Comprehensive Geriatric Assessment (CGA)
Comprehensive Geriatric Assessment (CGA) is an organized evaluation method to multidisciplinary assessment of the elderly. CGA determines the appropriate care for them in the hospital or an elderly’s eligibility for clinical trials. It also evaluates elderly patients considering chemotherapy.
Advocates of CGA believe that a full evaluation of an older patient may help identify treatable health problems which can lead to better outcomes. CGA is useful in treating hospitalized, in-care, and with cancer older patients who needs primary care. Evidence shows that patients who receive CGA are more likely to return home, have less functional decline, and lower mortality rate.
Understanding Comprehensive Geriatric Assessment (CGA)
CGA is a timely assessment for persons over the age of 70. It can also be done after a doctor detects a potential risk to the patient’s health. Unlike the traditional healthcare system, CGA allows different experts (doctors, nurses, therapists, social workers) to work together and closely follow the patient until he or she is ready for discharge.
The team then reviews the results and revises the treatment plan accordingly. After a discussion with the
care-giver and patients, the physicians create and develop long term treatment plans and arrangements for rehabilitative services. When done right, comprehensive geriatric assessment can improve elderly’s functional status and quality of life. It can also reduce mortality and length of stay in hospitals. Studies find that older patients who stayed in hospitals a lot longer experience higher risk of functional decline.
Geriatric Syndrome
The term “geriatric syndrome” refers to common health problems in older adults that don’t fit in most organ-specific categories. It often has multi-factorial causes and can include several problems such as frailty, delirium, cognitive impairment, malnutrition, dizziness, pressure ulcers, and more. These conditions can have a major impact on the quality of life of the patient. Using comprehensive geriatric assessment, an appropriate plan and intervention can be started along with the help of a healthcare team.
History of Comprehensive Geriatric Assessment
The roots of modern CGA can be traced back 70 years ago through the work of Marjory Warren, a UK doctor. She used a specialized geriatric assessment unit to assess people in a large chronic disease hospital where she worked. The infirmary was largely populated by older individuals who are either bedridden or neglected by their relatives.
Warren categorized patients into two 1) the ones who can be discharged after treatment and 2) those who need continuous care after treatment. Warren was able to determine who could benefit the most from certain treatments and who needed further care. Because of her work, she became the leading advocate for comprehensive assessment of seniors. She was able to help them get placement in chronic hospitals or nursing homes as we know them today.
The orthogeriatric services of Devas and Irvine in Hastings created the first formal models of CGA in the 1960s. It laid the foundation for managing orthopedic problems in older adults with concurrent medical problems. Through the years, more models have been created by various specialists to manage treatment for elders.
Who Needs CGA?
The main significance of a geriatric assessment is to gather data for the physician in order to create an accurate diagnosis and plan of care for older people. It will allow them to create a treatment and rehabilitation program that will support the patient’s long-term needs. CGA is timely and comprehensive. It’s done usually to frail old people with complex problems.
All older adults over the age of 70 who are identified as being frail or at risk of frailty are recommended to have timely comprehensive geriatric assessment performed and documented in their health records. What is frailty? Frailty is a state of health related to aging. It is an inevitable part of growing old and like diabetes and Alzheimer’s, is considered a long-term condition
Comprehensive Geriatric Assessment: How It’s Done
CGA starts with gathering necessary information and data of the patient. Usually, a formal geriatric assessment tool and pre-visit questionnaire is sent to the patient before the initial meeting in order to save time and gather more information. The first assessment will involve a discussion including the patient and the caregiver. The first part revolves around getting to know the person in order to take effective care of them.
The information will gather data including general medical history, sources of social support (friends or family), mental health (depressive symptoms), and functional difficulties (vision or hearing). The team shall then communicate the outcomes of the comprehensive geriatric assessment to the family, care-givers, staff, and person involved.
Next would be the creation of a development or treatment plan. In this stage, the physician will use the assessment information to create future treatment goals and necessary advanced care plan for the patient. Lastly, is the implementation, monitoring, and revision (if needed) of the plan.
CGA is not a one-time process. The team has to monitor the older person’s health status on an ongoing basis. It is important to follow the geriatric assessment process in order for the patient to achieve maximum health and functional benefits. They will have to review progress and create revisions to the care plan if necessary.
Other CGA models focus on post-discharge geriatric assessment. Even newer models aim at primary and secondary prevention instead of rehabilitative and restorative care.
Who Performs the Assessment?
CGA is a multidisciplinary evaluation, which means it can’t be done by a geriatrician, nurse, or therapist alone. Common scenarios include different members of the geriatric assessment multidisciplinary team discussing with the elder during CGA.
