De-prescribing in Older Adults: Why “Less is More” is Easier Said Than Done
Abstract
The adage “less is more” has gained significant traction in modern healthcare, particularly in geriatric medicine, where polypharmacy presents substantial challenges. De-prescribing, defined as the planned and supervised process of discontinuing inappropriate medications, has emerged as a critical intervention for optimizing medication management in older adults. This analytical review examines the complex landscape of de-prescribing implementation, exploring the multifaceted barriers that make this seemingly straightforward concept challenging to execute in clinical practice. This paper analyses current literature and identifies key obstacles, including healthcare provider resistance, patient attitudes, system-level barriers, and the lack of standardized protocols. While evidence demonstrates that de-prescribing interventions can significantly reduce the proportions of older adults with potentially inappropriate medications and improve medication compliance [1], the translation from research to routine clinical practice remains problematic. The paper synthesizes findings from systematic reviews, intervention studies, and qualitative research to provide a comprehensive understanding of why implementing “less is more” approaches in geriatric prescribing continues to be more complex than anticipated. Despite substantial evidence supporting the safety and efficacy of de-prescribing, multiple stakeholder perspectives reveal deeply entrenched barriers that require systematic approaches to overcome. This analysis concludes that the successful implementation of de-prescribing requires coordinated efforts simultaneously addressing individual, professional, and systemic factors.
Keywords: de-prescribing, polypharmacy, older adults, medication management, healthcare barriers, clinical decision-making
Introduction
The “less is more” concept in healthcare has never been more relevant than in contemporary geriatric medicine. As populations age globally, the phenomenon of polypharmacy—commonly defined as the concurrent use of five or more medications—has reached epidemic proportions among older adults. Polypharmacy is common in older adults and is associated with adverse drug events, cognitive and functional impairment, increased healthcare costs, and increased risk of frailty, falls, hospitalizations, and mortality [2]. De-prescribing has emerged as a critical intervention strategy in this context, representing a paradigm shift from the traditional “more is better” approach to medication management.
De-prescribing, defined as the planned, supervised process of medication discontinuation [3], offers a promising solution to the growing challenges of inappropriate polypharmacy. The theoretical foundation is compelling: by systematically removing medications that are no longer beneficial, potentially harmful, or inappropriate for a patient’s current health status, clinicians can improve health outcomes while reducing medication-related risks. However, the practical implementation of de-prescribing has proven significantly more complex than the underlying principle suggests.
Current demographics and prescribing patterns underscore the urgency of addressing this challenge. In the UK, it is estimated that around 20% of adults are in receipt of ≥5 or more regular drugs, and >1 in 20 adults take ≥10 or more regular medications [4]. More concerning, two-thirds of patients given >10 medicines are exposed to potentially serious [5] adverse events. These statistics illustrate the magnitude of the challenge facing healthcare systems worldwide.
Despite growing recognition of the need for de-prescribing and accumulating evidence of its benefits, implementation remains inconsistent and often unsuccessful. Evidence on barriers and facilitators to deprescribing has underscored how deprescribing in routine clinical practice can be complex and challenging [6]. This complexity stems from multiple interconnected factors operating at individual, professional, and system levels, creating a web of resistance that makes the straightforward concept of “less is more” remarkably difficult to implement.
This analytical review aims to examine the multifaceted nature of de-prescribing implementation challenges, exploring why a concept that appears logical and evidence-based encounters such significant obstacles in clinical practice. Through systematic analysis of current literature, this paper aims to comprehensively understand the barriers, facilitators, and complex dynamics that influence de-prescribing success, ultimately addressing the fundamental question: why is “less is more” easier said than done in geriatric medication management?

Literature Review and Current State of Evidence
Theoretical Framework and Definition
The theoretical foundation of de-prescribing rests on several key principles that distinguish it from simple medication discontinuation. Deprescribing (i.e., the process of discontinuing an inappropriate medication) requires time, knowledge, and care, but there is a lack of education, support, and guidelines for this critical clinical task [7]. This complexity is reflected in the various definitions in the literature, though most converge on planned, supervised medication withdrawal or dose reduction.
The evidence base supporting de-prescribing has grown substantially over the past decade. Extensive evidence suggests that deprescribing is feasible and safe, though questions remain about the potential clinical benefits [8]. This statement encapsulates a crucial tension in the field: while safety and feasibility have been established, the translation to meaningful clinical outcomes remains variable.
Effectiveness of De-prescribing Interventions
Recent systematic reviews and meta-analyses have provided increasingly robust evidence for de-prescribing effectiveness. Compared to routine care, deprescribing interventions significantly improve clinical outcome indicators for older adults [9]. More specifically, thirteen studies (92.9%) found deprescribing interventions reduced the number of drugs and/or doses taken. No studies found threats to patient safety regarding primary outcomes, including morbidity, hospitalizations, emergency room use, and falls [10].
The safety profile of de-prescribing interventions is particularly reassuring. RCT primary outcomes found that deprescribing is safe and reduces the number of drugs or doses. Five RCTs found a significant deprescribing impact on HRQOL, cost, or hospitalization [11]. These findings provide a solid foundation for the theoretical appeal of de-prescribing approaches.
However, the translation from research settings to clinical practice reveals significant challenges. Comprehensive medication review may have reduced all-cause mortality (OR 0.74, 95% CI: 0.58 to 0.95, I2 = 0, k = 12, low COE) but probably had little to no effect on falls, health-related quality of life, or hospitalizations (low to moderate COE) [12]. This mixed evidence suggests that while de-prescribing can be effective, the magnitude and consistency of benefits may vary considerably across different contexts and populations.
Economic Considerations
The economic dimension of de-prescribing presents another layer of complexity. Although results varied across settings, time horizons, and interventions, most were cost-effective according to the World Health Organisation threshold. Deprescribing interventions are promising economically, but more studies are needed [13]. The economic argument for de-prescribing is theoretically compelling—fewer medications should result in lower pharmaceutical costs and reduced healthcare utilization due to fewer adverse events.
