Bioidentical Hormone Replacement Therapy (HRT) – Paradigm Shift
Please like and subscribe if you enjoyed this video 🙂
Introduction
Hormone replacement therapy (HRT) has been a subject of significant debate and research in recent years, particularly concerning its use in postmenopausal women. As our understanding of hormonal changes during menopause and their impact on women’s health evolves, so too do the treatment guidelines for HRT. This article aims to provide healthcare professionals with an up-to-date overview of the latest treatment guidelines for HRT, focusing on the use of bioidentical hormones in postmenopausal women. We will also explore common symptoms of menopause and discuss the rationale for avoiding conjugated estrogens and medroxyprogesterone in favor of more personalized approaches.
Understanding Menopause and Its Impact
Defining Menopause
Menopause is a natural biological process marking the end of a woman’s reproductive years. It is clinically defined as the cessation of menstruation for 12 consecutive months, typically occurring between the ages of 45 and 55. The transition to menopause, known as perimenopause, can last several years and is characterized by fluctuating hormone levels, particularly estrogen and progesterone.
Hormonal Changes During Menopause
During menopause, the ovaries gradually produce less estrogen and progesterone. This decline in hormone production leads to various physiological changes throughout the body, affecting multiple organ systems and often resulting in a range of symptoms that can significantly impact a woman’s quality of life.
Common Symptoms of Menopause
Vasomotor Symptoms
Hot Flashes and Night Sweats
Hot flashes and night sweats are among the most common and bothersome symptoms of menopause. These sudden feelings of intense heat, often accompanied by sweating and flushing, can occur during the day or night, disrupting sleep and daily activities. It is estimated that up to 80% of menopausal women experience vasomotor symptoms to some degree.
Genitourinary Symptoms
Vaginal Dryness and Atrophy
The decline in estrogen levels during menopause can lead to thinning and drying of the vaginal tissues, resulting in discomfort, itching, and pain during intercourse. This condition, known as vaginal atrophy or genitourinary syndrome of menopause (GSM), affects up to 50% of postmenopausal women.
Urinary Incontinence
Weakening of the pelvic floor muscles and changes in urethral tissue can lead to various urinary symptoms, including increased frequency, urgency, and stress incontinence.
Psychological Symptoms
Mood Changes and Depression
Hormonal fluctuations during menopause can contribute to mood swings, irritability, and an increased risk of depression. These psychological symptoms can significantly impact a woman’s overall well-being and quality of life.
Cognitive Changes
Some women report difficulties with memory and concentration during the menopausal transition, often referred to as “brain fog.” While the exact relationship between menopause and cognitive function is still being studied, these symptoms can be distressing for many women.
Musculoskeletal Changes
Osteoporosis Risk
The decline in estrogen levels during menopause accelerates bone loss, increasing the risk of osteoporosis and fractures. This is a significant health concern for postmenopausal women and a key consideration in HRT decision-making.
Joint Pain
Some women experience increased joint pain and stiffness during menopause, which may be related to hormonal changes and the natural aging process.
Cardiovascular Health
Changes in Lipid Profile
Menopause is associated with changes in lipid metabolism, often leading to an increase in LDL cholesterol and a decrease in HDL cholesterol. These changes can contribute to an increased risk of cardiovascular disease in postmenopausal women.
Endothelial Function
Estrogen plays a role in maintaining healthy blood vessel function. The decline in estrogen levels during menopause may contribute to changes in endothelial function and an increased risk of hypertension and cardiovascular events.

Evolution of Hormone Replacement Therapy
Historical Perspective
Hormone replacement therapy has been used for decades to alleviate menopausal symptoms and address long-term health risks associated with estrogen deficiency. However, the approach to HRT has evolved significantly over time, influenced by large-scale clinical trials and ongoing research.
