Continuous Glucose Monitoring (CGM) for Type 2 Diabetes: Should It Be the Standard?

Abstract
Continuous glucose monitoring (CGM) has evolved into one of the most notable innovations in modern diabetes care. While its benefits are well established in type 1 diabetes, growing evidence suggests that CGM also holds considerable promise for individuals living with type 2 diabetes. This review provides an in-depth analysis of the clinical, economic, and policy dimensions of CGM adoption in type 2 diabetes, with a particular focus on whether CGM should be considered a standard of care in this population.
Clinical evidence, including randomized controlled trials, meta-analyses, and real-world studies, consistently shows that CGM use in type 2 diabetes leads to meaningful improvements in glycemic outcomes. Patients using CGM experience modest but statistically significant reductions in HbA1c, with pooled analyses indicating an average decrease of approximately 0.32 percent compared to traditional self-monitoring of blood glucose.[1] [2] In addition, CGM increases time in target glucose range, reduces glycemic variability, and enhances patient engagement in self-care. Importantly, these benefits extend to both insulin-treated individuals and selected patients using non-insulin therapies.
Beyond clinical outcomes, the economic implications of CGM adoption are central to its evaluation as a standard of care. Cost-effectiveness analyses suggest that CGM can be economically viable in specific populations, particularly those at high risk for hypoglycemia or those requiring intensive insulin therapy. However, results vary across healthcare systems, and broader implementation faces persistent challenges. These include high device costs, limited or inconsistent insurance coverage, time demands on clinicians, and disparities in reimbursement policies.[3] [4] Issues of healthcare equity also remain critical, as unequal access to CGM could exacerbate existing disparities in diabetes outcomes.
Regulatory and implementation perspectives further shape the debate. Standardizing CGM use requires alignment of device accuracy standards, integration into clinical workflows, and improved clinician education on interpreting and applying CGM data. Policymakers and payers must also address structural barriers, including fragmented reimbursement frameworks and variations in regional healthcare infrastructure.
In conclusion, CGM demonstrates potential to improve clinical outcomes and patient quality of life in type 2 diabetes. However, the evidence does not yet support universal standardization across all patient populations.[5] [6] Instead, a targeted, population-specific approach is recommended, prioritizing individuals who are most likely to benefit clinically and economically. Expanding insurance coverage, refining implementation strategies, and promoting equitable access will be essential steps in advancing CGM as a cornerstone of comprehensive type 2 diabetes management.
Keywords: Continuous glucose monitoring, Type 2 diabetes, Standard of care, Clinical effectiveness, Cost-effectiveness, Healthcare policy
Introduction
Type 2 diabetes mellitus (T2DM) represents one of the most pressing public health challenges of the 21st century. Current estimates indicate that more than 463 million adults worldwide are living with T2DM, and projections suggest that this figure could climb to nearly 700 million by 2045. Beyond its impact on individual health, the disease exerts a staggering economic toll. In the United States alone, diabetes-related expenditures are estimated at approximately 246 billion dollars each year, driven largely by hospitalizations, complications, and long-term disease management.[7]
Traditionally, the assessment of glycemic control in patients with T2DM has relied on two main strategies: self-monitoring of blood glucose (SMBG) using fingerstick testing and periodic measurement of glycated hemoglobin (HbA1c).[8] While both methods remain valuable, their limitations are increasingly recognized. HbA1c provides an average measure of glycemic control over several months, but it cannot reveal short-term fluctuations or identify acute hypoglycemic and hyperglycemic events. Similarly, SMBG captures glucose levels only at discrete points in time, often missing critical insights into glycemic variability, patterns of glucose excursions, and the percentage of time spent within target ranges. These gaps in monitoring may contribute to delayed treatment adjustments and suboptimal outcomes.