However, the reality is more nuanced. Overall, 85% of the interventions were cost-saving, dominated usual care, or were cost-effective considering 1 gross domestic product per capita [14]. While these findings are encouraging, they also highlight the variability in economic outcomes and the need for more comprehensive economic evaluations.
Global Perspective and Implementation Challenges
The challenges of implementing de-prescribing are not unique to any single healthcare system. There is increasing recognition of the need for deprescribing of inappropriate medications in older adults. However, efforts to encourage implementation of deprescribing in clinical practice have resulted in mixed results across settings and countries [15] [16]. This global perspective underscores that the challenges are fundamental rather than system-specific.
The heterogeneity of interventions and contexts makes generalization difficult. Deprescribing intervention studies are inherently heterogeneous because of the complexity of interventions employed and often do not reflect the real-world [17]. This gap between research and practice represents a critical barrier to implementation.
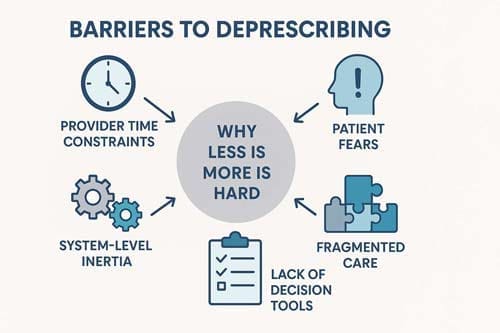
Barriers to De-prescribing Implementation
Healthcare Provider Barriers
Healthcare providers face numerous obstacles when attempting to implement de-prescribing in clinical practice. The barriers were patient-specific, prescriber-specific, and healthcare provision and system. Prescriber deprescribing competencies, medication-specific outcomes, availability of empirical evidence, and the pharmacist’s role were the enablers identified [18].
One of the most significant prescriber-specific barriers is the lack of education and training in de-prescribing principles. Improving competencies on deprescribing was repeatedly cited as an enabler by physicians. The development of targeted educational training can help reduce the obstacles prescribers face [19]. This suggests that many healthcare providers feel unprepared to undertake de-prescribing initiatives despite their theoretical understanding.
Time constraints represent another significant barrier. These include time constraints, fear of consequences, and the perception that older adults are reluctant to stop medications [20] [21]. The de-prescribing process requires careful consideration of each medication’s indication, effectiveness, and potential for withdrawal, which can be time-consuming in busy clinical environments.
Fear of adverse consequences also plays a significant role in provider reluctance. Numerous tools have been developed for clinicians to facilitate deprescribing, yet most require substantial time and, thus, may be difficult to implement during routine healthcare encounters [22]. Concerns about patient reactions and potential liability issues often compound this fear.
Patient-Related Barriers
Patient attitudes and beliefs toward de-prescribing represent a complex set of barriers that healthcare providers must navigate. Four barriers were identified: favourable perceptions of medications, fear of medication discontinuation, the complexity of the healthcare system, and discouragement from healthcare professionals; and seven enablers were identified: medication safety concerns, patient autonomy and confidence, education, follow-up, deprescribing strategies, relationships with physicians, and patient-perceived benefits of deprescribing [23].
Interestingly, patient willingness to use de-prescribing is higher than many healthcare providers assume. Despite this perceived hesitancy, 92% of older adults in the United States strongly agree that they would be willing to take less medication if their provider recommended this [24]. This finding suggests that perceived patient resistance may be more of a barrier in providers’ minds than in actual patient attitudes.
However, specific patient concerns remain significant. Older age and female sex increased the odds of willingness to deprescribe; higher concerns about stopping medications decreased the odds. These findings suggest addressing patients’ concerns about stopping their medicines may contribute to deprescribing success [25].
The finding further illustrates the complexity of patient attitudes, namely that perceptions of medication burden were associated with patients’ total daily pills (median 16) and PIMS (median 7), yet 61% agreed that all their medicines were necessary [26]. This paradox highlights the disconnect between objective medication burden and subjective perceptions of necessity.
System-Level Barriers
Healthcare system factors create additional layers of complexity for de-prescribing implementation. Health system complexity and direct discouragement from healthcare providers were barriers uniquely identified in the older adult population. This population would benefit from interventions to increase their medication literacy, confidence, and autonomy in the deprescribing journey [27].
The fragmentation of care across multiple providers presents particular challenges. Theme 2, ‘provider-related barriers’, discusses trust, short office visits, lack of communication, and various providers [28]. When patients receive care from multiple specialists, coordinating de-prescribing efforts becomes significantly more complex.
System-level incentives often work against de-prescribing initiatives. Having a care goal known to every HCP involved in managing a patient is an enabler for deprescribing. At the same time, the lack of incentives and remuneration for HCPs who de-prescribe may not necessarily be a barrier to deprescribing [29]. However, the healthcare payment structure typically rewards prescribing rather than de-prescribing activities.
Technological and Decision Support Barriers
The lack of adequate decision support tools represents another significant barrier. There is a need to develop a CDSS for deprescribing. There are, if any, guidelines or support for deprescribing, which is regarded as a significant obstacle [30]. This gap in technological support leaves healthcare providers without the tools they need to make informed de-prescribing decisions.
The requirements for effective decision support systems are demanding. A clinical decision support system must be user-friendly and not require more time than necessary to obtain relevant and reliable information. Physicians need fast, simple, and up-to-date information filtered, summarised, and synthesized from reliable sources [31] [32]. Meeting these requirements while maintaining clinical accuracy represents a significant technological challenge.

Patient Perspectives and Attitudes
Willingness to De-prescribe
Patient attitudes toward de-prescribing are more complex and nuanced than often assumed by healthcare providers. Research consistently demonstrates that older adults are generally willing to de-prescribe when approached appropriately. Most older adults and caregivers are eager to have one of their or their care recipient’s medications deprescribed. However, different predictors (characteristics/attitudes) of this willingness were identified in these two groups [33] [34].
The level of willingness is remarkably high when patients are adequately informed and involved in the decision-making process. 93% of participants were willing to deprescribe if their physician agreed [35] [36]. This finding challenges the assumption that patients are inherently resistant to medication changes.