The Women’s Health Initiative (WHI) Impact
The publication of the Women’s Health Initiative (WHI) study results in 2002 led to a dramatic shift in HRT prescribing practices. The study raised concerns about the risks associated with long-term use of conjugated equine estrogens and medroxyprogesterone acetate, particularly in terms of breast cancer and cardiovascular events.
Paradigm Shift: Individualized Approach
In the years following the WHI study, there has been a growing recognition of the need for a more personalized approach to HRT. This shift has led to increased interest in bioidentical hormones and tailored treatment regimens based on individual patient factors and preferences.
Latest Treatment Guidelines for HRT Using Bioidentical Hormones
Defining Bioidentical Hormones
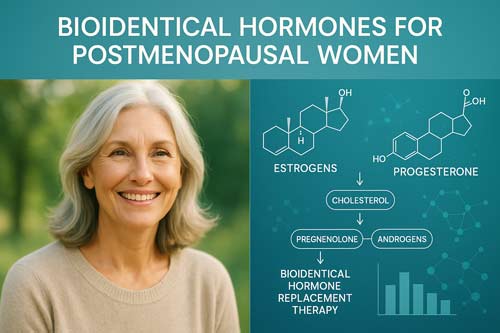
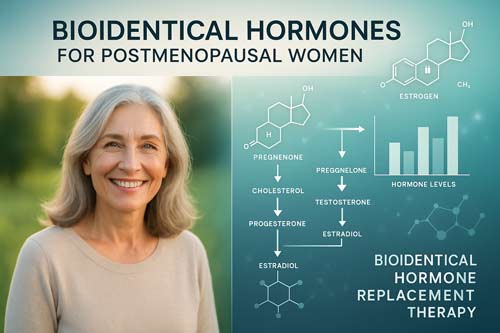
Molecular Structure and Function
Bioidentical hormones are compounds that have the same molecular structure as hormones naturally produced in the human body. In the context of HRT, this typically refers to 17β-estradiol, estrone, estriol, and progesterone. These hormones are designed to interact with hormone receptors in the same way as endogenous hormones, potentially offering a more physiological approach to hormone replacement.
Sources and Formulations
Bioidentical hormones can be derived from plant sources (e.g., soy or yam) and are chemically modified to match human hormones. They are available in various formulations, including oral tablets, transdermal patches, gels, creams, and vaginal preparations.
Current Guidelines for Bioidentical HRT
Indications for Treatment
Vasomotor Symptom Management
The primary indication for systemic HRT remains the management of moderate to severe vasomotor symptoms. Bioidentical estradiol, alone or in combination with bioidentical progesterone (for women with an intact uterus), is considered an effective option for alleviating hot flashes and night sweats.
Genitourinary Symptom Relief
For women experiencing vaginal dryness and atrophy, low-dose vaginal estrogen preparations, including bioidentical estradiol, are recommended as first-line therapy. These local treatments can effectively address genitourinary symptoms with minimal systemic absorption.
Bone Health Preservation
HRT, including bioidentical formulations, remains an approved option for the prevention of osteoporosis in postmenopausal women at high risk of fracture who cannot tolerate other bone-specific treatments.
Dosing and Administration
Estrogen Dosing
The current recommendation is to use the lowest effective dose of estrogen for symptom relief. For systemic therapy, typical starting doses of transdermal estradiol range from 0.025 to 0.05 mg/day, with oral estradiol typically starting at 0.5 to 1 mg/day.
Progesterone Use
For women with an intact uterus, progesterone must be used in combination with estrogen to protect against endometrial hyperplasia and cancer. Bioidentical micronized progesterone is typically prescribed at 100-200 mg/day orally or 20-40 mg/day transdermally.
Route of Administration
Transdermal administration of estradiol is often preferred due to its more favorable pharmacokinetic profile, bypassing first-pass liver metabolism and potentially reducing the risk of venous thromboembolism compared to oral formulations.
Duration of Treatment
Individualized Approach
The duration of HRT should be individualized based on the treatment goals, ongoing symptom burden, and the patient’s overall health profile. The concept of the “lowest effective dose for the shortest duration” has been replaced by a more nuanced approach that considers the benefits and risks for each individual patient.