The emergence of continuous glucose monitoring (CGM) technology has begun to address many of these limitations. CGM systems provide real-time or near real-time glucose data, trend information, and predictive alerts that enable more precise and proactive management. Robust evidence has demonstrated the clinical benefits of CGM in children and adults with type 1 diabetes, as well as in adults with type 2 diabetes who require insulin therapy. These findings have led to the widespread recognition of CGM as a standard of care for insulin-dependent populations.
The question of whether CGM should be extended as a standard tool for all individuals with T2DM, regardless of insulin use, is more complex. This consideration requires a careful evaluation of multiple domains. Clinically, CGM has shown promise in improving glycemic control, reducing hypoglycemic episodes, and enhancing patient engagement in self-management. Economically, the potential to reduce long-term complications and hospitalizations must be weighed against the upfront costs of devices and sensors, as well as issues of insurance coverage and reimbursement. Implementation barriers, including patient education, health system integration, and disparities in access, remain notable challenges. Regulatory perspectives also play a crucial role, as approval pathways and guidelines influence adoption patterns across different healthcare systems. Finally, real-world data continue to emerge, providing valuable insights into the effectiveness of CGM outside controlled clinical trial environments.
This analytical review aims to provide a balanced and comprehensive overview of the current evidence base surrounding CGM use in type 2 diabetes. Rather than advocating for universal adoption or selective use, the objective is to equip clinicians, policymakers, and stakeholders with a clear understanding of the clinical, economic, regulatory, and practical considerations that shape this ongoing debate. By synthesizing findings across these domains, the review seeks to inform future decisions about whether CGM should evolve into a standard of care for the broader T2DM population.
Current Landscape of Type 2 Diabetes Management
Self-monitoring of blood glucose (SMBG) continues to play an important role in the management of individuals with diabetes who are treated with insulin. For this group, frequent capillary glucose checks help guide insulin dosing decisions and can prevent acute complications. However, routine use of SMBG is not generally recommended for patients with type 2 diabetes who are not on insulin therapy, as evidence has shown limited benefit in improving long-term glycemic control in this population.[9]
Despite its value, SMBG has several important limitations. It relies on intermittent fingerstick measurements, which provide only single time-point readings without capturing the broader context of glucose variability. As a result, it cannot detect asymptomatic episodes of hypoglycemia, particularly those that occur at night, nor does it adequately reflect postprandial glucose excursions. This is especially concerning because patients may present with apparently well-controlled glycated hemoglobin (HbA1c) values while still experiencing major fluctuations in glucose levels that remain undetected. In addition, the requirement for multiple daily blood samples can be burdensome, inconvenient, and uncomfortable for patients, potentially leading to poor adherence.[10]
Continuous glucose monitoring (CGM) systems were developed to address these shortcomings. Unlike SMBG, CGM measures glucose levels in the interstitial fluid through a subcutaneous sensor that records data automatically every few minutes. This continuous stream of information offers a more comprehensive and dynamic picture of glycemic patterns throughout the day and night. CGM not only captures fluctuations in real time but also reveals the impact of factors such as physical activity, meals, oral medications, and insulin administration on glucose levels. Furthermore, many CGM devices provide alerts for impending hypoglycemia or hyperglycemia, allowing for timely interventions and improved safety. By offering richer contextual data and reducing reliance on repeated fingerstick testing, CGM represents an advancement in diabetes management, particularly for individuals at risk of unrecognized glucose variability. [11] [12]
Research Objectives
This analysis aims to address several critical questions:
- What is the clinical evidence for CGM effectiveness in type 2 diabetes populations?
- How do cost-effectiveness considerations influence the case for standardization?
- What barriers currently limit CGM implementation and access?
- How do different regulatory and clinical guideline perspectives inform the debate?
- What are the implications of device accuracy and reliability for widespread adoption?
- How might implementation strategies differ across diverse patient populations?

