Hidden First Signs of Leukemia That Doctors Often Miss in Primary Care
Please like and subscribe if you enjoyed this video 🙂
Introduction
Leukemia accounts for approximately 3.2% of all new cancer cases in the U.S., yet its early signs often resemble common, non-specific illnesses—making early diagnosis particularly challenging. Acute lymphocytic leukemia (ALL) primarily affects children, while acute myelogenous leukemia (AML) is the most common form in adults. Both present with unique clinical patterns and survival rates, but often begin with vague symptoms.
The early symptoms of leukemia can remain deceptively subtle, with manifestations such as fatigue, fever, and easy bruising often being attributed to more benign conditions. In fact, many cases of leukemia are discovered incidentally through routine blood tests, as chronic forms may remain asymptomatic for years. This challenge is even greater in older adults—most commonly diagnosed at age 65 or older—where comorbidities can obscure the clinical picture.
This comprehensive analysis examines the silent yet vital early indicators of leukemia that practitioners should carefully evaluate during primary care assessments, including:
- Hematological changes often attributed to other conditions
- Systemic symptoms frequently dismissed as routine ailments
- Physical manifestations commonly overlooked during examinations
- Common diagnostic pitfalls in primary care settings

Subtle Hematological Changes: First Signs of Leukemia
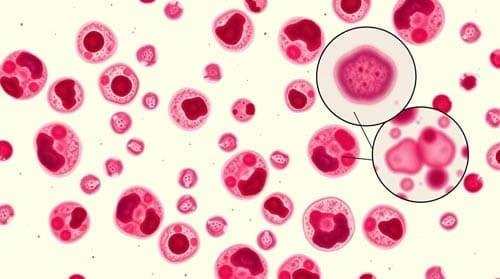
The small changes in complete blood count (CBC) often constitute the earliest detectable signs of leukemia, frequently preceding obvious clinical symptoms by months or even years. However, these early hematological shifts can be remarkably deceptive, leading to delayed diagnosis as primary care physicians attribute them to more common conditions.
Blood count abnormalities often attributed to other conditions
Early signs of leukemia often appear as mild and persistent abnormalities in the complete blood count (CBC), which may go unnoticed or be attributed to more benign causes. Common misinterpretations include:
- Anemia misdiagnosed as iron deficiency or chronic disease
- Thrombocytopenia mistaken for medication effects
- Leukopenia dismissed as a viral response
Importantly, copper deficiency can mimic myelodysplastic syndromes, and autoimmune cytopenias like immune thrombocytopenia or hemolytic anemia may actually be secondary to undiagnosed leukemia—especially in 4–10% of chronic lymphocytic leukemia (CLL) cases.
Persistent mild cytopenias as warning signals
Mild yet persistent reductions in blood cell counts represent important warning signals that warrant closer scrutiny. These include:
- Pancytopenia (reduction in all three cell lines)
- Isolated neutropenia without clear infectious cause
- Mild thrombocytopenia that persists beyond expected resolution timeframes
- Unexplained anemia resistant to iron supplementation
Alarmingly, a study found that almost one-third of 189 children referred with persistent cytopenias had an underlying inherited disorder, with 79.7% of those having a germline predisposition to leukemia. Consequently, physicians should consider genetic evaluation for persistent unexplained cytopenias.
The significance of trending CBC values over time
Monitoring CBC trends is far more informative than relying on isolated results. Gradual declines in blood counts—still within normal limits—can point to early leukemia when viewed over time. Subtle morphological changes, such as vacuolated myeloid precursors or ring sideroblasts in differential counts, may also signal early disease.
Rather than isolated abnormal values, the pattern and progression of changes offer more diagnostic value. Therefore, primary care physicians should establish baseline hematologic parameters for patients and monitor trends, especially when accompanied by subtle systemic symptoms like unexplained fatigue or recurrent infections that persist beyond expected timeframes.

Systemic Symptoms Frequently Misattributed
Beyond laboratory values, systemic manifestations often represent early leukemia warning signs that primary care physicians frequently misinterpret. Systemic symptoms appear because of both the direct effects of leukemic cells and the body’s response to malignancy, yet they commonly receive alternative explanations.
Fatigue dismissed as stress or depression
Fatigue is one of the most common early symptoms of leukemia, affecting up to 100% of patients. Unlike typical tiredness, leukemic fatigue is profound, persistent, and unrelieved by rest. It often disrupts daily function and quality of life. However, it is frequently misattributed to:
- Psychological stress or depression
- Poor sleep habits
- Work-related burnout
Nevertheless, leukemic fatigue typically doesn’t improve with rest and may intensify despite adequate sleep. This exhaustion stems predominantly from anemia resulting from bone marrow infiltration and impaired red blood cell production.
