The Hidden Burden of Subclinical Hypothyroidism: When to Treat and When to Watch
Abstract
Background:
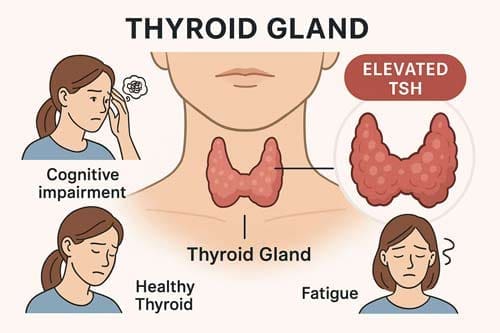
Subclinical hypothyroidism (SCH) is defined by elevated serum thyroid-stimulating hormone (TSH) levels alongside normal free thyroxine (FT4) concentrations. It is a common condition, affecting between 3 and 8 percent of the general population. Despite its prevalence, SCH presents a key clinical challenge because it often lacks clear symptoms, and the decision to initiate treatment remains controversial. The complexity arises from varied clinical presentations and outcomes, making it difficult to establish universal management guidelines.
Methods:
This review synthesizes findings from recent meta-analyses, randomized controlled trials (RCTs), and systematic reviews to provide a comprehensive evaluation of SCH management. The aim is to clarify current evidence surrounding the diagnosis, treatment benefits, and risks of levothyroxine therapy in diverse patient populations.
Results:
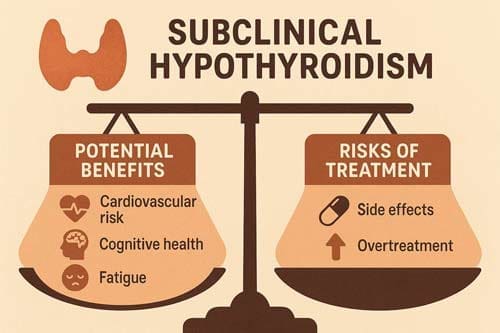
Current research demonstrates considerable heterogeneity in the effects of SCH across different groups. There is evidence linking SCH to increased cardiovascular risk, subtle cognitive impairment, and negative pregnancy outcomes such as miscarriage and preterm birth. However, clinical trials evaluating levothyroxine treatment show inconsistent results. While some subpopulations appear to benefit, especially pregnant women or younger patients with markedly elevated TSH, the majority of studies report minimal improvement in symptoms or quality of life for older adults or those with mild TSH elevations.
Recent clinical guidelines have therefore shifted towards a more conservative approach. Treatment is generally not recommended for most adults over 65 years old when TSH levels are below 10 mIU/L, as the risks of overtreatment and side effects may outweigh potential benefits. In younger individuals, or in cases of higher TSH levels, treatment decisions should be more individualized based on symptom burden and risk factors.
Conclusions:
Managing SCH requires careful, personalized decision-making that takes into account patient age, TSH level, symptom severity, cardiovascular risk profile, pregnancy status, and the presence of thyroid autoantibodies. The use of age-specific reference ranges for TSH can help avoid overdiagnosis and unnecessary treatment in elderly populations, where mild TSH elevations may be normal. Conversely, treatment is most clearly beneficial in younger patients with markedly elevated TSH, symptomatic individuals, or those experiencing pregnancy-related complications or infertility. Overall, the goal is to balance the potential benefits of levothyroxine therapy against the risks and to tailor interventions based on each patient’s clinical context.
Keywords:
Subclinical hypothyroidism, thyroid-stimulating hormone, levothyroxine, cardiovascular risk, cognitive function, pregnancy outcomes, clinical management, treatment guidelines.

Introduction
Subclinical hypothyroidism represents one of the most prevalent yet contentious conditions in modern endocrinology. Subclinical hypothyroidism (sHypo) is defined as normal serum free thyroid hormone levels coexisting with elevated serum thyroid-stimulating hormone (TSH) levels [1] [2], affecting an estimated 3-8% of the general population with higher prevalence in elderly individuals and women. The condition’s “subclinical” designation belies its potential for vital clinical impact, creating a therapeutic paradox that has puzzled clinicians for decades.
The fundamental question underlying SCH management, when to treat and when to watch, has become increasingly complex as our understanding of thyroid physiology and its systemic effects has evolved. The panel concluded that almost all adults with SCH would not benefit from treatment with thyroid hormones. Other factors in the strong recommendation include the burden of lifelong management and uncertainty on potential harms [3], according to recent evidence-based guidelines. However, this blanket recommendation masks substantial heterogeneity in patient populations and clinical scenarios where treatment may be beneficial.
The clinical significance of SCH extends beyond simple laboratory abnormalities. Clinical evidence emerging during the previous decade generally supports the view that SCH is associated with adverse outcomes to an extent that is intermediate between euthyroidism and overt hypothyroidism although evidence that treatment with thyroid hormone replacement is beneficial is lacking [4]. This intermediate position between normal thyroid function and overt disease creates unique challenges for risk stratification and therapeutic decision-making.