Clinical Evidence for CGM in Type 2 Diabetes
Meta-Analytic Evidence
The most robust evidence for CGM effectiveness in type 2 diabetes comes from systematic reviews and meta-analyses of randomized controlled trials. A comprehensive meta-analysis of 14 randomized controlled trials including 1,647 patients found that CGM led to modest but statistically significant declines in HbA1c of approximately 0.32% [13] [14]. This reduction, while smaller than typically seen in type 1 diabetes populations, represents clinically meaningful improvement when applied across large populations.
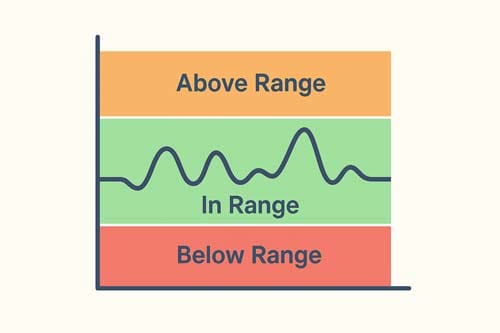
The effect was comparable in studies including individuals using insulin with or without oral agents (0.30% reduction) and those using oral agents only (0.29% reduction). CGM was also associated with increased time in range (+6.36%), decreased time below range (-0.66%), decreased time above range (-5.86%), and reduced glycemic variability (-1.47%) [15] [16].
Real-Time vs. Flash Glucose Monitoring
The evidence suggests differential effectiveness between CGM technologies. Real-time CGM showed a trend toward larger effect sizes (0.36% HbA1c reduction) compared to intermittently scanned CGM (0.16% reduction) [17], though both technologies demonstrated benefits. This finding has important implications for policy decisions, as different CGM technologies may warrant different implementation strategies.
Population-Specific Effectiveness
Insulin-Treated Type 2 Diabetes
Clinical trials have demonstrated particular benefits for adults with type 2 diabetes using intensive insulin therapy [18]. Studies in patients treated with basal insulin have shown consistent improvements in glycemic metrics. One randomized trial of adults with type 2 diabetes not on insulin demonstrated superior HbA1c reduction with CGM (-0.69%) compared to enhanced usual care (-0.33%), with 92% higher likelihood of achieving clinically remarkable HbA1c reduction ≥0.5% [19].
Non-Insulin-Treated Populations
Perhaps more notably for policy considerations is the emerging evidence in non-insulin-treated populations. Studies in individuals with type 2 diabetes not on insulin have shown effectiveness of CGM combined with diabetes education and remote monitoring [20]. However, despite recent clinical guidelines endorsing CGM use in individuals treated with nonintensive insulin regimens, insurance coverage remains limited or nonexistent [21].
Quality of Life and Patient-Reported Outcomes
Research indicates that CGM use in type 2 diabetes is associated with reduced HbA1c, improved glucose control, better overall health and quality of life, and increased self-care behaviors [22]. Importantly, the study identified self-care behaviors and self-care support factors (diabetes knowledge and health self-efficacy) as key variables linking CGM user experience to clinical outcomes [23].
Limitations of Current Evidence
Despite positive findings, systematic reviews note that the duration of included randomized controlled trials was relatively short, and few studies reported on important clinical outcomes such as adverse events, emergency department use, or hospitalization. Longer-term studies are needed to determine if short-term improvements in glucose control lead to improvements in clinically important outcomes [24].
Cost-Effectiveness Analysis
Economic Modeling Studies
The cost-effectiveness of CGM in type 2 diabetes has been evaluated through multiple economic modeling studies, with generally favorable results for specific populations. Analysis for US patients with type 2 diabetes receiving basal insulin therapy concluded that CGM is cost-effective compared with SMBG, suggesting that state Medicaid programs could benefit from broader CGM coverage [25].
In the base case analysis, CGM was dominant to SMBG, providing more quality-adjusted life years (6.18 vs 5.97) at lower cost ($70,137 vs $71,809) over a 10-year time horizon [26]. This finding suggests that CGM may actually reduce total healthcare costs while improving outcomes, a compelling argument for broader adoption.