Regular Reassessment
Guidelines recommend regular reassessment of the need for continued HRT, typically on an annual basis. This allows for adjustment of the treatment regimen as needed and ensures that the benefits continue to outweigh any potential risks.

Benefits of Bioidentical HRT
Symptom Relief
Vasomotor Symptom Improvement
Bioidentical estradiol has been shown to be highly effective in reducing the frequency and severity of hot flashes and night sweats, with many women experiencing significant relief within a few weeks of starting treatment.
Enhancement of Vaginal Health
Both systemic and local bioidentical estrogen preparations can significantly improve vaginal dryness, atrophy, and associated symptoms, enhancing sexual function and quality of life.
Long-term Health Benefits
Bone Density Preservation
HRT, including bioidentical formulations, has been consistently shown to maintain bone mineral density and reduce the risk of osteoporotic fractures in postmenopausal women.
Potential Cardiovascular Benefits
Some studies suggest that initiating HRT close to the onset of menopause may have cardioprotective effects, particularly when using transdermal estradiol. However, this remains an area of ongoing research and debate.
Risks and Considerations
Breast Cancer Risk
The relationship between HRT and breast cancer risk remains complex. While the WHI study showed an increased risk with combined estrogen-progestin therapy, subsequent analyses and studies have suggested that the risk may be lower with bioidentical progesterone compared to synthetic progestins.
Venous Thromboembolism
The risk of venous thromboembolism (VTE) is a key consideration in HRT. Transdermal estradiol appears to carry a lower VTE risk compared to oral formulations, particularly in women with risk factors such as obesity or a history of VTE.
Endometrial Safety
For women with an intact uterus, the use of estrogen must always be balanced with adequate progestogen to protect against endometrial hyperplasia and cancer. Bioidentical micronized progesterone has shown favorable endometrial protection when used appropriately.
Avoiding Conjugated Estrogens and Medroxyprogesterone
Rationale for Shifting Away from Traditional HRT
Conjugated Estrogens
Conjugated estrogens, particularly those derived from pregnant mare’s urine, contain a mixture of estrogen compounds, some of which are not naturally found in humans. This complex composition makes it challenging to predict individual responses and may contribute to unwanted side effects.
Medroxyprogesterone Acetate
Medroxyprogesterone acetate, a synthetic progestin, has been associated with a higher risk of breast cancer and potentially adverse cardiovascular effects compared to bioidentical progesterone.
Advantages of Bioidentical Hormones
Molecular Precision
Bioidentical hormones offer a more targeted approach, allowing for precise dosing of specific hormones that are structurally identical to those produced by the human body.
Potential for Reduced Side Effects
Some studies suggest that bioidentical hormones, particularly when administered transdermally, may have a more favorable side effect profile compared to traditional HRT formulations.
Customization Options
The use of bioidentical hormones allows for greater flexibility in tailoring treatment regimens to individual patient needs, potentially optimizing efficacy while minimizing risks.
Personalizing HRT: A Patient-Centered Approach
Comprehensive Assessment
Medical History and Risk Factors
A thorough evaluation of the patient’s medical history, family history, and personal risk factors is essential for determining the appropriateness of HRT and selecting the optimal treatment regimen.
Symptom Evaluation
Careful assessment of menopausal symptoms, their severity, and impact on quality of life helps guide treatment decisions and allows for targeted symptom management.
Shared Decision-Making
Patient Preferences and Values
Engaging patients in the decision-making process, considering their preferences, concerns, and treatment goals, is crucial for ensuring adherence and satisfaction with HRT.
Risk-Benefit Discussion
Healthcare providers should engage in a comprehensive discussion of the potential benefits and risks of HRT, tailored to the individual patient’s health profile and circumstances.