Contemporary practice reveals striking inconsistencies in SCH management across different healthcare systems and specialties. Treatment with thyroid hormones is increasing and more than 10-15% of people aged over 80 years are prescribed levothyroxine replacement therapy [5], suggesting potential overtreatment in elderly populations. Conversely, specific patient groups such as women planning pregnancy or those with severe symptoms may be undertreated due to overly restrictive guidelines.
This analytical review examines the current evidence base for SCH management, exploring the complex interplay between biochemical markers, clinical outcomes, and treatment responses across diverse patient populations. By critically evaluating recent research findings and guideline recommendations, we aim to provide a nuanced framework for clinical decision-making that moves beyond simple TSH thresholds toward personalized care approaches.
The stakes of appropriate SCH management are considerable. Overtreatment exposes patients to unnecessary risks including cardiac arrhythmias, bone loss, and healthcare costs, while undertreatment may leave patients vulnerable to cardiovascular complications, cognitive decline, and adverse pregnancy outcomes. Understanding when to intervene and when to observe requires careful consideration of multiple factors including patient age, comorbidities, symptom burden, and specific clinical contexts.
Literature Review and Background
Definition and Diagnostic Considerations
Subclinical hypothyroidism (SCH) should be considered in two categories according to the elevation in serum thyroid-stimulating hormone (TSH) level: mildly increased TSH levels (4.0-10.0 mU/l) and more severely increased TSH value (>10 mU/l) [6]. This stratification has important therapeutic implications, as the risk-benefit ratio of treatment varies notably between these groups.
The diagnostic process for SCH requires careful attention to several factors. An initially raised serum TSH, with FT4 within reference range, should be investigated with a repeat measurement of both serum TSH and FT4, along with thyroid peroxidase antibodies, preferably after a 2- to 3-month interval [7]. This approach helps distinguish persistent SCH from transient elevations that may occur due to illness, medications, or physiological stress.
Epidemiological Considerations and Age-Related Changes
The prevalence of SCH increases with age, creating important diagnostic challenges. The reference range for TSH also rises with age, as the population distribution of TSH concentration progressively rises with age [8]. This age-related shift has prompted calls for age-specific reference ranges to prevent overdiagnosis in elderly populations.
The overdiagnosis and overtreatment of SCH in elderly patients have become concerns as TSH levels naturally increase with age. Studies have shown that many elderly patients with SCH can recover without treatment, and the administration of levothyroxine (L-T4) does not improve their prognosis [9]. These findings challenge the universal application of standard TSH reference ranges across all age groups.
Pathophysiological Mechanisms
During the differential diagnosis, it is important to remember that a considerable proportion of sHypo cases are transient and reversible in nature; the focus is better placed on persistent or progressive forms, which mainly result from chronic autoimmune thyroiditis [10]. Understanding the underlying etiology can help predict disease progression and guide treatment decisions.
The progression from SCH to overt hypothyroidism varies considerably based on several factors. The annual rate of progression to overt hypothyroidism is 4.3% in patients of all ages with both high concentrations of serum TSH and positive thyroid peroxidase (TPO) antibodies, 2.8% in patients of all ages with normal concentrations of serum TSH and positive TPO antibodies [11]. These data highlight the importance of antibody testing in risk stratification.
Cardiovascular Outcomes and Risk Assessment
Evidence for Cardiovascular Associations
The relationship between SCH and cardiovascular outcomes represents one of the most extensively studied aspects of this condition, yet controversies persist regarding both the magnitude of risk and the benefits of treatment. Subclinical hypothyroidism is likely associated with an increased risk of CHD mortality, and subclinical hyperthyroidism is likely associated with increased risk of CHD, CHD mortality, and total mortality [12], according to systematic reviews of prospective cohort studies.
However, the cardiovascular risk appears to be age-dependent. Subgroup analysis indicated a higher estimation risk in CHD, cardiovascular mortality, and CHD mortality among participants < 65 years [13]. This age stratification suggests that the cardiovascular implications of SCH may be more pronounced in younger individuals, potentially informing treatment decisions.
Cardiac Surgery Outcomes
Recent evidence from surgical populations provides additional insights into the clinical significance of SCH. Patients with SCH have higher operative mortality, prolonged hospital LOS, and increased renal complications after cardiac surgery. Achieving and maintaining a euthyroid state prior to and after cardiac surgery procedures might improve outcomes in these patients [14]. These findings suggest that surgical patients may represent a subgroup where pre-operative thyroid optimization could be beneficial.