International Cost-Effectiveness Evidence
Cost-effectiveness analyses from Canada demonstrate that for people with insulin-treated type 2 diabetes and poor glycemic control, real-time CGM is likely to be cost-effective relative to SMBG [27] [28]. Studies from the United States focusing on non-insulin-treated type 2 diabetes populations found that real-time CGM as a self-care tool is cost-effective, with repeated use potentially providing additional cost-effectiveness benefits [29] [30].
Professional vs. Personal CGM
Economic analysis of professional CGM use showed robust clinical benefits, with economic benefits observed particularly for patients who utilized professional CGM more than once within a one-year period or during diabetes therapy changes [31]. This suggests that different CGM implementation strategies may have varying economic profiles.
Barriers to Economic Analysis
While evidence suggests CGM use is safe and effective in improving glucose management with marked reduction in resource utilization, several challenges remain including the high cost of devices and limitations in approved clinical uses [32]. Additionally, longer follow-up studies are needed to assess CGM effectiveness in the long term and its relationship with diabetes complications [33].
Implementation Barriers and Access Issues
Insurance Coverage and Reimbursement
Major barriers to CGM prescribing include lack of insurance coverage for CGM costs to patients and time constraints for healthcare providers. Primary care clinicians identify these as noteworthy obstacles, reinforcing the need for improved clinician education and continued expansion of insurance coverage [34].
The Centers for Medicare & Medicaid Services eligibility criteria for CGM coverage ignore conclusive evidence supporting CGM use in various diabetes populations currently deemed ineligible. Although Medicaid is administered through CMS, there is no consistent Medicaid policy for CGM coverage in the United States [35] [36].
Healthcare Provider Perspectives
Despite uniform support for CGM by healthcare providers, ongoing challenges related to cost, insurance coverage, and difficulties with prescription processes remain major barriers to CGM use [37] [38]. CGM prescription often occurs in endocrinology practices, yet 50% of adults with type 1 diabetes and 90% of people with type 2 diabetes receive their diabetes care in primary care settings, highlighting the need for broader implementation strategies [39].
Socioeconomic and Health Equity Considerations
Research demonstrates that CGM uptake disparities can largely be overcome by eliminating cost barriers. CGM use was associated with improved HbA1c across all major racial/ethnic groups, highlighting broad CGM appeal, utilization, and effectiveness across underprivileged patient populations [40].
Studies of CGM programs for youth on public insurance show that expansion is limited by stringent barriers for CGM approval and difficult post-approval patient workflows, despite demonstrated success in improving glycemic outcomes [41] [42].
Clinical Workflow Integration
Most healthcare providers report that their CGM data review is valued by patients, although only half report having adequate time (45.1%) or an efficient process (56.1%) to review the data [43]. This suggests that successful CGM implementation requires not just device access but also healthcare system redesign to accommodate new workflows.
Patient-Level Barriers
Clinician-identified modifiable barriers include patient perceptions about disliking having devices on their body (73% for pumps, 63% for CGM), disliking alarms (61% for CGM), and not understanding what to do with device information (46% for CGM) [44]. Patient perspectives include convenience benefits over finger sticks but concerns about physical and auditory barriers, desire for privacy and autonomy, and need for adequate education about CGM use [45] [46].
Regulatory and Clinical Guideline Perspectives
American Diabetes Association Standards
The American Diabetes Association’s 2024 Standards of Care state that continuous glucose monitoring improves outcomes with injected or infused insulin and is superior to blood glucose monitoring [47]. The ADA guidelines include CGM in their treatment algorithms, particularly for insulin-treated populations.
Recent clinical guidelines from the American Diabetes Association and American Association of Clinical Endocrinology now endorse CGM use in individuals treated with nonintensive insulin regimens [48] [49], representing an expansion beyond traditional insulin-intensive populations.