However, patient willingness varies significantly based on several factors. Older adults’ health outcome priorities related to medication use are associated with their desire to consider deprescribing. Future research should determine how best to elicit patients’ health outcome priorities to facilitate goal-concordant medication-use decisions [37].
Factors Influencing Patient Attitudes
Several key factors influence patient attitudes toward de-prescribing. The willingness of both older adults and carers to have one or more medications deprescribed was influenced by the following main themes: their perception of the appropriateness of that medication; fear of outcomes of withdrawal; dislike of taking medications; and the availability of a process for withdrawal (including a discussion with a healthcare professional and knowing that the medication could be restarted if necessary) [38].
The role of healthcare provider communication is critical in shaping patient attitudes. A patient’s regular GP was identified as a strong influence both for and against medication withdrawal [39]. This finding underscores the importance of the therapeutic relationship in successful de-prescribing initiatives.
Patient education and information provision are also crucial factors. Consumer-centric tools could improve older adults’ self-efficacy in initiating deprescribing conversations. Removing barriers and implementing enablers may empower older adults to initiate deprescribing conversations with providers to take fewer medications [40].
Cultural and Individual Variations
Patient attitudes toward de-prescribing vary significantly across cultural contexts and individual circumstances. Attention should be given to concerns about stopping specific medicines, especially among patients using multiple glucose-lowering medications, who may be more eligible but were less willing to accept deprescribing [41] [42]. This finding highlights the importance of considering medication-specific factors in patient attitudes.
The complexity of patient decision-making is further illustrated by the finding that most older people living with cognitive impairment are willing to deprescribe. Addressing previous bad experiences with stopping a medication and stress when changes are made to medications may be key points to discuss during deprescribing conversations [43].
Healthcare System Factors
Organizational Barriers
Healthcare systems present numerous organizational barriers that impede de-prescribing implementation. In conceptual models of deprescribing, multilevel factors of the patient, clinician, and healthcare system are all related to the efficacy of deprescribing. Numerous tools have been developed for clinicians to facilitate deprescribing, yet most require substantial time and, thus, may be difficult to implement during routine healthcare encounters [44].
The fragmentation of care across multiple providers and settings creates coordination challenges. Older patients often have multimorbidity, frequently resulting in polypharmacy. Independently, multimorbidity and polypharmacy are among the most significant risk factors for inappropriate medication, adverse drug reactions, adverse drug events, and morbidity, leading to patient harm and hospitalizations [45].
Implementation Challenges
Implementing de-prescribing interventions faces significant challenges related to existing healthcare structures and processes. Yet, there has been limited consideration of implementation factors in prior deprescribing interventions, especially regarding the personnel and resources in existing healthcare systems and the feasibility of incorporating components of deprescribing interventions into the routine care processes of clinicians. Future trials require a more balanced consideration of effectiveness and implementation when designing deprescribing interventions [46].
The need for system-level changes is evident in the finding that deprescribing interventions may need to be individually tailored to target the unique barriers and opportunities to deprescribing in different clinical settings. Introduction of national policies to encourage deprescribing may be beneficial, but they need to be evaluated to determine if there are any unintended consequences [47].
Resource and Infrastructure Requirements
Successful de-prescribing implementation requires significant resources and infrastructure support. Dissemination included an implementation toolkit and four dashboards that collect and display data from the electronic medical record to monitor utilization of VIONE, track medication discontinuations, and prospectively identify veterans who may be candidates for deprescribing. Between 2016 and the present, VIONE has been adopted at >130 medical centres and influenced almost 700,000 unique patients [48].
The VIONE example demonstrates that large-scale implementation is possible but requires substantial organizational commitment and resources. The VIONE methodology and informatics tools were widely disseminated and successfully adopted and sustained nationally in a high-reliability organization, reducing PIM use by older adults and improving quality and patient safety [49].
Clinical Decision-Making and Tools
Current State of Clinical Guidelines
The availability and quality of clinical guidelines for de-prescribing remain significant challenges. Most guidelines contained recommendations regarding who (75%, n=60), what (99%, n=89), and when or why (91%, n=73) to deprescribe; however, fewer guidelines (58%, n=46) contained detailed guidance on how to deprescribe [50] [51]. This gap in procedural guidance leaves healthcare providers without clear direction on implementation.
The variability in guideline quality and content is problematic. Deprescribing recommendations had substantial variability in their format and terminology [52]. This inconsistency makes it difficult for healthcare providers to develop systematic approaches to de-prescribing.
Decision Support Tools
Developing practical decision support tools for de-prescribing remains a work in progress. Of the 257 full-text records assessed, 11 met the eligibility criteria, detailing the development of 10 deprescribing tools and guidelines in CKD. These were categorized into four types: (1) comprehensive deprescribing process guidance (n = 2); (2) protocols for comprehensive deprescribing care models (n = 2); (3) drug-specific deprescribing algorithms (n = 4); and (4) screening tools for specific deprescribing steps (n = 2) [53].
The challenge of developing practical tools is highlighted by the finding that Algorithm development was guided by existing deprescribing protocols intended for the general population and the expert opinions of our study team, due to a lack of background literature on HD-specific deprescribing protocols. There is no universally accepted method for validating clinical decision-making tools [54].
Provider Preferences and Needs
Understanding healthcare provider preferences for de-prescribing interventions is crucial for successful implementation. Continued efforts to improve clinicians’ ability to make prescribing decisions, especially around deprescribing, have many potential benefits, including decreased pharmaceutical and health care costs, fewer adverse drug events and complications, and improved patient involvement and satisfaction with their care. Future work, whether as research or quality improvement, should incorporate clinicians’ preferences for interventions, as greater buy-in from front-line staff leads to better adoption of changes [55].
The complexity of provider needs is reflected in the requirement for fast, up-to-date, and straightforward information filtered, summarised, and synthesized from reliable sources. The information should preferably be integrated into a pre-existing electronic health record [56]. Meeting these requirements while maintaining clinical accuracy represents a significant challenge for tool developers.
