Methadone Treatment: Initiation and Titration
David McAuley, Pharm.D., R.Ph.
“Deaths, cardiac and respiratory, have been reported during initiation and conversion of pain patients to methadone treatment from treatment with other opioid agonists. It is critical to understand the pharmacokinetics of methadone when converting patients from other opioids. During methadone treatment, particular vigilance is necessary during treatment initiation, during conversion from one opioid to another, and during dose titration.” (Source: black box warning – package insert)
Protocol for Opioid-Naive Patients – ‘Start low, go Slow’:
Note: preferred titration doses and intervals are indicated by bold print.
| Week 1: |
Dose: Methadone 2.5 mg q8h or q12h |
Total daily dose: 5 to 7.5 mg |
| Week 2: |
Dose: Methadone 5 mg q8h or q12h |
Total daily dose: 10 to 15 mg |
| Week 3: |
Dose: Methadone 7.5 mg q8h or q12h |
Total daily dose: 15 to 22.5 mg |
| Week 4: |
Dose: Methadone 10 mg q8h or q12h |
Total daily dose: 20 to 30 mg |
| Week 5: |
Dose: Methadone 10 mg q6h or q8h |
Total daily dose: 30 to 40 mg |
| Week 6: |
Continue slow titration if adequate analgesia still not achieved. |
Important Points:
- Consider much lower initial doses in the following patients undergoing methadone treatment (e.g. 2.5 mg orally q12 to 24h):
- Frail or elderly patients (decreased methadone clearance).
- Patients receiving other sedative drugs, including alcohol and benzodiazepines. (Potentiation of CNS depression.)
- Patients with severe COPD, acute asthma, or respiratory depression. [Consider avoiding methadone]
- Presence of Interacting medications (reduced clearance of methadone): Examples: Cimetidine, Ciprofloxacin, Fluconazole, Fluvoxamine, MAOIs, TCAs, Other. Methadone is primarily metabolized by the cytochrome P450 liver isoenzyme CYP34A and induction or inhibition of this enzyme is the mechanism behind many of methadone’s drug interactions.
- Patients with liver, renal, or pulmonary disease.
- Frail or debilitated patients.
- Acceptable guidelines for methadone titration are lacking, so increases should be based on the patient’s response.
- Generally, weekly regimen increases should be limited to an increase of 2.5 mg per dose (q5-7 days).
- If a patient has adequate pain relief at any step, further dosage increases should be immediately halted.
- If tolerable pain relief is not achieved at a particular step, consider increasing the dosage frequency (q12h –> q8h –> q6h)
- Consider alternative treatments for patients who cannot be adequately monitored at home (especially during the initial titration period).
- If a patient develops sedation (respiratory depression may follow), hold or decrease the following dose of methadone and decrease subsequent doses and/or make dosage increments less frequently. Do not increase the dose of methadone.
- Several days (usually 5 to 7) are required to reach steady-state plasma levels, so monitoring during methadone treatment should continue after the last dosage increase to detect potential overdose.
- VAPBM: If a practitioner or consultant with experience in using methadone for chronic pain is not available, consider using another long-duration opioid until such consultation can be obtained.
Current support for above protocol – Methadone initiation in non-tolerant patients:
- College of Physicians and Surgeons of : Methadone starting dose: 2.5 mg po every 8 hours. Titrate q5-7 days.
- Package Insert: usual oral methadone starting dose is 2.5 mg to 10 mg every 8 to 12 hours, slowly titrated to effect….. Extreme caution is necessary to avoid overdosage, taking into account methadone’s long elimination half-life.
- VA/DoD Clinical Practice Guidelines: Starting dose: 2.5 mg po every 8 hours. Titrate every 5 to 7 days. (May consider increases in dosing frequency (q6h) for cancer pain and situations where frequent monitoring is possible)
- Toombs JD. Methadone treatment for pain states. Am Fam Physician – 1-APR-2005; 71(7): 1353-8: (Repeats CPSO’s position): In an opioid-naïve patient, the recommended starting dosage is 2.5 mg orally every eight hours. In frail older patients, the starting dosage may need to be as low as 2.5 mg orally once per day. In the outpatient setting, incremental increases may be made every five to seven days, depending on the patient’s response.
Patient Education
- Explain to patients that the degree of pain relief from methadone will increase throughout the week after each dosage increase as the drug level reaches steady state.
- Explain that it may take several weeks to reach the correct maintenance dose. The initial dose will often be inadequate for pain relief. (A pain medicine diary should be kept.) Reassure patients that the dose will be titrated to achieve adequate analgesia.
- Remind patients undergoing methadone treatment about the need for and the frequency of monitoring during the titration and maintenance periods. Ideally, patients should be seen every few days and before any dosage increases.