International Consensus Statements
International consensus statements recommend that standardized CGM-derived metrics should be considered for use in all clinical studies in diabetes. The consensus aims to provide clinical information for investigators, regulators, companies, clinicians, and individuals with diabetes [50].
Asia-Pacific consensus recommendations state that continual use of CGM is recommended for individuals with diabetes on intensive insulin therapy and suboptimal glycemic control, or at high risk of problematic hypoglycemia. Continual/intermittent CGM may also be considered for individuals with type 2 diabetes on basal insulin regimen with suboptimal glycemic control [51] [52].
Regulatory Accuracy Standards
The National Institute for Clinical Excellence updated guidance for CGM in 2022, recommending CGM availability for all people with type 1 diabetes. Manufacturers can trade in the UK with CE marking without initial national assessment, contrasting with FDA and Australian regulatory processes.
The promotion of CGM to standard of care for type 1 diabetes and insulin-treated type 2 diabetes reflects robust evidence, with multiple devices available worldwide. However, accuracy metrics may no longer differentiate between devices as almost all exceed acceptable thresholds [53] [54].
Device Accuracy and Performance Considerations
Current Accuracy Standards
Recent head-to-head comparisons show that current CGM systems achieve high accuracy, with devices like the FreeStyle Libre 3 demonstrating superior performance (8.9% MARD) compared to competitors (13.6% MARD), with 91.4% of glucose values within ±20 mg/dL/±20% of reference [55] [56].
Third-generation CGM systems demonstrate accurate performance across the dynamic glycemic range during 14-day sensor wear periods [57]. Long-term implantable systems show 85% of values within 15/15% of reference with 9.6% MARD, with updated algorithms improving accuracy to 87% within reference range and 8.5% MARD [58] [59].
Accuracy in Clinical Context
The accuracy of continuous glucose monitors now supports their use by persons with diabetes and clinicians. Reviews of accuracy measures, contributing factors, and clinical implications demonstrate the utility of CGMs in clinical practice [60] [61].
While improvements in CGM accuracy have increased interest in hospital use, clinicians must be familiar with situations where CGM may not be accurate or reliable. Several mechanisms can impact device accuracy including mechanical factors, chemical interferences, or radiologic substances [62].
Real-World Performance
Real-world studies of newer CGM systems show acceptable performance with 17.2% MARD and 77.1% of sensors lasting the full 15-day wear duration. Approximately 69.5% of results were within 20 mg/dL or 20% of reference, with 98.8% of data falling within acceptable clinical accuracy zones [63] [64].
Discussion
Synthesizing the Evidence
The evidence regarding CGM standardization for type 2 diabetes presents a nuanced picture that defies simple yes-or-no answers. Clinical trials consistently demonstrate modest but meaningful improvements in glycemic control across diverse type 2 diabetes populations. Meta-analytic evidence shows statistically significant benefits in HbA1c reduction, time in range improvement, and reduced glycemic variability. However, the magnitude of these benefits varies by population, with potentially greater effects in insulin-treated individuals.
Cost-effectiveness analyses generally support CGM adoption, particularly in insulin-treated populations, with some studies suggesting CGM may be cost-saving overall. However, these analyses often rely on modeling assumptions about long-term outcomes that require validation through extended follow-up studies.
The Case for Targeted Implementation
Rather than universal standardization, the evidence suggests a more nuanced, population-specific approach may be optimal. Several factors support this perspective:
- Differential Clinical Benefits: Effect sizes vary meaningfully across populations, with stronger evidence in insulin-treated individuals.
- Resource Constraints: Healthcare systems face limited resources, and targeted implementation may maximize population-level benefits.
- Implementation Barriers: Current barriers to access and clinical workflow integration suggest that universal adoption may be premature without addressing systemic issues.
- Patient Preferences: Not all individuals may benefit equally from or desire CGM technology, supporting individualized rather than universal approaches.