Successful Implementation Strategies
Comprehensive Approaches
Successful de-prescribing implementation requires comprehensive approaches that address multiple levels of barriers simultaneously. There is evidence that even simple interventions, such as direct deprescribing targeted at risky medications and explicit criteria-based approaches, effectively reduce inappropriate prescribing. On the other hand, if the goal is to improve clinical outcomes such as hospitalization and emergency department visits, patient-centred multimodal interventions such as a combination of medication review, multidisciplinary collaboration, and patient education are likely to be more effective [57].
The importance of comprehensive approaches is further supported by the finding that five studies had significant, positive primary outcomes related to health-related quality of life (HRQOL), cost, and/or hospitalization, with four reporting patient-centred elements in their intervention [58]. Patient-centred approaches are crucial for achieving meaningful clinical outcomes.
Multidisciplinary Collaboration
Successful de-prescribing often requires multidisciplinary collaboration. Most deprescribing interventions included some medication review with or without a supportive educational component (n = 11, 85%), and in general, were delivered within a pharmacist-physician care collaboration. Settings included community pharmacies, primary care/outpatient clinics, and patients’ homes [59].
The role of pharmacists in de-prescribing initiatives is vital. Deprescribing is a standard recommendation by pharmacists performing medication reviews in care homes; however, requiring prescriber authorization is a barrier [60] [61]. This finding highlights the need for clear role definitions and collaborative protocols.
Patient-Centered Approaches
Patient-centred approaches are essential for successful de-prescribing implementation. This is the first deprescribing process developed using knowledge of the patients’ views of medication cessation; it focuses on engaging patients throughout the process to improve long-term health outcomes. Despite a comprehensive literature review, there is still a lack of evidence on which to conduct deprescribing.
The finding reinforces the importance of patient engagement, which evidence suggests that empowering the individual to initiate such conversations with their provider leads to the alignment of medication regimens with their health goals and preferences [62].
Education and Training
Education and training are crucial components of successful de-prescribing implementation. The facilitators included cost-effectiveness and time effectiveness, avoidance of side effects, the clinical pharmacist’s role, the need for system(s) to help apply deprescribing, and patient counselling/education. Similarly, barriers included lack of knowledge of the deprescribing term and process, patient comorbidities, risk/fear of conflict between physicians and clinical pharmacists, lack of documentation and communication, lack of time or crowded clinics, and patient resistance/acceptance [63].
The need for systematic education is highlighted by the study, identifying several factors affecting family medicine physicians’ deprescribing behaviour. The use of theoretical underpinning design helped to provide a comprehensive range of factors to be considered when defining targets for intervention(s) [64].
Future Directions and Recommendations
Research Priorities
Future research in de-prescribing should address several key priorities. Deprescribing research faces many challenges, such as identifying and employing the optimal outcome measures. Further, there is uncertainty about which deprescribing approaches are likely to be most effective and in what contexts [65].
The need for implementation research is critical. Thus, finding practical, sustainable ways to implement deprescribing is a priority for future research [66]. This emphasis on implementation reflects the growing recognition that effectiveness alone is insufficient for successful de-prescribing initiatives.
Moving Beyond Barriers and Facilitators
The field of de-prescribing research needs to evolve beyond simply identifying barriers and facilitators. We have come to the point where barriers and facilitators around deprescribing are well-established. There is an urgent need to translate this knowledge into strategies and tools that can impact clinical practice and lead to practical and sustained deprescribing efforts [67].
This evolution requires a shift in focus. Therefore, the research focus should shift to developing ways to address known barriers and harness knowledge of facilitators. There is an urgent need to translate this knowledge into strategies and tools that can impact clinical practice and lead to practical and sustained deprescribing efforts [68] [69].
Technology and Innovation
The development of effective technology solutions remains a priority for the field. Future efforts should continue to consider ways to leverage electronic medical record data and other relevant informatics tools to provide customised clinical decision support to further medication optimisation and deprescribing efforts [70].
The potential for technology to address some of the current barriers is significant. This review highlights the need for more robust, evidence-based deprescribing tools tailored to the complex needs of CKD populations [71], though this principle applies beyond specific patient populations.
Policy and System Changes
System-level changes and policy initiatives may be necessary to support widespread de-prescribing implementation. There is a need for regulations and policies to support the identified enablers among HCPs and reduce the barriers to the effective deprescribing process [72].
The importance of policy support is highlighted by the finding that the development and implementation of patient-centred opioid deprescribing policies are both essential and feasible, if key challenges such as structural stigma and the complex interplay between pain and opioid use disorder are recognized and addressed.
Quality Improvement and Sustainability
Ensuring the sustainability of de-prescribing initiatives requires ongoing quality improvement efforts. Management strategies that target all healthcare system levels are needed to overcome these challenges. Future studies may consider large multicenter prospective designs to establish the effects and sustainability of deprescribing interventions on clinical outcomes [73].
The sustainability challenge is reflected in the finding that long-term sustainability remains limited despite the proven feasibility to discontinue medications safely, and re-prescribing of discontinued medications often occurs when the intervention period ends [74].
Discussion
The analysis presented in this review reveals the complex and multifaceted nature of de-prescribing implementation challenges. While the principle of “less is more” appears straightforward and is supported by substantial evidence, the practical implementation of de-prescribing interventions encounters significant barriers at multiple healthcare system levels.
The Paradox of Evidence and Implementation
One of the most striking findings from this analysis is the apparent paradox between the strength of evidence supporting de-prescribing and the challenges encountered in implementation. The evidence base demonstrates that hospital deprescribing interventions are feasible, generally effective at reducing PIMs, and safe. However, the current evidence is limited and of low quality, and the impact on clinical outcomes is unclear [75]. This paradox highlights the difference between demonstrating efficacy in controlled research settings and achieving effectiveness in real-world clinical practice.
The safety profile of de-prescribing interventions is reassuring and should provide confidence to healthcare providers. The narrative synthesis indicated that most interventions resulted in some evidence of medication reduction, while we found primarily no evidence of an effect for other outcomes. Deprescribing interventions likely resulted in medication reduction, but proof on different outcomes, particularly adverse events, or vulnerable subgroups or settings was limited [76] [77]. This finding suggests that healthcare providers may overestimate the fear of adverse consequences from de-prescribing.
