβ deposition was measured using [18F]-flutemetamol or [11C]-Pittsburgh Compound-B in Add-Tau, and [18F]-florbetapir or [18F]-florbetaben in ADNI. Both studies followed standardized protocols for data collection and preprocessing, including the use of FreeSurfer for image segmentation and the lesion segmentation toolbox (LST) for white matter hyperintensity (WMH) analysis.
Key findings highlighted that hypertension may contribute to Alzheimer’s disease (AD) development by reducing cerebral perfusion, linking it with Aβ and tau pathology as well as white matter damage. Preventive hypertension control was suggested as a potential strategy to reduce AD risk through both AD-related and independent mechanisms. Future studies were recommended to investigate longitudinal associations between hypertension, cerebral blood flow, and AD pathology, as well as the effects of controlling blood pressure on reducing AD-related changes.
The study employed statistical models to explore the relationships between hypertension, regional WMH burden, tau pathology, and episodic memory, considering Aβ status as a moderating factor. Sensitivity analyses were conducted to account for outliers, and models were adjusted for factors such as age, APOE ε4 status, and disease progression. Statistical software packages in R were used for data analysis, ensuring robust handling of missing data through full-information maximum likelihood estimation.
Result
The study compares the characteristics of two cohorts, Add-Tau and ADNI, focusing on amyloid-beta (Aβ) positivity and its association with white matter hyperintensities (WMH), hypertension, and other factors. In the Add-Tau cohort, 26% of participants were Aβ+, while the ADNI cohort had a higher rate of Aβ+ participants at 44.7%. In the Add-Tau group, Aβ+ participants displayed greater deep frontal WMH volume and a higher likelihood of hypertension, though Aβ+ individuals with hypertension did not show an increased Aβ burden. In contrast, the ADNI cohort showed that Aβ+ participants had elevated WMH volumes in the occipital, parietal, and deep frontal regions, but hypertension prevalence did not differ significantly between Aβ+ and Aβ− groups.
Further analyses revealed that in the Add-Tau cohort, after adjusting for age, sex, and APOE ε4 status, Aβ+ individuals were more likely to have hypertension, though no significant regional WMH burden differences were found. In the ADNI cohort, Aβ+ individuals demonstrated increased occipital and parietal WMH burden after adjusting for covariates, though deep frontal WMH volume was not significantly different. Hypertension in Aβ+ individuals in the Add-Tau cohort was linked to higher tau pathology in the entorhinal cortex (EC), whereas WMH burden was associated with reduced EC thickness, particularly in the occipital region. Notably, the ADNI cohort revealed stronger associations between EC tau and memory decline in Aβ+ individuals compared to Aβ− participants.
The study also explored the effects of cerebral blood flow (CBF) on the relationship between hypertension, Aβ burden, and WMH or tau pathology. In the Add-Tau cohort, hypertension was associated with reduced frontal CBF but not with regional WMH burden or CBF in the occipital and parietal regions. In contrast, the ADNI cohort demonstrated that higher Aβ burden correlated with lower CBF in the occipital region. Additionally, lower CBF in the medial temporal lobe (MTL) was associated with increased EC tau in Aβ+ individuals in both cohorts, further suggesting that CBF may mediate the relationship between hypertension, Aβ burden, and tau pathology.
The findings suggest that hypertension, Aβ burden, and CBF are interconnected with varying implications for WMH burden, tau pathology, and cognitive outcomes depending on the cohort and disease stage. Furthermore, the results highlight the complexity of interactions between vascular risk factors, amyloid pathology, and neurodegeneration, which may differ across individuals based on their Aβ status and other covariates.
Conclusion
The study examined the effects of hypertension on brain health by analyzing two independent cohorts: one with a low amyloid-beta (Aβ) burden (Add-Tau cohort) and another in more advanced stages of Alzheimer’s disease (AD) with a high Aβ burden (ADNI cohort). The findings suggest that hypertension negatively impacts brain health through both Alzheimer’s disease (AD)-dependent and AD-independent mechanisms. Additionally, both Aβ and hypertension were identified as contributing factors to increased white matter hyperintensities (WMH) and entorhinal cortex (EC) tau, particularly in the posterior regions of the brain. This may occur via a shared pathway, with impaired cerebral perfusion as a potential factor.
Hypertension was found to be a significant risk factor for increased WMH volume and medial temporal lobe (MTL) atrophy, with a strong connection to tau pathology, both independently and in conjunction with Aβ. In the Add-Tau cohort, hypertensive individuals were more likely to be Aβ-positive, which was associated with lower EC thickness and higher EC tau, particularly when Aβ burden was elevated. These concurrent mechanisms indicate that some effects of hypertension depend on the presence of Aβ. Specifically, the study revealed that occipital WMH burden was linked to reduced EC thickness in individuals with Aβ, and that hypertension, when interacting with Aβ, predicted higher EC tau. Elevated EC tau levels were strongly correlated with reduced EC thickness and poorer episodic memory performance.
In the ADNI cohort, the relationship between hypertension and AD pathology was less pronounced. Hypertension primarily affected EC thickness through increased WMH burden. However, hypertension’s association with WMH burden in the parietal and deep frontal regions persisted, highlighting how these processes may vary in different brain regions. These findings emphasize the complex, interconnected relationship between vascular health and AD pathology.
The study also pointed out differences between the cohorts. In the ADNI cohort, hypertension’s effects were largely tied to WMH burden, while in the Add-Tau cohort, hypertension was linked to AD pathology, EC thickness, and WMH burden. Notably, hypertensive ADNI participants with Aβ had lower EC tau, contrary to expectations and previous research. These discrepancies could reflect the disease stage differences between the cohorts, recruitment strategies, and vascular risk profiles.
Hypertension and Aβ were found to be common risk factors for WMH and EC tau, potentially mediated by brain hypoperfusion. The study observed a specific decrease in gray matter cerebral blood flow (CBF), particularly in the MTL, which correlated with increased EC tau in Aβ-positive individuals. Interestingly, systolic blood pressure (SBP) emerged as a better predictor of lower CBF than hypertension diagnosis alone, emphasizing the MTL’s vulnerability to blood pressure fluctuations.
The study suggests that decreased CBF could mediate the relationship between Aβ burden and posterior WMH volume, though this association was more pronounced in the Add-Tau cohort. The posterior-to-anterior gradient in Aβ-to-CBF associations could be influenced by underlying cerebral amyloid angiopathy (CAA). CAA has been linked to increased WMH burden in posterior regions and impaired vasodilation in response to physiological stimuli in the occipital lobe.
While the findings support the role of hypertension and Aβ in AD development, the authors caution that causality cannot be definitively established due to the study’s cross-sectional design. Furthermore, the study may have underestimated the effects of hypertension, as participants in both cohorts had relatively low vascular risk and were generally well-educated. The authors also noted limitations such as small sample sizes, differences in disease stages, and the exclusion of key variables such as APOE ε4 allele and sex, which could influence the observed relationships.
In conclusion, the study highlights the multifaceted impact of hypertension on the development of AD dementia, revealing its connections to both vascular and AD pathology. Hypertension contributed to increased AD pathology and WMH burden, particularly in the frontal lobe, both of which were linked to reduced EC thickness and worse memory performance. Reduced cerebral perfusion, influenced by Aβ and hypertension, was associated with WMH burden and increased EC tau. Further longitudinal research is needed to clarify the temporal sequence of these factors and assess whether managing blood pressure could help mitigate AD pathology.