Critical Implementation Considerations
Healthcare Equity
Evidence demonstrates that when cost barriers are removed, CGM benefits extend across diverse racial and ethnic groups [65]. This suggests that standardization policies must prioritize equitable access rather than assuming market-based distribution will achieve optimal outcomes.
Clinical Workflow Redesign
The finding that many healthcare providers lack adequate time or efficient processes for CGM data review [66] highlights that successful implementation requires healthcare system transformation beyond device availability. Standardization efforts must include provider training, workflow redesign, and potentially new care models.
Long-term Outcome Evidence
The limitation of short-term study durations and limited reporting of clinical outcomes [67] represents a monumental gap in the evidence base. While surrogate markers like HbA1c and time in range show improvement, demonstration of reduced complications, hospitalizations, and mortality requires longer-term studies.
Regulatory and Policy Implications
The patchwork of regulatory approaches and reimbursement policies creates barriers to rational implementation. The lack of consistent Medicaid policy for CGM coverage and eligibility criteria that ignore conclusive evidence [68] suggests need for policy reform alongside any standardization efforts.
International variations in regulatory approaches also highlight the need for evidence-based harmonization of standards and approval processes to ensure patients have access to beneficial technologies while maintaining appropriate safety oversight.
Future Research Priorities
Several research gaps must be addressed to inform evidence-based policy decisions:
- Long-term Clinical Outcomes: Studies with extended follow-up examining complications, mortality, and healthcare utilization.
- Implementation Science: Research on optimal strategies for CGM implementation across diverse healthcare settings and populations.
- Personalized Medicine: Studies identifying which patients are most likely to benefit from CGM technology.
- Health Economics: Real-world cost-effectiveness studies that account for implementation costs and long-term outcomes.
- Technology Development: Continued advancement in accuracy, usability, and integration with healthcare systems.
Limitations of Current Analysis
This analysis has several limitations that must be acknowledged. The evidence base continues to evolve rapidly, and newer studies may alter conclusions. The focus on published literature may introduce publication bias toward positive findings. Economic analyses rely on modeling assumptions that may not reflect real-world implementation. Finally, the analysis cannot account for all local contextual factors that influence implementation decisions.

Conclusion 
The question of whether continuous glucose monitoring (CGM) should become the standard of care for type 2 diabetes does not lend itself to a simple yes or no answer. While the technology offers clear advantages, its role in clinical practice must be carefully considered in the context of evidence, cost, health system readiness, and patient equity.
The clinical benefits of CGM are well established. Numerous studies demonstrate improvements in glycemic control, reductions in hypoglycemic events, and enhanced patient engagement with self-management. Cost-effectiveness analyses, although variable across healthcare systems, increasingly show favorable profiles, particularly for insulin-treated populations. Professional societies and expert consensus are moving toward broader endorsement, underscoring the growing recognition of CGM’s value.
Despite this momentum, several limitations caution against immediate universal adoption. Barriers to implementation remain substantial, including inconsistent reimbursement, lack of provider training, and the need to integrate CGM data into already burdened clinical workflows. Evidence is strongest for individuals with type 2 diabetes treated with insulin, but questions remain regarding the magnitude of benefit for those not using insulin. Furthermore, gaps persist in long-term outcomes research, particularly concerning complication rates, healthcare utilization, and population-level cost savings.
A more balanced approach emerges when these factors are considered together. The evidence supports prioritizing immediate CGM access for insulin-treated type 2 diabetes, where benefits are most consistently demonstrated. For non-insulin-treated populations, pilot programs and real-world evidence generation should be emphasized to clarify clinical utility and guide future expansion. At the same time, health systems must systematically address implementation barriers. This includes establishing sustainable reimbursement structures, training providers to interpret and act on CGM data, and developing workflow solutions that prevent technology from adding to clinical burden rather than alleviating it.
Equity must remain central to this process. Without deliberate efforts, CGM adoption risks widening disparities, with underserved populations least likely to benefit. Policymakers, payers, and providers should prioritize access pathways that ensure equitable distribution, recognizing that technology-driven care must serve all patients rather than only those with greater financial or geographic access.