Recurrent infections mistaken for immune deficiency
Approximately 20% of patients experience frequent or severe infections before their leukemia diagnosis. These infections are a result of dysfunctional or insufficient white blood cell production, which compromises immune defense. Clinical features that should raise suspicion include:
- Infections that are unusually severe or long-lasting, such as persistent respiratory or urinary tract infections
- Poor response to standard antimicrobial therapy, requiring prolonged or repeated courses of antibiotics
- Frequent recurrence, sometimes involving the same anatomic sites or pathogens
These patterns are often misinterpreted as:
- Recurrent viral syndromes (e.g., influenza, Epstein-Barr virus)
- Primary or secondary immunodeficiency
- Stress-related immune suppression
Recognizing an abnormal infection pattern in a previously healthy patient should prompt further investigation, including a complete blood count and evaluation of immune cell counts.
Unexplained weight loss attributed to lifestyle changes
Rapid and unintentional weight loss—without dietary or activity changes—can be a red flag for an underlying malignancy. In leukemia, this symptom may reflect the metabolic demands of the disease or systemic inflammation. Key clinical considerations include:
- Significant weight loss (>5% of body weight over 6–12 months) in the absence of caloric restriction
- Stable or increased appetite, ruling out anorexia or dietary modification as a cause
- Accompanying systemic symptoms, such as fatigue or fever
Despite these signs, such weight loss is often attributed to:
- Lifestyle changes or increased physical activity
- Work-related stress or anxiety
- Gastrointestinal conditions or minor metabolic disturbances
Weight loss should never be dismissed, especially when accompanied by other constitutional symptoms.
Night sweats confused with menopause or environmental factors
About one-third of leukemia patients report experiencing drenching night sweats prior to diagnosis. These are often due to cytokine release and the body’s inflammatory response to malignancy. Features that distinguish them from benign causes include:
- Sweats that soak through clothing and bed linens
- Occurrence in cool environments, not related to room temperature or bedding
- Absence of fever or infection, though low-grade fevers may coexist
Physicians may mistakenly attribute these symptoms to:
- Menopausal hot flashes
- Environmental heat or bedding materials
- Anxiety-related autonomic symptoms
When seen alongside fatigue, weight loss, or lymphadenopathy, night sweats should prompt evaluation for hematologic malignancies.
Physical Manifestations Overlooked in Routine Examinations
Physical examination findings play a vital role in identifying leukemia, yet certain manifestations often remain unnoticed or misinterpreted during routine assessments. Primary care providers must develop a heightened awareness of these subtle physical signs to facilitate earlier diagnosis.
Subtle lymphadenopathy: when to be concerned
Lymphadenopathy is a common clinical sign in leukemia, particularly in lymphoid subtypes. It is often overlooked during routine exams, especially when nodes are small, non-tender, or located in less accessible regions. Concerning features include:
- Firm, non-tender lymph nodes that do not resolve over time
- Nodes in atypical locations, such as supraclavicular, axillary, or posterior cervical areas
- Progressive enlargement, particularly without signs of infection
- Generalized lymphadenopathy, involving two or more non-contiguous regions
Radiologic imaging may reveal mediastinal lymphadenopathy, especially in acute lymphoblastic leukemia or CLL. A high standardized uptake value (SUV) on PET scan may indicate aggressive disease, but biopsy is essential for diagnosis.
Petechiae and easy bruising: distinguishing pathological from normal
Leukemia often presents with bleeding manifestations due to thrombocytopenia or platelet dysfunction. These signs may precede diagnosis in up to 24% of patients. Clinical features that differentiate pathologic bruising include:
- Bruising in uncommon areas, such as the back, buttocks, or upper arms
- Multiple bruises without known trauma, raising concern for spontaneous bleeding
- Petechiae, which are non-blanching, pinpoint red spots commonly seen on the lower legs, abdomen, or mucous membranes
- Concurrent bleeding, such as gingival bleeding or epistaxis
- Prolonged resolution time, with bruises taking over four weeks to heal
These findings are often misattributed to minor trauma, coagulation disorders, or even aging. However, persistent or unexplained bruising should always prompt a complete blood count and platelet evaluation.
Splenomegaly: detection challenges in primary care settings
An enlarged spleen can be a subtle but significant finding in leukemia. However, it is frequently missed during routine physical exams. Key points include:
- Physical exam sensitivity is limited (60–70%), especially in obese patients or those with a high diaphragm
- Palpable spleen tip >2 cm below the left costal margin suggests splenomegaly, especially when associated with symptoms
- Associated signs, such as early satiety, abdominal discomfort, or fullness in the left upper quadrant, may provide additional clues
Some healthy individuals—particularly thin patients—may have a naturally palpable spleen, creating diagnostic uncertainty. In such cases, ultrasound is the preferred imaging modality due to its sensitivity and lack of radiation.