The primary assessor is usually the senior physician or geriatrician. A pharmacist may do the medication review, while the nurse assists in personal care. If there are problems in balance and mobility, a physiotherapist is usually present. Finally, a social worker will deal with the social aspect of the case.
Depending on the health of the older adult, other paramedical health care professionals may be involved. For example, if there’s speech problems (speech and language therapist) and nutritional deficits (dietitian). Teams may vary depending on the condition of the senior, but more often than not everyone in the geriatric assessment team meets with the patient regularly. Communication between all members of the team is key to successful service.
Assessment of Physical Medical Conditions
This geriatric assessment gathers information about the patient’s co-morbid conditions and disease severity. It has a detailed medication review, nutritional status, and problem list. It includes every medical record including the older adult’s immunization status.
Assessment of Functional Status
An elderly’s functional status refers to his ability to perform daily tasks. It determines several core functions such as balance and mobility. Activities such as shopping, eating, bathing, and using the toilet, basically every task that is important for the patient to live an independent life.
These activities will determine the older person’s capacity to live without assistance or if he will require help from someone else to complete these basic tasks. Geriatricians can measure functional status by simply watching older patients complete various tasks such as putting on his shoes, writing on a piece of paper, and unbuttoning and buttoning a shirt.
Assessment of Mental Health Conditions
Old people are more prone to cognitive and mental health decline after the age of 65. By the age of 90, half of the elderly have some form of mental functioning disorder. Even old people who don’t have dementia are at a higher risk of accidents, delirium, missed medication, and other forms of disability. Some elders also don’t complain of any memory loss or any kind of mental disability, even when questioned. To help healthcare providers determine this correctly, they screen the older adults using simple questions during their initial visits.
Assessment of Social Health
This evaluation will focus on the social aspect of the senior’s life. Does he have available family and friends to provide personal support? Does he live with anyone that may mistreat and abuse him either mentally or physically?
Assessment of Environment
This assessment includes environmental data about the patient. What’s his/her house like? Is it a comfortable place to stay? What facilities does the patient have? Which of them are safe to use based on her condition?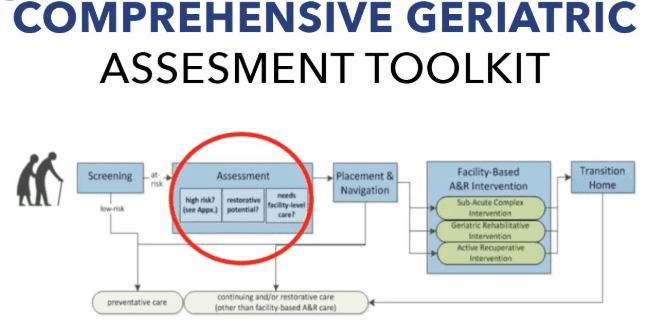
The assessment will allow doctors to detect various potential problems (for example: rugs inside the house that may cause elders to trip). After identifying these critical points, the team creates solutions. Everything is considered, from her transport facilities to the accessibility of her local resources.
Benefits of Comprehensive Geriatric Assessment
CGA is a structured approach to patient assessment that has helped encouraged older person and their family to consider effective and advance treatment to improve quality of life. It has proved valuable in modern medical treatment plans through the following benefits:
- Improved diagnostic accuracy
- Less complication during hospitalization or in-care treatment
- Optimized rehabilitation treatment
- Enhanced health and functional outcome
- Effective discharge planning and less readmission
Conclusion
Modern CGA is not yet perfect. We need more research to improve its applicability in different kinds of settings. But it’s undeniable that CGA provides a brilliant model of care to deliver effective healthcare to frail older patients. Since its inception, CGA has improved patient well-being and reduced hospital re-admissions.
Geriatrics
 |
Geriatrics and related calculators
Calculators / Tools
Activities of daily living (ADL) assessment tool ADAM (Androgen Deficiency in Aging Males) Aging Males’ Symptom (AMS) scale Beers Criteria – New Patient-specific reporting possible Berg Balance Scale – Fall risk/balance assessment Geriatric changes with age Geriatric Depression Scale (GDS) – Short Version Geriatric Depression Scale (GDS) – Long Version International Index of Erectile Function (IIEF) International Prostate Symptom Score (IPSS) Medication Appropriateness Index Calc Overactive Bladder 8-question Screener – (OAB-q) Overactive Bladder Symptom Score (OABSS) SLUMS-Screening for Cognitive Impairment in Older AdultsUrinary Incontinence Treatment /Symptom Calculator
Medical Articles & News
Comprehensive Geriatric Assessment