Heart Failure Interactions
The relationship between SCH and heart failure outcomes has emerged as a particularly important area of investigation. Subclinical hypothyroidism was an independent predictor (hazard ratio: 2.31; 95% confidence interval: 1.44 to 3.67; P < 0.001), whereas low-T3 syndrome and subclinical hyperthyroidism were not. Subclinical hypothyroidism on admission was an independent predictor of adverse cardiovascular outcomes in ADHF patients, suggesting a possible interaction between thyroid dysfunction and the pathophysiology of ADHF [15].
Metabolic Syndrome and Cardiovascular Risk Factors
The aim of this cross-sectional study was to evaluate the cardiovascular risk in patients with subclinical hypothyroidism (SH) and metabolic syndrome (MetS) components. The study included 60 patients with SH and a control group of 60 healthy volunteers, gender and age matched, with normal thyroid-stimulating hormone (TSH) and free thyroxin (FT4) concentration [16]. These studies reveal complex interactions between SCH and other cardiovascular risk factors that may modify treatment recommendations.
Treatment Controversies and Clinical Guidelines
Recent Guideline Recommendations
The publication of major clinical practice guidelines has greatly influenced SCH management approaches. The guideline panel issues a strong recommendation against thyroid hormones in adults with SCH (elevated TSH levels and normal free T4 levels). It does not apply to women who are trying to become pregnant or patients with TSH >20 mIU/L. It may not apply to patients with severe symptoms or young adults (such as those ≤30 years old) [17].
This strong recommendation represents a major shift from previous guidelines that were more permissive regarding treatment. However, the exceptions noted in the guidelines highlight the complexity of individual patient scenarios and the need for nuanced decision-making.
European Thyroid Association Perspective
The European Thyroid Association guidelines provide additional context for treatment decisions. Even in the absence of symptoms, replacement therapy with L-thyroxine is recommended for younger patients (<65-70 years) with serum TSH >10 mU/l. In younger SCH patients (serum TSH <10 mU/l) with symptoms suggestive of hypothyroidism, a trial of L-thyroxine replacement therapy should be considered [18].
These recommendations acknowledge the importance of age and symptom burden in treatment decisions, while maintaining a higher threshold for elderly patients. The oldest old subjects (>80-85 years) with elevated serum TSH ≤10 mU/l should be carefully followed with a wait-and-see strategy, generally avoiding hormonal treatment [19].
Age-Specific Considerations
The approach to elderly patients with SCH has evolved notably based on emerging evidence. These data suggest that treatment with levothyroxine should be considered for individuals aged 65 years or older with subclinical hypothyroidism when thyroid-stimulating hormone concentration is persistently 7 mIU/L or higher and to not initiate treatment with thyroid-stimulating hormone concentrations of less than 7 mIU/L. Levothyroxine doses should be personalised according to age, comorbidities, and life expectancy [20].

Quality of Life and Patient-Reported Outcomes
Systematic Reviews of Quality of Life Data
The impact of levothyroxine treatment on quality of life in SCH patients has been rigorously evaluated through multiple systematic reviews. Among nonpregnant adults with subclinical hypothyroidism, the use of thyroid hormone therapy was not associated with improvements in general quality of life or thyroid-related symptoms. These findings do not support the routine use of thyroid hormone therapy in adults with subclinical [21] hypothyroidism.
This finding represents a critical challenge to the assumption that SCH treatment consistently improves patient wellbeing. The lack of demonstrable quality of life benefits in most patients raises important questions about the value of treatment beyond laboratory normalization.
Age-Specific Quality of Life Responses
Interestingly, the quality of life response to treatment may vary by age group. We found lower QoL in both young and old patients with subclinical hypothyroidism compared to age-matched healthy individuals. Higher scores on follow-up were found in all patients irrespective of age, indicating better QoL on LT4 therapy. Analysis of the ThyPRO questionnaire showed that old patients experienced less Emotional Susceptibility, Tiredness, and Impaired Day Life on LT4, while young patients reported less Cognitive Complaints, Emotional Susceptibility, and Impaired Day Life compared to baseline assessment [22] [23].
Patient Perspectives and Treatment Satisfaction
Recent surveys of hypothyroid patients reveal concerning gaps between laboratory normalization and symptom resolution. There was a large-sized impairment of QoL (Cohen’s d = 1.04, +93 % ThyPRO score) in hypothyroid patients on thyroid replacement therapy (n = 1195) as compared to controls (n = 236). Daily functioning was reduced i.e., general health (-38 %), problems with vigorous- (+64 %) and moderate activities (+77 %). Almost 80 % of patients reported having complaints despite thyroid medication and in-range thyroid blood values, with 75 % expressing a desire for improved treatment options for hypothyroidism [24].
These data suggest that current treatment approaches may be inadequate for a considerable proportion of patients, highlighting the need for improved understanding of optimal thyroid hormone replacement strategies.
Pregnancy and Reproductive Health
Pregnancy Outcomes in Subclinical Hypothyroidism
The management of SCH during pregnancy represents one of the most compelling arguments for treatment in specific clinical contexts. Subclinical hypothyroidism, defined by elevated thyrotropin (TSH) and normal free thyroxine levels, is associated with adverse pregnancy outcomes, including preterm birth, pre-eclampsia, and small for gestational age [25].