Diagnostic Pitfalls in Primary Care Assessment
Early recognition of leukemia in primary care remains difficult due to overlapping symptoms with common conditions and several diagnostic pitfalls. These challenges often lead to delayed referrals—15% of leukemia patients see their GP three or more times before being referred to hospital care.
Anchoring bias: when common diagnoses overshadow leukemia
One of the most significant barriers is anchoring bias—when clinicians fixate on an initial diagnosis and interpret subsequent findings within that framework. This can result in serious delays. For example, a case of pancytopenia was initially attributed to pneumonia, postponing the diagnosis of acute myeloid leukemia (AML) until disease progression made it unmistakable.
A large VA-based study also illustrated this phenomenon: patients with documented congestive heart failure were one-third less likely to undergo pulmonary embolism testing, even though actual PE rates were unchanged. Similarly, early leukemia symptoms are often mistaken for:
- Viral infections (unexplained fevers)
- Depression (persistent fatigue)
- Immune deficiency (frequent infections)
Laboratory interpretation errors in early disease stages
Test Interpretation Challenges
Even when appropriate labs are ordered, early leukemia can be missed. Factors such as recent transfusions or medications may mask abnormal findings. Interpretation of peripheral smears and other tests is subjective and varies between observers, particularly in identifying and quantifying blasts.
Technical Errors
Errors in sample handling—such as improper fixation—or inconsistencies in flow cytometry gating can lead to misclassification. False-positive results have also been noted, especially with NPM1 marker testing, further complicating the diagnostic process.
When to order peripheral blood smears
According to NICE guidelines, urgent blood tests should be performed within 48 hours when leukemia symptoms are present. Still, only 68% of patients receive timely testing.
Peripheral smears are essential when CBC results show:
- Unexplained cytopenias
- Abnormal white cell counts
- Atypical morphology
Despite their value, these tests are underutilized due to time constraints and limited access to expert interpretation in primary care settings.

Conclusion
Primary care providers play a pivotal role in early leukemia detection. Diagnosis is often missed because early symptoms—such as fatigue, low-grade fever, or bruising—are attributed to more common conditions. To avoid missed or delayed diagnoses, clinicians should remain alert to:
- Persistent cytopenias not responding to standard treatment
- Systemic symptoms that exceed the severity of the presumed diagnosis
- Unusual bruising or bleeding patterns
- Repeated visits for unrelated or vague complaints
Tracking subtle lab trends and performing thorough physical exams are key. Reassessing initial assumptions and remaining open to alternate diagnoses are crucial—especially when symptoms evolve or fail to resolve.
Timely leukemia diagnosis in primary care relies on minimizing cognitive bias, recognizing early hematologic clues, and ensuring access to key diagnostic tools. Clinicians should adopt a systematic, vigilant approach and stay current with evolving guidelines. Doing so will not only improve early detection rates but also significantly enhance patient outcomes.
Frequently Asked Questions:
FAQs
Q1. What are the early signs of leukemia that doctors might overlook? Early signs of leukemia can include subtle blood count abnormalities, persistent fatigue, recurrent infections, unexplained weight loss, and night sweats. These symptoms are often mistaken for more common conditions, making early diagnosis challenging.
Q2. How can persistent fatigue be a sign of leukemia? Leukemic fatigue is characterized by excessive, persistent exhaustion that significantly disrupts daily activities and doesn’t improve with rest. Unlike ordinary tiredness, it’s often more severe and long-lasting, stemming from anemia caused by decreased red blood cell production.
Q3. What physical signs should raise suspicion for leukemia during a routine examination? Key physical signs include subtle lymphadenopathy (swollen lymph nodes), unusual bruising or petechiae (tiny red spots on the skin), and splenomegaly (enlarged spleen). These signs can be easily overlooked or misinterpreted during routine check-ups.
Q4. How do blood tests help in detecting early-stage leukemia? Blood tests, particularly complete blood counts (CBCs), can reveal abnormal levels of white blood cells, red blood cells, or platelets. Tracking these values over time is crucial, as gradual changes, even within normal ranges, may indicate early leukemia.
Q5. Why is leukemia often misdiagnosed initially? Leukemia is frequently misdiagnosed due to its symptoms mimicking common conditions like viral infections, stress, or depression. Cognitive biases, such as anchoring to initial diagnoses, and challenges in interpreting early-stage laboratory results can also contribute to misdiagnosis.