- Patients should be instructed to immediately contact the provider if they develop increasing or intolerable adverse effects.
- Advise patients to avoid abrupt discontinuation of methadone or other opioids without first consulting their physician. Educate patients about withdrawal symptoms.
Methadone is NOT a first line drug – Possible Indications:
- Morphine allergy
- Neuropathic pain
- Intolerable adverse effects with other opioids
- Pain refractory to other opioids
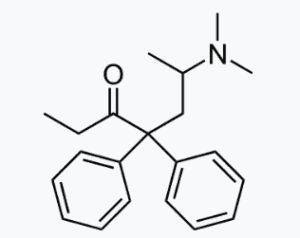
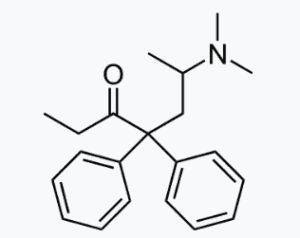
Support: Methadone’s delta receptor activity makes it a sensible switch to regain analgesia following tolerance to a mu agonist. Methadone is a potent NMDA receptor antagonist which may explain the advantage that methadone has over morphine or fentanyl in neuropathic pain. Methadone does not have any known active metabolites – it has been suggested that the accumulation of active metabolites may be the reason that some patients do not respond to morphine or experience CNS side effects.
Safety Guidelines Issued for Prescribing Methadone
Subject: The Center for Substance Abuse Treatment (CSAT) convened a Cardiac Expert Panel that issued safety recommendations regarding arrhythmia risk and rate-corrected QT interval (QTc) interval monitoring for clinicians prescribing methadone.
The panel issued the following specific recommendations in 5 key clinical areas:
- Recommendation 1 (Disclosure): When clinicians prescribe methadone, they should inform patients about arrhythmia risk.
- Recommendation 2 (Clinical History): Clinicians should ask patients about any history of structural heart disease, arrhythmia, or syncope.
- Recommendation 3 (Screening): All patients should have a pretreatment electrocardiogram (ECG) to measure QTc interval and a follow-up ECG within 30 days and each year. If the methadone dosage is greater than 100 mg/day, or if patients have unexplained syncope or seizures, additional ECG is recommended.
- Screening with ECG may also be done as indicated for patients receiving methadone who have multiple risk factors for QTc interval prolongation, such as a family history of long QT syndrome or early sudden cardiac death or electrolyte depletion. Screening is also recommended when a cytochrome P450 inhibitor or other QTc interval–prolonging drug, including cocaine, is started.
- Recommendation 4 (Risk Stratification): For patients in whom the QTc interval is between 450 and 500 milliseconds, the potential risks and benefits should be discussed, and they should be monitored more frequently.
- If the QTc interval is greater than 500 milliseconds, discontinuing or decreasing the methadone dose should be considered, as well as eliminating other contributing factors such as drugs that cause hypokalemia. Use of an alternative therapy may be indicated.
- Recommendation 5 (Drug Interactions): Clinicians should be knowledgeable concerning interactions between methadone and other drugs that tend to prolong the QT interval or to slow the elimination of methadone.
Relevant Package Insert Statements
- Methadone’s pharmacokinetic properties, coupled with high interpatient variability in its absorption, metabolism, and relative analgesic potency, necessitate a cautious and highly individualized approach to prescribing. Particular vigilance is necessary during treatment initiation, during conversion from one opioid to another, and during dose titration.
- Optimal methadone initiation and dose titration strategies for the treatment of pain have not been determined. Published equianalgesic conversion ratios between methadone and other opioids are imprecise, providing at best, only population averages that cannot be applied consistently to all patients.
- It should be noted that many commonly cited equianalgesia tables only present relative analgesic potencies of single opioid doses in non-tolerant patients, thus greatly underestimating methadone’s analgesic potency, and its potential for adverse effects in repeated-dose settings.
- Regardless of the dose determination strategy employed, methadone is most safely initiated and titrated using small initial doses and gradual dose adjustments. As with all opioid drugs, it is necessary to adjust the dosing regimen for each patient individually, taking into account the patient’s prior analgesic treatment experience.
- Prescribers should always follow appropriate pain management principles of careful assessment and ongoing monitoring.
Navigation
Calculators
Tables
Articles

![]() NSAID Selection Calculator. Powerful tool to help select the most appropriate agent Methadone Dosing – Opioid conversions Morphine Equivalent Dose (MED) Calculator
NSAID Selection Calculator. Powerful tool to help select the most appropriate agent Methadone Dosing – Opioid conversions Morphine Equivalent Dose (MED) Calculator