However, the evidence for treatment benefits remains mixed. Treatment for subclinical hypothyroidism or hypothyroxinemia beginning between 8 and 20 weeks of gestation did not result in better cognitive outcomes in children through 5 years of age than no treatment for those conditions [26] [27], according to a large randomized controlled trial.
Fertility and Assisted Reproduction
There is controversy regarding whether to treat subtle abnormalities of thyroid function in infertile female patients. This guideline document reviews the risks and benefits of treating subclinical hypothyroidism in female patients with a history of infertility and miscarriage, as well as obstetric and neonatal outcomes in this population [28].
Meta-Analytic Evidence for Pregnancy Outcomes
Recent systematic reviews provide nuanced insights into treatment benefits during pregnancy. Levothyroxine replacement therapy for subclinical hypothyroidism during pregnancy may decrease pregnancy loss when early prescribed. Patients treated with levothyroxine had lower risk of pregnancy loss (risk ratio 0.69; 95% confidence interval 0.52-0.91; p < 0.01; 6 studies). However, there was no association between levothyroxine and live birth (risk ratio 1.01; 95% confidence interval 0.99-1.03; p = 0.29; 8 studies) [29] [30].
Evidence for Preconception Treatment
There is strong evidence from systematic reviews and meta-analyses that uncontrolled SCH is associated with an increased risk of adverse pregnancy outcomes, including miscarriage, preeclampsia, and gestational diabetes. The evidence base also suggests that treatment with levothyroxine (LT4), optimized to control thyrotropin (TSH) to within its pregnancy-specific reference ranges reduces these risks [31].
Cognitive Function and Neuropsychiatric Outcomes
Age-Related Cognitive Effects
The relationship between SCH and cognitive function appears to be age-dependent, with important implications for treatment decisions. A substantial risk of cognitive alteration was observed only in sHT individuals younger than age 75 years: composite endpoint odds ratio (OR) 1.56 (95% confidence interval [CI] 1.07-2.27, P = .02, I(2) = 82.5%), risk of dementia OR 1.81 (95% CI 1.43-2.28, P < .01, I(2) = 35%). This meta-analysis demonstrates a relationship between sHT and cognitive impairment only in individuals younger than 75 years of age and those with higher TSH concentrations [32].
Clinical Significance in Elderly Populations
The lack of utilization of age-related serum TSH reference ranges and consequent potential misdiagnosis of sHT in older people may account for this [33]. This observation reinforces the importance of age-appropriate diagnostic criteria and treatment thresholds.
Evidence for Cognitive Benefits of Treatment
Two meta-analyses did not show an association between subclinical hypothyroidism and cognitive impairment in participants older than 60 years or those older than 75 years. A third meta-analysis including seven prospective cohorts, conducted in patients with a mean age of 65 years or older, did not show any association between subclinical hypothyroidism and dementia or decline in cognition [34].
Bone Health and Fracture Risk
Fracture Risk in Subclinical Thyroid Dysfunction
The relationship between subclinical thyroid dysfunction and bone health reveals important distinctions between hypo- and hyperthyroidism. Subclinical hyperthyroidism could induce additional risk on fractures at any, hip, spine, and non-spine, whereas subclinical hypothyroidism did not have any impact on fractures [35] [36].
Meta-Analytic Evidence
Large-scale meta-analyses provide reassuring evidence regarding bone safety in SCH. In an unadjusted model, the relative risk (RR) of subclinical hypothyroidism for fracture was 1.30 (CI 1.08-1.56). Risk estimates were lower in a multivariable-adjusted model (RR = 1.20, CI 0.70-2.04) and when higher quality studies (RR = 0.95, CI 0.58-1.57) were analyzed [37].
Clinical Implications for Bone Health
Subclinical hypothyroidism, on the other hand, is not associated with osteoporosis or fragility fractures, and subclinical hyperthyroidism treatment with radioiodine could improve bone health. These findings suggest that SCH itself does not pose skeletal risks, alleviating concerns about withholding treatment for bone health reasons.
Gender and Age Considerations
Our data suggest no association between subclinical hypothyroidism or subclinical hyperthyroidism and hip fracture risk or BMD in older men and women. Additional data are needed to improve the precision of estimates for subclinical hyperthyroidism and in men [38].
Clinical Decision-Making Framework
Risk Stratification Approaches
The development of individualized treatment approaches requires careful consideration of multiple patient factors. Current evidence suggests that individuals with TSH levels greater than 10 mIU/L who test positive for antithyroid antibodies or are symptomatic may benefit from levothyroxine treatment to reduce the risk of progression to overt hypothyroidism, decrease the risk of adverse cardiovascular events, and improve their quality of life [39].