The Role of System Complexity
The complexity of healthcare systems emerges as a central theme in understanding implementation challenges. Although potentially beneficial, clinicians struggle to overcome structural, organizational, technological, and cognitive barriers to deprescribing, limiting its use in clinical practice. Deprescribing science would benefit from a unifying conceptual framework to prioritize research [78]. This complexity suggests successful implementation requires coordinated efforts across multiple system levels rather than individual initiatives.
The fragmentation of care across multiple providers and settings creates challenges for de-prescribing implementation. When patients receive care from multiple specialists, each focused on their specific area of expertise, the coordination required for effective de-prescribing becomes exponentially more complex. The lack of integrated decision support tools and standardized protocols compounds this fragmentation.
The Human Factor
Perhaps most importantly, this analysis reveals that de-prescribing is fundamentally a human process that depends on relationships, communication, and trust. This study highlights that discussions between the healthcare professional and the older adult or carer about withdrawing medications should address reasons for deprescribing. GPs should be aware of their significant influence on patients and regularly discuss the appropriateness of current medication use with older adults and their carers [79].
The importance of the therapeutic relationship cannot be overstated. Patients are generally willing to engage in de-prescribing when approached by trusted healthcare providers who take the time to explain the rationale and involve them in decision-making. However, the healthcare environment often does not provide adequate time or incentives for these crucial conversations.
The Need for Comprehensive Approaches
The evidence consistently points to the need for comprehensive, multifaceted approaches to de-prescribing implementation. Simple interventions may effectively reduce inappropriate prescribing, but achieving meaningful clinical outcomes requires more sophisticated strategies that simultaneously address patient, provider, and system factors.
The success of initiatives like VIONE demonstrates that large-scale implementation is possible but requires substantial organizational commitment and resources. In addition, a total of >1.6 million medication orders have been discontinued by >15,000 providers. The VIONE methodology and informatics tools were widely disseminated and successfully adopted and sustained nationally in a high-reliability organization, reducing PIM use by older adults and improving quality and patient safety [80]. This example provides a roadmap for system-level implementation and highlights the required significant resources.
Limitations and Future Directions
This analysis has several limitations that should be acknowledged. First, the literature on de-prescribing implementation is still evolving, and small sample sizes, short follow-up periods, and heterogeneous interventions limit many studies. Second, the contexts of the cultural and healthcare systems vary significantly across studies, making generalisation challenging. Third, the definition of successful de-prescribing varies across studies, making comparison difficult.
Future research should focus on developing and testing standardized approaches to de-prescribing implementation that can be adapted to different healthcare contexts. Future research should focus on designing studies powered to examine harms, patient-reported outcomes, and effects on vulnerable subgroups [81]. Additionally, there is a need for longer-term follow-up studies to assess the sustainability of de-prescribing interventions and their impact on clinical outcomes.
The development of practical decision support tools remains a priority. A co-designed template or best practice guide should be developed and employed, containing information on aspects of deprescribing recommendations that are essential or preferred by end-users [82]. These tools should be integrated into existing electronic health record systems and designed to support clinical decision-making without burdening healthcare providers.

Conclusion
The analysis presented in this review demonstrates that while “less is more” represents a compelling principle for geriatric medication management, its implementation through de-prescribing interventions is far more complex than initially apparent. The challenges are not insurmountable but require coordinated efforts that simultaneously address individual, professional, and system-level factors.
The evidence base supporting de-prescribing is robust and continues to grow. In any setting, deprescribing was able to significantly reduce the number of total and of potentially inappropriate medications (PIMs) in older patients (low certainty of evidence) and to reduce the proportion of participants potentially having several PIMs (moderate certainty of evidence) [83]. However, the translation from research evidence to routine clinical practice remains challenging.
The key to successful implementation is recognising that de-prescribing is not simply a technical process of medication removal but a complex human interaction that requires trust, communication, and shared decision-making. Healthcare providers need adequate training, time, and support to engage in these conversations effectively. Patients need education, reassurance, and involvement in decision-making processes. Healthcare systems must provide the infrastructure, incentives, and support necessary for sustainable implementation.
The “less is more” principle remains valid and essential for geriatric medication management. However, achieving “less” requires “more” in terms of time, resources, education, and systematic approaches to implementation. The paradox of de-prescribing is that simplifying medication regimens requires complex, multifaceted interventions that address the full spectrum of factors influencing prescribing decisions.
Moving forward, the field must shift focus from demonstrating the effectiveness of de-prescribing to understanding and addressing the implementation challenges preventing widespread adoption. That is, translating existing knowledge into strategies and tools that can impact clinical practice and lead to practical and sustained deprescribing efforts. The promise of “less is more” can be realised only through this comprehensive approach in routine clinical practice.
The ultimate goal is not simply to reduce the number of medications that older adults take, but to optimise their medication regimens to improve health outcomes, reduce adverse events, and enhance quality of life. Achieving this goal requires recognising that de-prescribing is easier said than done, but it can be accomplished successfully with appropriate support and systematic approaches.
Success in de-prescribing implementation will require continued collaboration between researchers, clinicians, policymakers, and patients to develop and implement evidence-based strategies that address the complex barriers identified in this analysis. The stakes are high—the health and well-being of ageing populations worldwide depend on our ability to move beyond the recognition that “less is more” to the actual implementation of this principle in clinical practice.
References
Ailabouni, N. J., Weir, K. R., Reeve, E., Turner, J. T., Norton, J. W., & Gray, S. L. (2022). Barriers and enablers of older adults initiating a deprescribing conversation. Patient Education and Counselling, 105(3), 615-624.
Alharthi, M., Wright, D., Scott, S., & Birt, L. (2023). Barriers and enablers to deprescribing for older people in care homes: The theory-based perspectives of pharmacist independent prescribers. Exploratory Research in Clinical and Social Pharmacy, 11, 100294.
Bloomfield, H. E., Greer, N., Linsky, A. M., Bolduc, J., Naidl, T., Vardeny, O., MacDonald, R., McKenzie, L., & Wilt, T. J. (2020). Deprescribing for Community-Dwelling Older Adults: A Systematic Review and Meta-analysis. Journal of General Internal Medicine, 35(11), 3323-3332.