Ultimately, the main issue may not be whether CGM should become the standard of care, but how it can be implemented in a way that maximizes health benefits while ensuring sustainability and fairness. A deliberate, evidence-based expansion strategy offers the most promising path forward. This requires alignment among healthcare providers, payers, policymakers, and technology developers, along with a commitment to ongoing research. As the evidence base grows and barriers are reduced, CGM may indeed become standard care for a broader range of people with type 2 diabetes. However, this transition should be guided by clinical outcomes, equity considerations, and system-level realities rather than by technological enthusiasm alone.

References:
- Effect of Continuous Glucose Monitoring on Glycemic Control in Patients With Type 2 Diabetes Treated With Basal Insulin: A Randomized Clinical Trial. PubMed
- Continuous glucose monitoring and metrics for clinical trials: an international consensus statement. ScienceDirect
- The use of continuous glucose monitoring in people living with obesity, intermediate hyperglycemia or type 2 diabetes. ScienceDirect
- Perceived impact of continuous glucose monitor use on quality of life and self-care for patients with type 2 diabetes. ScienceDirect
- The effectiveness of continuous glucose monitoring with remote telemonitoring-enabled virtual educator visits in adults with non-insulin dependent type 2 diabetes: A randomized trial. ScienceDirect
- Effectiveness of Continuous Glucose Monitoring on Metrics of Glycemic Control in Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis of Randomized Controlled Trials. PubMed
- Continuous Glucose Monitoring: Clinical Trials and Guidelines. PubMed
- Continuous glucose monitoring in adults with type 2 diabetes: a systematic review and meta-analysis. PubMed
- Continuous Glucose Monitoring: A Review of Recent Studies Demonstrating Improved Glycemic Outcomes. PubMed
- Clinical and economic outcomes of continuous glucose monitoring system (CGMS) in patients with diabetes mellitus: A systematic literature review. ScienceDirect
- Clinical and economic benefits of professional CGM among people with type 2 diabetes in the United States: analysis of claims and lab data. PubMed
- Cost-Effectiveness of a Continuous Glucose Monitoring Mobile App for Patients With Type 2 Diabetes Mellitus: Analysis Simulation. PubMed
- Clinical and economic outcomes of continuous glucose monitoring system (CGMS) in patients with diabetes mellitus: A systematic literature review. ScienceDirect
- Cost-effectiveness of continuous glucose monitoring and intensive insulin therapy for type 1 diabetes. PubMed
- Cost-utility of real-time continuous glucose monitoring versus self-monitoring of blood glucose in people with insulin-treated Type 2 diabetes in Canada. PubMed
- Cost-Effectiveness of Continuous Glucose Monitoring for Adults With Type 1 Diabetes Compared With Self-Monitoring of Blood Glucose: The DIAMOND Randomized Trial. PubMed
- A New Type 2 Diabetes Microsimulation Model to Estimate Long-Term Health Outcomes, Costs, and Cost-Effectiveness. ScienceDirect
- Continuous glucose monitoring for self-management of diabetes in people living with type 2 diabetes mellitus on basal insulin therapy: A microsimulation model and cost-effectiveness analysis from a US perspective with relevance to Medicaid. PubMed
- The cost-effectiveness of continuous glucose monitoring in type 1 diabetes. PubMed
- The Cost-Effectiveness of Real-Time Continuous Glucose Monitoring (RT-CGM) in Type 2 Diabetes. PubMed
- Clinician-Reported Barriers and Needs for Implementation of Continuous Glucose Monitoring. PubMed
- Overcoming Barriers to Diabetes Technology in Youth with Type 1 Diabetes and Public Insurance: Cases and Call to Action. PubMed
- Coverage for Continuous Glucose Monitoring for Individuals with Type 2 Diabetes Treated with Nonintensive Therapies: An Evidence-Based Approach to Policymaking. PubMed