Age-Specific Treatment Thresholds
Based on the overall evidence, treatment of SCH is indicated in younger persons with a TSH level >4.0 mIU/L. In older subjects, treatment should be individualised and based on the presence of symptoms, the level of TSH, and initiated at TSH levels ≥10 mIU/L and at low doses to avoid adverse [40] effects.
Monitoring and Follow-up Strategies
For patients who are not treated, careful monitoring remains essential. Once patients with SCH are commenced on L-thyroxine treatment, then serum TSH should be monitored at least annually thereafter [41]. Similar monitoring intervals may be appropriate for untreated patients to detect progression to overt hypothyroidism.
Treatment Goals and Targets
When treatment is initiated, appropriate target ranges must be established. The aim for most adults should be to reach a stable serum TSH in the lower half of the reference range (0.4-2.5 mU/l) [42]. However, elderly patients may benefit from higher target TSH levels to minimize overtreatment risks.
Special Populations and Clinical Scenarios
Subclinical Hypothyroidism in Infertility
The management of SCH in women with infertility requires special consideration. This study evaluated the frequency of these factors among adult (non-pregnant) women with SCH whose TSH levels are ≤10 mIU/L. The presence of the conditions that should be considered for the treatment of SCH according to ATA and AACE was evaluated in 252 women who were diagnosed with SCH and had TSH levels ≤10 mIU/L [43].
The high frequency of treatment-relevant factors in this population suggests that many women with infertility and mild SCH may warrant treatment consideration even with TSH levels below traditional thresholds.
Perioperative Considerations
Patients with SCH have higher operative mortality, prolonged hospital LOS, and increased renal complications after cardiac surgery. Achieving and maintaining a euthyroid state prior to and after cardiac surgery procedures might improve outcomes in these patients [44].
Patients with Cardiovascular Disease
The presence of established cardiovascular disease may modify treatment recommendations for SCH patients. SCH negatively impacted clinical outcomes following PCIs. Therefore, patients with SCH should be carefully observed after undergoing a PCI [45].
Current Controversies and Unresolved Questions
Treatment Duration and Reversibility
For such patients who have been started on L-thyroxine for symptoms attributed to SCH, response to treatment should be reviewed 3 or 4 months after a serum TSH within reference range is reached [46]. This approach allows for assessment of treatment benefit and potential discontinuation in non-responders.
Optimal Thyroid Hormone Preparations
Levothyroxine substitution improves, but does not always normalize, QOL, especially for individuals with mild hypothyroidism. However, neither studies combining levothyroxine and liothyronine (the synthetic form of tri-iodothyronine) nor the use of desiccated thyroid extract have shown robust improvements in patient satisfaction [47].
Biomarker Development
Despite compelling evidence documenting the health impacts of sHypo, the effects of levothyroxine treatment (LT4-Tx) in patients with sHypo remains controversial, especially in patients with grade 1 sHypo and older adults. Existing evidence suggests that it is reasonable to refrain from immediate LT4-Tx in most patients if they are closely monitored, except in women who are pregnant or in progressive cases [48].
Future Research Directions
Personalized Medicine Approaches
Future research is needed to further characterize the risks and benefits of LT4-Tx in different patient cohorts [49]. The development of more precise risk stratification tools could improve treatment selection and outcomes.
Age-Specific Reference Ranges
Therefore, It is necessary to establish age-specific reference ranges for TSH in elderly individuals to aid in clinical decision-making and prevent overdiagnosis [50] [51]. Implementation of age-adjusted reference ranges could impact SCH prevalence estimates and treatment patterns.
Biomarker Discovery
Appropriately designed and powered randomised controlled trials are required to confirm risk/benefit of treatment of subclinical hypothyroidism in older people [52]. Such trials should incorporate novel biomarkers and patient-reported outcome measures to better understand treatment effects.
Clinical Practice Implications
Shared Decision-Making
The complexity of SCH management necessitates robust shared decision-making between clinicians and patients. Almost 80 % of patients reported having complaints despite thyroid medication and in-range thyroid blood values, with 75 % expressing a desire for improved treatment options for hypothyroidism [53]. This patient dissatisfaction highlights the importance of realistic expectations and ongoing communication.
Healthcare System Considerations
There is growing evidence that treatment of subclinical hypothyroidism may not be beneficial, particularly in an older person. These findings are relevant at a time when treatment with thyroid hormones is increasing and more than 10-15% of people aged over 80 years are prescribed levothyroxine replacement therapy [54].
Cost-Effectiveness Analysis
The economic implications of SCH management decisions require careful consideration, particularly given the high prevalence of the condition and potential for overtreatment. Long-term cost-effectiveness studies incorporating quality-adjusted life years could inform healthcare policy decisions.