Carollo, M., Crisafulli, S., Vitturi, G., Besco, M., Hinek, D., Sartorio, A., Tanara, V., Spadacini, G., Selleri, M., Zanconato, V., Fava, C., Minuz, P., Zamboni, M., & Trifirò, G. (2024). Clinical impact of medication review and deprescribing in older inpatients: A systematic review and meta-analysis. Journal of the American Geriatrics Society, 72(10), 3219-3238.
Chock, Y. L., Wee, Y. L., Gan, S. L., Teoh, K. W., Ng, K. Y., & Lee, S. W. H. (2021). How Willing Are Patients or Their Caregivers to Deprescribe: a Systematic Review and Meta-analysis. Journal of General Internal Medicine, 36(12), 3830-3840.
Chua, S., Todd, A., Reeve, E., Smith, S. M., Fox, J., Elsisi, Z., Hughes, S., Husband, A., Langford, A., Merriman, N., Harris, J. R., Devine, B., & Gray, S. L. (2024). Deprescribing interventions in older adults: An overview of systematic reviews. PLOS ONE, 19(6), e0305215.
Cullinan, S., Raae Hansen, C., Byrne, S., O’Mahony, D., Kearney, P., & Sahm, L. (2017). Challenges of deprescribing in the multimorbid patient. European Journal of Hospital Pharmacy, 24(1), 43-46.
Frohnhofen, H., Michalek, C., & Wehling, M. (2013). Less is more – how to prevent polypharmacy? Deutsche Medizinische Wochenschrift, 138(3), 99-103.
Gadisa, D. A., Gebremariam, E. T., Yimer, G., & Deresa Urgesa, E. (2023). Attitudes of Older Adult Patients and Caregivers Towards Deprescribing of Medications in Ethiopia. Clinical Interventions in Ageing, 18, 1129-1143.
Green, A. R., Aschmann, H., Boyd, C. M., & Schoenborn, N. (2021). Assessment of Patient-Preferred Language to Achieve Goal-Aligned Deprescribing in Older Adults. JAMA Network Open, 4(4), e212633.
Heinrich, C. H., McHugh, S., McCarthy, S., & Donovan, M. D. (2022). Barriers and enablers to deprescribing in long-term care: A qualitative investigation into the opinions of healthcare professionals in Ireland. PLOS ONE, 17(12), e0274552.
Hollingsworth, E. K., Erickson, S. R., Rosenthal, M., Farris, K., Mather, J., Doucette, W., Stultz, J., Moga, D., Jameson, J. P., Blalock, S., Ferreri, S., Patel, N., Margolis, A., Rodebaugh, T., Herges, E., Brandt, N., & Steinman, M. A. (2022). Implementation considerations of deprescribing interventions: A scoping review. Journal of the American Geriatrics Society, 70(11), 3174-3195.
Japelj, N., Knez, L., Petek, D., & Horvat, N. (2024). Improving the feasibility of deprescribing proton pump inhibitors: GPs’ insights on barriers, facilitators, and strategies. Frontiers in Pharmacology, 15, 1468750.
Langford, A. V., Schneider, C. R., Reeve, E., & Gnjidic, D. (2024). Minimising Harm and Managing Pain: Deprescribing Opioids in Older Adults. Drugs & Ageing, 41(11), 863-871.
Linsky, A., Gellad, W. F., Linder, J. A., & Friedberg, M. W. (2019). Advancing the Science of Deprescribing: A Novel Comprehensive Conceptual Framework. Journal of the American Geriatrics Society, 67(10), 2018-2022.
Oktora, M. P., Yuniar, C. T., Amalia, L., Abdulah, R., Hak, E., & Denig, P. (2023). Attitudes towards deprescribing and patient-related factors associated with willingness to stop medication among older patients with type 2 diabetes (T2D) in Indonesia: a cross-sectional survey study. BMC Geriatrics, 23(1), 21.
Omuya, H., Nickel, C., Wilson, P., & Chewning, B. (2023). A systematic review of randomized-controlled trials on deprescribing outcomes in older adults with polypharmacy. International Journal of Pharmacy Practice, 31(4), 349-368.
Page, A. T., Potter, K., Clifford, R., & Etherton-Beer, C. (2016). Deprescribing in older people. Maturitas, 91, 115-134.
Pereira, A., Veríssimo, M., & Ribeiro, O. (2024). Predictors of older patients’ willingness to have medications deprescribed: A cross-sectional study. International Journal of Clinical Pharmacy, 46(3), 703-712.
Reeve, E., & Kouladjian O’Donnell, L. (2021). Deprescribing: Moving beyond barriers and facilitators. Exploratory Research in Clinical and Social Pharmacy, 4, 100073.
Reeve, E., Low, L. F., & Hilmer, S. N. (2019). Attitudes of Older Adults and Caregivers in Australia toward Deprescribing. Journal of the American Geriatrics Society, 67(6), 1204-1210.
Reeve, E., To, J., Hendrix, I., Shakib, S., Roberts, M. S., & Wiese, M. D. (2013). Patient barriers to and enablers of deprescribing: a systematic review. Drugs & Ageing, 30(10), 793-807.
Rochon, P. A., Petrovic, M., Cherubini, A., Onder, G., O’Mahony, D., Sternberg, S. A., Stall, N. M., & Gurwitz, J. H. (2021). Polypharmacy, inappropriate prescribing, and deprescribing in older people: through a sex and gender lens. The Lancet Healthy Longevity, 2(5), e290-e300.
Saka, S. A., & Osineye, T. R. (2024). Considerations, barriers, and enablers of deprescribing among healthcare professionals in Ogun State, Southwest, Nigeria: a cross-sectional survey. BMC Health Services Research, 24(1), 661.
Scott, I. A., Hilmer, S. N., Reeve, E., Potter, K., Le Couteur, D., Rigby, D., Gnjidic, D., Del Mar, C. B., Roughead, E. E., Page, A., Jansen, J., & Martin, J. H. (2015). Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Internal Medicine, 175(5), 827-834.