- Increase Access, Reduce Disparities: Recommendations for Modifying Medicaid CGM Coverage Eligibility Criteria. PubMed
- Effect of CGM Access Expansion on Uptake Among Patients on Medicaid With Diabetes. PubMed
- Diabetes Specialists Value Continuous Glucose Monitoring Despite Challenges in Prescribing and Data Review Process. PubMed
- Optimal Use of Diabetes Devices: Clinician Perspectives on Barriers and Adherence to Device Use. PubMed
- Barriers and Facilitators to Uptake of Continuous Glucose Monitoring for Management of Type 2 Diabetes Mellitus in Youth. PubMed
- The use of continuous glucose monitoring in people living with obesity, intermediate hyperglycemia or type 2 diabetes. ScienceDirect
- Current Eligibility Requirements for CGM Coverage Are Harmful, Costly, and Unjustified. PubMed
- Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes-2024. PubMed
- Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2021. PubMed
- Diagnosis and Classification of Diabetes: Standards of Care in Diabetes-2024. PubMed
- Classification and Diagnosis of Diabetes: Standards of Care in Diabetes-2023. PubMed
- American Association of Clinical Endocrinology Consensus Statement: Comprehensive Type 2 Diabetes Management Algorithm – 2023 Update. ScienceDirect
- Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes-2023. PubMed
- Management of Hyperglycemia in Type 2 Diabetes, 2022. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). PubMed
- Guidelines for the management of type 2 diabetes: is ADA and EASD consensus more clinically relevant than the IDF recommendations? ScienceDirect
- Comparison of Point Accuracy Between Two Widely Used Continuous Glucose Monitoring Systems. PubMed
- Accuracy and Potential Interferences of Continuous Glucose Monitoring Sensors in the Hospital. ScienceDirect
- Accuracy and Reliability of the Sinocare Continuous Glucose Monitoring System. PubMed
- Stability, Accuracy, and Risk Assessment of a Novel Subcutaneous Glucose Sensor. PubMed
- Evaluating the accuracy, reliability, and clinical applicability of continuous glucose monitoring (CGM): Is CGM ready for real time? PubMed
- Perceived impact of continuous glucose monitor use on quality of life and self-care for patients with type 2 diabetes. ScienceDirect
- A Prospective Multicenter Evaluation of the Accuracy and Safety of an Implanted Continuous Glucose Sensor: The PRECISION Study. PubMed
- Continuous glucose sensor accuracy: beyond the headline metric. PubMed
- Accuracy of the Third Generation of a 14-Day Continuous Glucose Monitoring System. PubMed
- Clinical Implications of Accuracy Measurements of Continuous Glucose Sensors. PubMed
- Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations From the International Consensus on Time in Range. PubMed
- Continuous glucose monitoring and metrics for clinical trials: an international consensus statement. ScienceDirect
- International Consensus on Use of Continuous Glucose Monitoring. PubMed
- Asia-Pacific consensus recommendations for application of continuous glucose monitoring in diabetes management. ScienceDirect
- Continuous glucose monitoring and metrics for clinical trials: an international consensus statement. PubMed
- CGM accuracy: Contrasting CE marking with the governmental controls of the USA (FDA) and Australia (TGA): A narrative review. PubMed
- International Diabetes Federation European Policy Group Standards for Diabetes. ScienceDirect
- The use of continuous glucose monitoring in people living with obesity, intermediate hyperglycemia or type 2 diabetes. ScienceDirect
- Glucose management for exercise using continuous glucose monitoring (CGM) and intermittently scanned CGM (isCGM) systems in type 1 diabetes: position statement of the European Association for the Study of Diabetes (EASD) and of the International Society for Pediatric and Adolescent Diabetes (ISPAD) endorsed by JDRF and supported by the American Diabetes Association (ADA). PubMed
- Management of Hyperglycemia in Type 2 Diabetes, 2022. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). PubMed