Limitations and Methodological Considerations
Heterogeneity in Study Populations
Variability in study populations presents a major challenge to evidence synthesis and the development of generalizable recommendations. Differences in geographic location, ethnicity, and socioeconomic status can affect both the prevalence of subclinical hypothyroidism (SCH) and the response to treatment, limiting the applicability of findings across diverse groups.
Outcome Measurement Variability
Inconsistent outcome measures across studies hinder meaningful comparisons and reduce the reliability of conclusions. The adoption of standardized, consensus-based core outcome sets would enhance the comparability and quality of future SCH research.
Selection Bias in Treatment Studies
Observational studies on SCH treatment are often affected by selection bias. Patients who receive treatment may differ in important ways from those who are not treated, which can distort estimates of treatment effectiveness and lead to misleading conclusions. More rigorous study designs are needed to address this limitation.
Conclusion
The management of subclinical hypothyroidism represents a paradigmatic example of how evidence-based medicine must evolve to embrace personalized care approaches. The accumulating evidence suggests that the traditional binary approach of “treat or don’t treat” is inadequate for addressing the complexity of SCH across diverse patient populations.
The current evidence supports a more nuanced approach that considers multiple patient factors including age, TSH level, symptom burden, comorbidities, and specific clinical contexts such as pregnancy or planned conception. For most elderly patients with mild TSH elevations, a watchful waiting approach appears appropriate and may prevent unnecessary medicalization of age-related physiological changes.
However, specific patient subgroups may derive benefit from treatment, including younger patients with higher TSH levels, women planning pregnancy or experiencing infertility, and patients with cardiovascular risk factors or symptomatic disease. The challenge for clinicians lies in accurately identifying these patients and implementing individualized treatment plans that optimize benefits while minimizing risks.
Future research efforts should focus on developing more precise risk stratification tools, validating age-specific reference ranges, and conducting well-designed randomized controlled trials in specific patient subgroups where treatment benefits may be most pronounced. The ultimate goal should be moving beyond simple TSH thresholds toward a more sophisticated understanding of which patients are most likely to benefit from intervention.
The hidden burden of subclinical hypothyroidism extends beyond laboratory abnormalities to encompass the complexity of clinical decision-making in an era of precision medicine. By embracing this complexity rather than seeking overly simplistic solutions, we can better serve patients and optimize outcomes across the spectrum of thyroid dysfunction.
Healthcare systems must also grapple with the implications of SCH management decisions, balancing the costs and potential harms of treatment against the benefits for selected patients. The development of clinical decision support tools and implementation of shared decision-making processes will be essential for translating research evidence into improved patient care.
As our understanding of subclinical hypothyroidism continues to evolve, the fundamental principle of individualized patient care must remain central to all treatment decisions. The journey from laboratory abnormality to clinical significance requires careful navigation of complex evidence, patient preferences, and clinical judgment—a challenge that epitomizes the art and science of modern medicine.
References
- Bekkering, G. E., Agoritsas, T., Lytvyn, L., Heen, A. F., Feller, M., Moutzouri, E., Abdulazeem, H., Aertgeerts, B., Beecher, D., Brito, J. P., Farhoumand, P. D., Singh, K., Snel, M., Until, C., Vermandere, M., Kuijpers, T., Vandvik, P. O., & Guyatt, G. H. (2019). Thyroid hormones treatment for subclinical hypothyroidism: a clinical practice guideline. BMJ, 365, l2006. https://doi.org/10.1136/bmj.l2006
- Carlé, A., Pedersen, I. B., Knudsen, N., Perrild, H., Ovesen, L., Rasmussen, L. B., & Laurberg, P. (2013). Epidemiology of subtypes of hypothyroidism in Denmark. European Journal of Endocrinology, 169(6), 755-762. https://doi.org/10.1530/EJE-13-0155
- Cooper, D. S., & Biondi, B. (2012). Subclinical thyroid disease. The Lancet, 379(9821), 1142-1154. https://doi.org/10.1016/S0140-6736(11)60276-6
- Garber, J. R., Cobin, R. H., Gharib, H., Hennessey, J. V., Klein, I., Mechanick, J. I., Pessah-Pollack, R., Singer, P. A., Woeber, K. A., & American Association of Clinical Endocrinologists and American Thyroid Association Taskforce on Hypothyroidism in Adults. (2012). Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid, 22(12), 1200-1235. https://doi.org/10.1089/thy.2012.0205
- Pearce, S. H., Brabant, G., Duntas, L. H., Monzani, F., Peeters, R. P., Razvi, S., & Wemeau, J. L. (2013). 2013 ETA guideline: management of subclinical hypothyroidism. European Thyroid Journal, 2(4), 215-228. https://doi.org/10.1159/000356507
- Razvi, S., Jabbar, A., Pingitore, A., Danzi, S., Biondi, B., Klein, I., Peeters, R., Zaman, A., & Iervasi, G. (2018). Thyroid hormones and cardiovascular function and diseases. Journal of the American College of Cardiology, 71(16), 1781-1796. https://doi.org/10.1016/j.jacc.2018.02.045