Tangiisuran, B., Rajendran, V., Sha’aban, A., Daud, N. A. A., & Nawi, S. N. M. (2022). Physicians’ perceived barriers and enablers for deprescribing among older patients at public primary care clinics: a qualitative study. International Journal of Clinical Pharmacy, 44(1), 201-213.
Thillainadesan, J., Gnjidic, D., Green, S., & Hilmer, S. N. (2018). Impact of Deprescribing Interventions in Older Hospitalised Patients on Prescribing and Clinical Outcomes: A Systematic Review of Randomised Trials. Drugs & Ageing, 35(4), 303-319.
Turner, J. P., Sanyal, C., Martin, P., & Tannenbaum, C. (2020). Economic Evaluation of Sedative Deprescribing in Older Adults by Community Pharmacists. The Journals of Gerontology: Series A, 75(9), 1736-1743.
Vasilevskis, E. E., Hollingsworth, E. K., Mixon, A. S., Kripalani, S., & Simmons, S. F. (2022). Deprescribing Medications Among Older Adults From End of Hospitalization Through Postacute Care: A Shed-MEDS Randomized Clinical Trial. JAMA Internal Medicine, 183(3), 223-231.
Weir, K. R., Ailabouni, N. J., Schneider, C. R., Hilmer, S. N., & Reeve, E. (2022). Consumer Attitudes Towards Deprescribing: A Systematic Review and Meta-Analysis. The Journals of Gerontology: Series A, 77(5), 1020-1034.
Wu, H., Kouladjian O’Donnell, L., Fujita, K., Masnoon, N., & Hilmer, S. N. (2021). Deprescribing in the Older Patient: A Narrative Review of Challenges and Solutions. International Journal of General Medicine, 14, 3793-3807.
Zhou, D., Chen, Z., & Tian, F. (2023). Deprescribing Interventions for Older Patients: A Systematic Review and Meta-Analysis. Journal of the American Medical Directors Association, 24(11), 1718-1725.
References
[1] Barriers and enablers to deprescribing of older adults and their caregivers: a systematic review and meta-synthesis – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37874489/
[2] Deprescribing in older adults with polypharmacy – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/38719530/
[3] Deprescribing: Moving beyond barriers and facilitators – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S1551741121001273
[4] Polypharmacy and deprescribing – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S1357303923002438
[5] Polypharmacy and deprescribing – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S1357303923002438
[6] Polypharmacy and Deprescribing in Older Adults – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37729029/
[7] Informatics Tools in Deprescribing and Medication Optimisation in Older Adults: Development and Dissemination of VIONE Methodology in a High Reliability Organisation – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S0149291823002965
[8] Polypharmacy and Deprescribing in Older Adults – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37729029/
[9] A narrative review of evidence to guide deprescribing among older adults – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/34221792/
[10] Predictors of older patients’ willingness to have medications deprescribed: A cross-sectional study – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37070165/
[11] Predictors of older patients’ willingness to have medications deprescribed: A cross-sectional study – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37070165/
[12] A systematic review of randomized-controlled trials on deprescribing outcomes in older adults with polypharmacy – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37155330/
[13] Deprescribing Interventions for Older Patients: A Systematic Review and Meta-Analysis – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37582482/
[14] Deprescribing Interventions for Older Patients: A Systematic Review and Meta-Analysis – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37582482/
[15] Deprescribing: Moving beyond barriers and facilitators – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S1551741121001273
[16] Deprescribing: Moving beyond barriers and facilitators – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S1551741121001273
[17] Deprescribing: Moving beyond barriers and facilitators – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S1551741121001273
[18] Deprescribing: Moving beyond barriers and facilitators – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S1551741121001273
[19] Deprescribing: Moving beyond barriers and facilitators – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S1551741121001273
[20] Barriers and enablers to deprescribing for older people in care homes: The theory-based perspectives of pharmacist independent prescribers – ScienceDirect –
https://www.sciencedirect.com/science/article/pii/S1551741123000335
[21] Barriers and enablers to deprescribing for older people in care homes: The theory-based perspectives of pharmacist independent prescribers – ScienceDirect –
https://www.sciencedirect.com/science/article/pii/S1551741123000335
[22] Challenges and Successes of Global Deprescribing Networks: A Qualitative Key Informant Study – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/34978496/
[23] Barriers and enablers of older adults initiating a deprescribing conversation – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S0738399121004201
[24] Barriers and enablers to deprescribing for older people in care homes: The theory-based perspectives of pharmacist independent prescribers – ScienceDirect –
https://www.sciencedirect.com/science/article/pii/S1551741123000335
[25] Knowledge and willingness of physicians about deprescribing among older patients: a qualitative study – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/30122912/
[26] Deprescribing tools and guidelines in chronic kidney disease: A scoping review – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S155174112500244X
[27] Barriers and enablers of older adults initiating a deprescribing conversation – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S0738399121004201
[28] Barriers and enablers to deprescribing for older people in care homes: The theory-based perspectives of pharmacist independent prescribers – ScienceDirect –
https://www.sciencedirect.com/science/article/pii/S1551741123000335
[29] Older patients’ perception of deprescribing in resource-limited settings: a cross-sectional study in an Ethiopian university hospital – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/29678983/
[30] Informatics Tools in Deprescribing and Medication Optimisation in Older Adults: Development and Dissemination of VIONE Methodology in a High Reliability Organisation – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S0149291823002965
[31] Informatics Tools in Deprescribing and Medication Optimisation in Older Adults: Development and Dissemination of VIONE Methodology in a High Reliability Organisation – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S0149291823002965
[32] Informatics Tools in Deprescribing and Medication Optimisation in Older Adults: Development and Dissemination of VIONE Methodology in a High Reliability Organisation – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S0149291823002965
[33] Barriers and enablers of older adults initiating a deprescribing conversation – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S0738399121004201
[34] Barriers and enablers of older adults initiating a deprescribing conversation – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S0738399121004201
[35] Deprescribing tools and guidelines in chronic kidney disease: A scoping review – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S155174112500244X
[36] Deprescribing tools and guidelines in chronic kidney disease: A scoping review – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S155174112500244X
[37] Beliefs and attitudes of older adults and carers about deprescribing of medications: a qualitative focus group study – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/27266865/