Monitoring and Follow-up
Regular Clinical Evaluation
Ongoing monitoring of treatment response, side effects, and overall health status is essential for optimizing HRT outcomes and ensuring patient safety.
Adjusting Treatment as Needed
Flexibility in modifying the HRT regimen based on clinical response and changing patient needs is a key aspect of personalized care.
Emerging Trends and Future Directions
Advances in Hormone Delivery Systems
Novel Transdermal Technologies
Ongoing research into improved transdermal delivery systems may offer enhanced absorption and more stable hormone levels, potentially improving efficacy and reducing side effects.
Targeted Tissue Delivery
Development of hormone formulations that target specific tissues (e.g., bone or brain) while minimizing systemic exposure is an area of active investigation.
Precision Medicine Approaches
Genetic Testing and Pharmacogenomics
Emerging research in pharmacogenomics may allow for more precise prediction of individual responses to HRT, enabling truly personalized treatment strategies.
Biomarker-Guided Therapy
Identification and validation of biomarkers for HRT response and risk assessment could further refine treatment selection and monitoring.

Conclusion
The landscape of hormone replacement therapy for postmenopausal women continues to evolve, with a growing emphasis on personalized care and the use of bioidentical hormones. Current guidelines advocate for an individualized approach to HRT, considering the unique symptoms, risk factors, and preferences of each patient. The shift towards bioidentical hormones and away from conjugated estrogens and medroxyprogesterone reflects a broader trend towards more physiological and targeted hormone replacement strategies.
As healthcare professionals, it is crucial to stay informed about the latest evidence and guidelines for HRT while maintaining a patient-centered approach to care. By carefully weighing the benefits and risks, engaging in shared decision-making, and providing ongoing monitoring and support, we can help postmenopausal women navigate the complexities of HRT and achieve optimal health outcomes.
The future of HRT holds promise for even more refined and personalized treatment options, potentially leveraging advances in genetics, biomarker research, and drug delivery technologies. As we continue to expand our understanding of menopause and hormonal health, the goal remains to provide safe, effective, and individualized care that enhances the quality of life for postmenopausal women.
References:
-
The 2022 Hormone Therapy Position Statement of The North American Menopause Society. Menopause. 2022;29(7):734–760.
-
Stuenkel CA, Davis SR, Gompel A, et al.; Endocrine Society. Treatment of Symptoms of the Menopause: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2020;105(11):3853–3853.
-
American College of Obstetricians and Gynecologists. Hormone Therapy for Menopause. ACOG Practice Bulletin. 2023.
-
American College of Obstetricians and Gynecologists. Compounded Bioidentical Menopausal Hormone Therapy: Clinical Consensus. Obstet Gynecol. 2023;142(5):e50–e61.
-
International Menopause Society. Menopause and MHT in 2024: Addressing the Key Controversies—2024 White Paper. IMS; 2024.
-
National Institute for Health and Care Excellence. Menopause: Identification and Management (NG23). NICE; November 2024.
-
European Menopause and Andropause Society. EMAS Guidelines for the Management of Menopause. EMAS; 2024.
-
British Menopause Society. Commentary on the 2024 NICE Menopause Guideline (NG23). Br Menopause Soc; 2024.
-
Carr L. New Hormone Therapy Guidelines from The North American Menopause Society. Contemp Ob Gyn. July 2022.
-
Rahn DD, Laughlin-Tommaso SK. Rethinking Menopausal Hormone Therapy: For Whom, What, When. Menopause. 2023;30(4):463–472.
-
Boniface DR, et al. Compounded Bioidentical Hormone Preparations. In: NCBI Bookshelf, NBK562866. Overview of cBHT formulations and compounding standards.
-
The British Menopause Society & Women’s Health Concern. Consensus Statement on HRT Recommendations, September 2023. Updated guidance on bioidentical and traditional HRT regimens.
-
Society for Endocrinology. Joint Position Statement on Best‑Practice Recommendations for the Care of Women Experiencing the Menopause, The Endocrinologist, Summer 2022.