- Rodondi, N., den Elzen, W. P., Bauer, D. C., Cappola, A. R., Razvi, S., Walsh, J. P., Asvold, B. O., Iervasi, G., Imaizumi, M., Collet, T. H., Bremner, A., Maisonneuve, P., Sgarbi, J. A., Khaw, K. T., Vanderpump, M. P., Newman, A. B., Cornuz, J., Franklyn, J. A., Westendorp, R. G., Vittinghoff, E., & Gussekloo, J. (2010). Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA, 304(12), 1365-1374. https://doi.org/10.1001/jama.2010.1361
- Surks, M. I., Ortiz, E., Daniels, G. H., Sawin, C. T., Col, N. F., Cobin, R. H., Franklyn, J. A., Hershman, J. M., Burman, K. D., Denke, M. A., Gorman, C., Cooper, R. S., & Weissman, N. J. (2004). Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA, 291(2), 228-238. https://doi.org/10.1001/jama.291.2.228
- Stott, D. J., Rodondi, N., Kearney, P. M., Ford, I., Westendorp, R. G., Mooijaart, S. P., Sattar, N., Aubert, C. E., Aujesky, D., Bauer, D. C., Baumgartner, C., Blum, M. R., Browne, J. P., Byrne, S., Collet, T. H., Dekkers, O. M., den Elzen, W. P., Du Puy, R. S., Ellis, G., Feller, M., Floriani, C., Hendry, K., Hurley, C., Jukema, J. W., Kean, S., Kelly, M., Krebs, D., Langhorne, P., McCarthy, G., McCarthy, V., McConnachie, A., McDade, M., Messow, M., O’Flynn, A., O’Riordan, D., Poortvliet, R. K., Quinn, T. J., Russell, A., Sinnott, C., Smit, J. W., Van Dorland, H. A., Walsh, K. A., Walsh, E. K., Watt, T., Wilson, R., & Gussekloo, J. (2017). Thyroid hormone therapy for older adults with subclinical hypothyroidism. New England Journal of Medicine, 376(26), 2534-2544. https://doi.org/10.1056/NEJMoa1603825
- Razvi, S., Weaver, J. U., Butler, T. J., & Pearce, S. H. (2012). Levothyroxine treatment of subclinical hypothyroidism, fatal and nonfatal cardiovascular events, and mortality. Archives of Internal Medicine, 172(10), 811-817. https://doi.org/10.1001/archinternmed.2012.1159
References
[1] Subclinical Hypothyroidism: Prevalence, Health Impact, and Treatment Landscape – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34139799/
[2] Subclinical Hypothyroidism: Prevalence, Health Impact, and Treatment Landscape – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34139799/
[3] Thyroid hormones treatment for subclinical hypothyroidism: a clinical practice guideline – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31088853/
[4] Subclinical hypothyroidism, outcomes and management guidelines: a narrative review and update of recent literature – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36632720/
[5] Age-specific serum thyrotropin reference range for the diagnosis of subclinical hypothyroidism and its association with lipid profiles in the elderly population – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36463291/
[6] 2013 ETA Guideline: Management of Subclinical Hypothyroidism – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/24783053/
[7] 2013 ETA Guideline: Management of Subclinical Hypothyroidism – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/24783053/
[8] Age-specific serum thyrotropin reference range for the diagnosis of subclinical hypothyroidism and its association with lipid profiles in the elderly population – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36463291/
[9] Thyroid disorders in elderly: A comprehensive review – ScienceDirect – www.sciencedirect.com https://www.sciencedirect.com/science/article/abs/pii/S0011502921000997
[10] Subclinical Hypothyroidism: Prevalence, Health Impact, and Treatment Landscape – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/34139799/
[11] Hypothyroidism in the older population – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/30774717/
[12] Prognostic Role of Hypothyroidism in Heart Failure: A Meta-Analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/26222845/
[13] Prognostic Role of Hypothyroidism in Heart Failure: A Meta-Analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/26222845/
[14] Subclinical hypothyroidism and cardiovascular risk: how to end the controversy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/23633199/
[15] Treatment of Subclinical Hypothyroidism or Hypothyroxinemia in Pregnancy – PubMed – pubmed.ncbi.nlm.nih.govhttps://pubmed.ncbi.nlm.nih.gov/28249134/
[16] Cardiovascular risk in chronic autoimmune thyroiditis and subclinical hypothyroidism patients. A cluster analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/28038798/
[17] Thyroid hormones treatment for subclinical hypothyroidism: a clinical practice guideline – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31088853/
[18] 2013 ETA Guideline: Management of Subclinical Hypothyroidism – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/24783053/
[19] 2013 ETA Guideline: Management of Subclinical Hypothyroidism – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/24783053/
[20] Hypothyroidism in the older population – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/30774717/
[21] Impact of subclinical hypothyroidism on clinical outcomes following percutaneous coronary intervention – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/29306458/
[22] Subclinical thyroid dysfunction and hip fracture and bone mineral density in older adults: the cardiovascular health study – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/24878045/
[23] Subclinical thyroid dysfunction and hip fracture and bone mineral density in older adults: the cardiovascular health study – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/24878045/