[38] Attitudes towards deprescribing and patient-related factors associated with willingness to stop medication among older patients with type 2 diabetes (T2D) in Indonesia: a cross-sectional survey study – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/36635653/
[39] Attitudes towards deprescribing and patient-related factors associated with willingness to stop medication among older patients with type 2 diabetes (T2D) in Indonesia: a cross-sectional survey study – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/36635653/
[40] Barriers and enablers to deprescribing for older people in care homes: The theory-based perspectives of pharmacist independent prescribers – ScienceDirect –
https://www.sciencedirect.com/science/article/pii/S1551741123000335
[41] Exploring the need for a clinical decision support system for deprescribing – A qualitative interview study – ScienceDirect –
https://www.sciencedirect.com/science/article/pii/S2667276625000150
[42] Exploring the need for a clinical decision support system for deprescribing – A qualitative interview study – ScienceDirect –
https://www.sciencedirect.com/science/article/pii/S2667276625000150
[43] What do clinical practice guidelines say about deprescribing? A scoping review – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/38789258/
[44] Challenges and Successes of Global Deprescribing Networks: A Qualitative Key Informant Study – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/34978496/
[45] Challenges of deprescribing in the multimorbid patient – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/31156897/
[46] Challenges and Successes of Global Deprescribing Networks: A Qualitative Key Informant Study – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/34978496/
[47] Deprescribing: Moving beyond barriers and facilitators – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S1551741121001273
[48] Clinical practice guideline for deprescribing opioid analgesics: summary of recommendations – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37356051/
[49] Clinical practice guideline for deprescribing opioid analgesics: summary of recommendations – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37356051/
[50] Development and Validation of Nine Deprescribing Algorithms for Patients on Hemodialysis to Decrease Polypharmacy – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/33194213/
[51] Development and Validation of Nine Deprescribing Algorithms for Patients on Hemodialysis to Decrease Polypharmacy – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/33194213/
[52] Development and Validation of Nine Deprescribing Algorithms for Patients on Hemodialysis to Decrease Polypharmacy – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/33194213/
[53] Deprescribing tools and guidelines in chronic kidney disease: A scoping review – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/40368718/
[54] Implementation considerations of deprescribing interventions: A scoping review – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/36524602/
[55] Advancing the Science of Deprescribing: A Novel Comprehensive Conceptual Framework – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/31430394/
[56] Informatics Tools in Deprescribing and Medication Optimisation in Older Adults: Development and Dissemination of VIONE Methodology in a High Reliability Organisation – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S0149291823002965
[57] Deprescribing for Community-Dwelling Older Adults: a Systematic Review and Meta-analysis – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/32820421/
[58] Predictors of older patients’ willingness to have medications deprescribed: A cross-sectional study – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37070165/
[59] Deprescribing Interventions for Older Patients: A Systematic Review and Meta-Analysis – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37582482/
[60] Barriers and enablers of older adults initiating a deprescribing conversation – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/34183219/
[61] Barriers and enablers of older adults initiating a deprescribing conversation – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/34183219/
[62] Older Patient and Surrogate Attitudes Toward Deprescribing During the Transition From Acute to Post-Acute Care – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/35164584/
[63] Willingness of older people living with dementia and mild cognitive impairment and their caregivers to have medications deprescribed – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/36702513/
[64] Willingness of older people living with dementia and mild cognitive impairment and their caregivers to have medications deprescribed – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/36702513/
[65] Polypharmacy and Deprescribing in Older Adults – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37729029/
[66] Polypharmacy and Deprescribing in Older Adults – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37729029/
[67] Barriers to Optimising Prescribing and Deprescribing in Older Adults with Dementia: A Narrative Review – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/26338170/
[68] Barriers to Optimising Prescribing and Deprescribing in Older Adults with Dementia: A Narrative Review – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/26338170/
[69] Barriers to Optimising Prescribing and Deprescribing in Older Adults with Dementia: A Narrative Review – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/26338170/
[70] Clinical practice guideline for deprescribing opioid analgesics: summary of recommendations – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37356051/
[71] Deprescribing tools and guidelines in chronic kidney disease: A scoping review – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/40368718/
[72] Older patients’ perception of deprescribing in resource-limited settings: a cross-sectional study in an Ethiopian university hospital – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/29678983/
[73] Deprescribing: A narrative review of the evidence and practical recommendations for recognising opportunities and taking action – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S0953620516304502
[74] Older Patient and Surrogate Attitudes Toward Deprescribing During the Transition From Acute to Post-Acute Care – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/35164584/
[75] Association between willingness to deprescribe and health outcome priorities among U.S. older adults: Results of a national survey – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/35661991/
[76] Attitudes of Older Adults and Caregivers in Australia toward Deprescribing – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/30756387/
[77] Attitudes of Older Adults and Caregivers in Australia toward Deprescribing – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/30756387/
[78] Using the behaviour change wheel to link published deprescribing strategies to identified local primary healthcare needs – ScienceDirect –
https://www.sciencedirect.com/science/article/abs/pii/S1551741121003867
[79] Attitudes towards deprescribing and patient-related factors associated with willingness to stop medication among older patients with type 2 diabetes (T2D) in Indonesia: a cross-sectional survey study – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/36635653/
[80] Clinical practice guideline for deprescribing opioid analgesics: summary of recommendations – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/37356051/
[81] Attitudes of Older Adults and Caregivers in Australia toward Deprescribing – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/30756387/
[82] Development and Validation of Nine Deprescribing Algorithms for Patients on Hemodialysis to Decrease Polypharmacy – PubMed – pubmed.ncbi.nlm.nih.gov
https://pubmed.ncbi.nlm.nih.gov/33194213/
[83] Deprescribing Interventions for Older Patients: A Systematic Review and Meta-Analysis – ScienceDirect –https://www.sciencedirect.com/science/article/abs/pii/S152586102300645X