[24] Thyroid Related Quality of Life in Elderly with Subclinical Hypothyroidism and Improvement on Levothyroxine is Distinct from that in Young Patients (TSAGE) – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31505703/
[25] Treatment of thyroid disorders before conception and in early pregnancy: a systematic review – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/22431565/
[26] Optimizing levothyroxine treatment for subclinical hypothyroidism during pregnancy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/37897184/
[27] Optimizing levothyroxine treatment for subclinical hypothyroidism during pregnancy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/37897184/
[28] Subclinical hypothyroidism in the infertile female population: a guideline – ScienceDirect – www.sciencedirect.com https://www.sciencedirect.com/science/article/pii/S001502822302109X
[29] Reference Ranges for Thyroid-Stimulating Hormone and Free Thyroxine in Older Men: Results From the Health In Men Study – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/27440910/
[30] Reference Ranges for Thyroid-Stimulating Hormone and Free Thyroxine in Older Men: Results From the Health In Men Study – PubMed – pubmed.ncbi.nlm.nih.govhttps://pubmed.ncbi.nlm.nih.gov/27440910/
[31] Effects of maternal subclinical hypothyroidism on obstetrical outcomes during early pregnancy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/21642766/
[32] Thyroid Function Changes in the Elderly and Their Relationship to Cardiovascular Health: A Mini-Review – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/30032140/
[33] Thyroid Function Changes in the Elderly and Their Relationship to Cardiovascular Health: A Mini-Review – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/30032140/
[34] Hypothyroidism in the older population – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/30774717/
[35] Subclinical thyrotoxicosis and bone – ScienceDirect – www.sciencedirect.com https://www.sciencedirect.com/science/article/abs/pii/S2451965017300285
[36] Subclinical thyrotoxicosis and bone – ScienceDirect – www.sciencedirect.com https://www.sciencedirect.com/science/article/abs/pii/S2451965017300285
[37] The Influence of Thyroid Pathology on Osteoporosis and Fracture Risk: A Review – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32156092/
[38] Association Between Subclinical Thyroid Dysfunction and Fracture Risk – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36346629/
[39] Association of Thyroid Hormone Therapy With Quality of Life and Thyroid-Related Symptoms in Patients With Subclinical Hypothyroidism: A Systematic Review and Meta-analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/30285179/
[40] Subclinical thyroid dysfunction and fracture risk: a meta-analysis – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/26010634/
[41] 2013 ETA Guideline: Management of Subclinical Hypothyroidism – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/24783053/
[42] 2013 ETA Guideline: Management of Subclinical Hypothyroidism – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/24783053/
[43] How selective are the new guidelines for treatment of subclinical hypothyroidism for patients with thyrotropin levels at or below 10 mIU/L? – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/23627903/
[44] Subclinical hypothyroidism and cardiovascular risk: how to end the controversy – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/23633199/
[45] Is Hypothyroidism Associated With Outcomes in Fracture Patients? Data From a Trauma Registry – ScienceDirect – www.sciencedirect.com https://www.sciencedirect.com/science/article/abs/pii/S0022480421005047
[46] 2013 ETA Guideline: Management of Subclinical Hypothyroidism – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/24783053/
[47] The current debate over treatment of subclinical hypothyroidism to prevent cardiovascular complications – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/32159256/
[48] Subclinical hypothyroidism is an independent predictor of adverse cardiovascular outcomes in patients with acute decompensated heart failure – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/27818781/
[49] Subclinical hypothyroidism is an independent predictor of adverse cardiovascular outcomes in patients with acute decompensated heart failure – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/27818781/
[50] Thyroid disorders in elderly: A comprehensive review – ScienceDirect – www.sciencedirect.com https://www.sciencedirect.com/science/article/abs/pii/S0011502921000997
[51] Thyroid disorders in elderly: A comprehensive review – ScienceDirect – www.sciencedirect.com https://www.sciencedirect.com/science/article/abs/pii/S0011502921000997
[52] Age-specific serum thyrotropin reference range for the diagnosis of subclinical hypothyroidism and its association with lipid profiles in the elderly population – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36463291/
[53] Thyroid Related Quality of Life in Elderly with Subclinical Hypothyroidism and Improvement on Levothyroxine is Distinct from that in Young Patients (TSAGE) – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/31505703/
[54] Age-specific serum thyrotropin reference range for the diagnosis of subclinical hypothyroidism and its association with lipid profiles in the elderly population – PubMed – pubmed.ncbi.nlm.nih.gov https://pubmed.ncbi.nlm.nih.gov/36463291/

